Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Middle and Lower Respiratory Tract Infections
Lower Respiratory Tract Infection
LOWER RESPIRATORY TRACT INFECTION
Lower respiratory tract infection develops with invasion and disease of the lung, includ-ing the alveolar spaces and their supporting structure, the interstitium, and the terminal bronchioles. Bronchiolitis, an inflammatory process primarily affecting the small terminal airways in infants. Infection may occur by exten-sion of a middle respiratory tract infection, aspiration of pathogens past the upper airway defenses, or less commonly by hematogenous spread from a distant site such as an abscess or an infected heart valve. When infection develops through the respiratory tract, some compromise of the upper airway mechanisms for filtering or clearing inhaled infectious agents usually occurs. The most common are those that impair the epiglottic and cough reflexes, such as drugs, anesthesia, stroke, and alcohol abuse. Toxic inhalations and cigarette smoking may also interfere with the normal mucociliary action of the tracheobronchial tree. In healthy persons, the most common antecedent to lower respira-tory infection is infection of the middle respiratory structures (usually viral), allowing an otherwise innocuous aspiration of oropharyngeal flora to reach the lower tract and progress to disease rather than undergo rapid clearance. Some small infectious particles can accomplish airborne passage through the middle airway and bypass mucociliary defenses; if they can survive or multiply in alveolar macrophages, they may produce a primary infection. Examples include arthroconidia of Coccidioides immitis and cells of Mycobacterium tuberculosis and Bacillus anthracis.
CLINICAL FEATURES
Acute Pneumonia
Acute pneumonia is an infection of the lung parenchyma that develops over hours to days and, if untreated, runs a natural course lasting days to weeks. The onset may be gradual, with malaise and slowly increasing fever, or sudden, as with the bed-shaking chill associ-ated with the onset of pneumococcal pneumonia. The only early symptom referable to the lung may be cough, which is caused by bronchial irritation. In adults the cough becomes productive of sputum, which is purulent material generated in the alveoli and small air passages. In some cases the sputum may be blood streaked, rusty in color, or foul smelling. Labored or difficult breathing (dyspnea), rapid respiratory rate, and sometimes cyanosis are signs of increasing loss of alveolar air-exchange surface through spread of exudate. Chest pain from inflammatory involvement of the pleura is common. Physical signs on auscultation reflect the filling and eventual consolidation of alveoli by fluid and inflammatory cells.
The radiologic pattern of inflammatory changes in the lung is very useful in the diag-nosis of pneumonia and for clinical differentiation into likely etiologic categories. The most common pattern is patchy infiltrates related to multiple foci centering on small bronchi (bronchopneumonia), which may progress to a more uniform consolidation of one or more lobes (lobar pneumonia). A more delicate, diffuse, or “interstitial” pattern, which is also common, is particularly associated with viral pneumonia.
Chronic Pneumonia
Chronic pneumonia has a slow insidious onset that develops over weeks to months and may last for weeks or even years. The initial symptoms are the same as those of acute pneumonia (fever, chills, and malaise), but they develop more slowly. Cough can develop early or late in the illness. As the disease progresses, appetite and weight loss, insomnia, and night sweats are common. Cough and sputum production may be the first indication of a vague constitutional illness referable to the lung. Bloody sputum (hemoptysis), dysp-nea, and chest pain appear as the disease progresses. The physical findings and radiologic features can be similar to those of acute pneumonia, except that the diffuse interstitial in-filtrates of viral pneumonia are uncommon. There may be parenchymal destruction and the formation of abscesses or cavities communicating with the bronchial tree. The clinical features of chronic pneumonia may be due to a number of infectious agents or noninfec-tious causes such as neoplasms, vasculitis, allergic conditions, infarction, radiation or toxic injury, and diseases of unknown etiology (eg, sarcoidosis).
Pleural effusion is the transudation of fluid into the pleural space in response to aninflammatory process in adjacent lung parenchyma. It may result from a wide variety of causes, both infectious and noninfectious. Empyema is a purulent infection of the pleural space that develops when the infectious agent gains access by contiguous spread from an infected lung through a bronchopleural fistula or, less often, by extension of an abdominal infection through the diaphragm. Symptoms are usually insidious and related to the pri-mary infection until enough exudate is formed to produce symptoms referable to the chest wall or to compromise the function of the lung. The physical and radiologic findings are characteristic, with dullness to percussion and localized opacities on x-ray. In contrast to noninfectious effusions, empyema is frequently loculated.
Lung Abscess
Lung abscess is usually a complication of acute or chronic pneumonia caused by organisms that can cause localized destruction of lung parenchyma. It may occur as part of a chronic process or as an extension of an acute, destructive pneumonia, often after aspiration of oral or gastric contents. The symptoms of lung abscess, which are usually not specific, resemble those of chronic pneumonia or an acute pneumonia that has failed to resolve.
Persistent fever, cough, and the production of foul-smelling sputum are typical. Lung abscess can be diagnosed and localized with certainty only radiologically; it appears as a localized area of inflammation with single or multiple excavations or as a cavity with an air–fluid level. Multiple abscesses may develop as a result of blood-borne infection.
COMMON ETIOLOGIC AGENTS
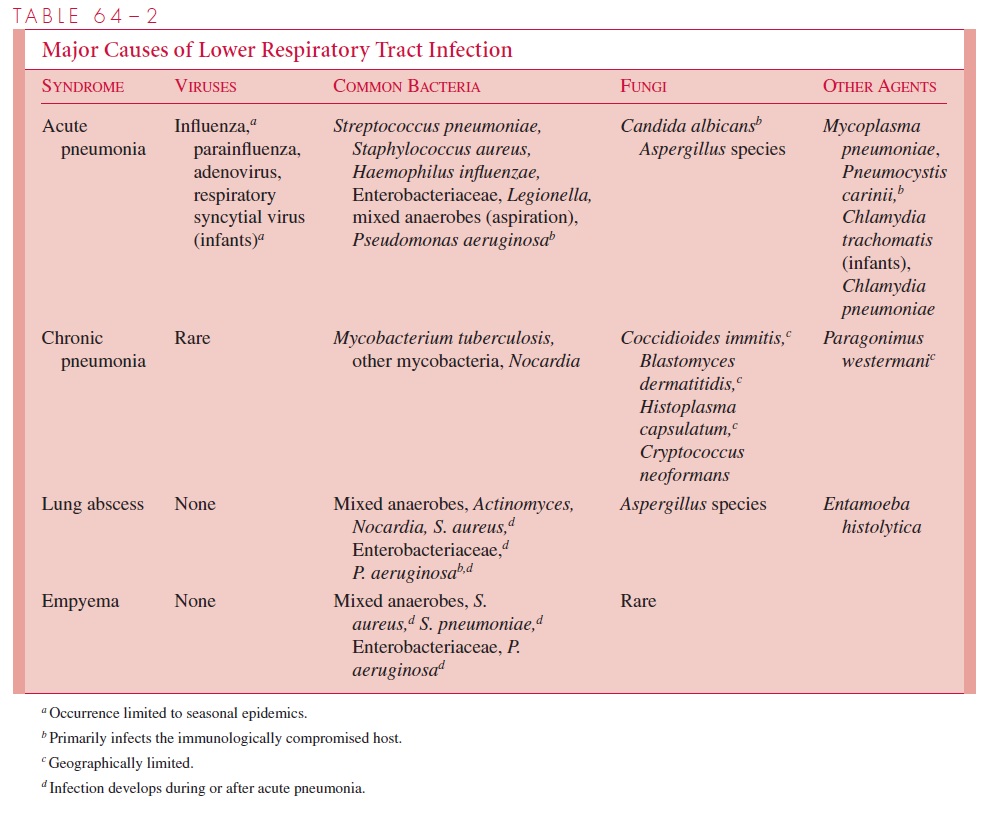
The infectious agents that most frequently cause lower respiratory infection are listed in Table 64 – 2. The etiology of acute pneumonia is strongly dependent on age. More than 80% of pneumonias in infants and children are caused by viruses, whereas less than 10 to 20% of pneumonias in adults are viral. The reasons are probably the same as those indi-cated previously for middle respiratory tract infections. Influenza and other viruses, however, may provide the initial predisposition toward bacterial infection.
Viruses are ex-tremely rare as a cause of chronic as opposed to acute lower respiratory tract infections, although some symptoms of the acute infection, such as cough, may persist for weeks until the bronchial damage has healed. Influenza virus is noteworthy as a cause of acute life-threatening pneumonia, even in previously healthy young adults. Pneumonia caused by bacteria such as enteric Gram-negative rods, Pseudomonas, andLegionella is primarily limited to patients with serious debilitating underlying disease or as a complication of hos-pitalization and its procedures (nosocomial infection). At any age, the pneumococcus is the most common bacterial cause of acute pneumonia, and Gram-negative infections other than Haemophilus are rare in children unless they have cystic fibrosis or immunodefi-ciency. Acute and subacute pneumonia may be due to Chlamydia; C. trachomatis is almost exclusively limited to infants less than 7 months of age, whereas C. pneumoniae com-monly affects school children and young adults, producing both bronchitis and pneumonia.
Lung abscess and empyema follow infections with the more destructive organisms or aspiration of mixed anaerobic flora from the oropharynx. Several clinical clues can sug-gest some of the etiologic agents, given a typical clinical syndrome. For example, Nocar-dia and mycobacteria, which are strict aerobes, tend to produce upper lobe infiltrates,whereas aspiration pneumonia caused by anaerobes tends to develop in the most depen-dent parts of the lung. Textbooks on infectious disease should be consulted for further de-tails regarding these features.
GENERAL DIAGNOSTIC APPROACHES
The degree of difficulty in establishing an etiologic diagnosis for a lower respiratory tract infection depends on the number of organisms produced in respiratory secretions, whether the causative species is normally found in the oropharyngeal flora, and how eas-ily it is grown. In the presence of typical clinical findings, the isolation of influenza virus from the throat or of M. tuberculosis from sputum is sufficient for diagnosis of influenza or tuberculosis, because these organisms are not normally found in such sites. The same cannot be said for S. pneumoniae and most bacterial pathogens, because they may be found in the throat in a significant number of healthy persons .
The examination of expectorated sputum has been the primary means of diagnosing the causes of bacterial pneumonia, but this approach has several advantages and disad-vantages. The advantages are ease of collection and absence of risk to the patient. The primary disadvantage is the confusion that results from contamination of the sputum with oropharyngeal flora in the process of expectoration and excessive contamination with saliva. Efforts have been unsuccessful to remove saliva from sputum by washing or to ac-complish interpretive differentiation of infective from normal flora by quantitative culture as with urine specimens . The quality of a sputum sample can be en-hanced by collection early in the morning (just after the patient arises), careful instruction of the patient, and occasionally by the use of saline aerosols (induced sputum) under the supervision of an inhalation therapy specialist. The worst results can be expected when the physician’s only involvement is writing an order, which is then passed down the ward chain of command to an orderly, who directs the patient to put his “sputum” in a cup placed at the bedside.
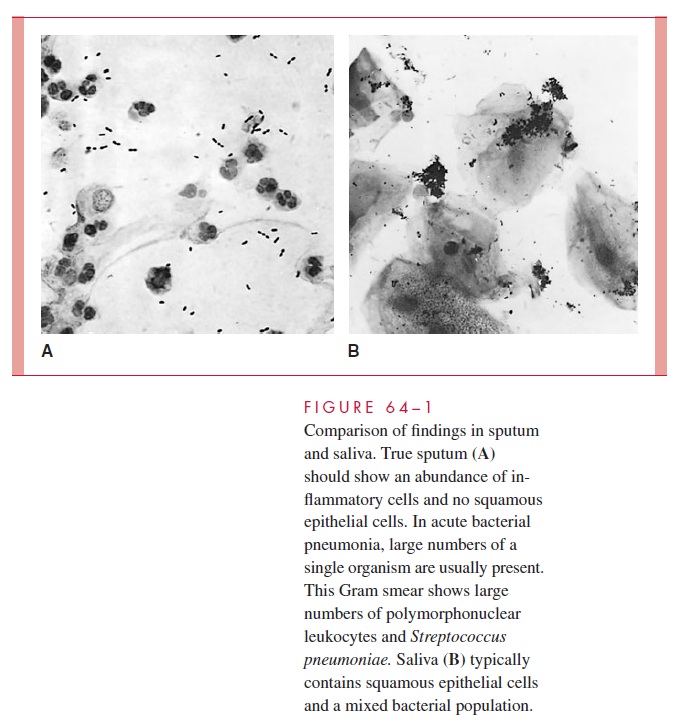
Microscopic examination before culture of direct Gram smears of specimens alleged to be sputum has proved useful. Polymorphonuclear leukocytes and large numbers of a single morphologic type of organism are typical findings in sputum from patients with bacterial pneumonia. Squamous epithelial cells from the oropharynx and a mixed bacter-ial population are characteristic of saliva (Fig 64 – 1). Unfortunately, most specimens are a mixture of both, which makes interpretation more difficult. Studies have shown that more than 10 to 25 squamous epithelial cells per low-power microscopic field are evidence of excessive salivary contamination, and such specimens should not be cultured because the results may be misleading. Thus, the direct Gram smear is crucial to the use of expecto-rated sputum for diagnosis of acute bacterial pneumonia. The smear may be useful in the absence of cultural results, but cultures are useless without a Gram smear to assess speci-men quality.
Another approach is to attempt a more direct collection from the lung using methods that bypass the oropharyngeal flora. This approach may be used in patients who are not producing sputum or in cases where analysis of expectorated sputum has been inconclu-sive. The major techniques include transtracheal aspiration, bronchoalveolar lavage (BAL), direct aspiration, and open biopsy. In transtracheal aspiration, an incision is made in the cricothyroid membrane and a catheter advanced deep into the tracheobronchial tree to aspirate sputum directly. This method is useful in diagnosis of both pneumonia and lung abscess. BAL is a modification of bronchoscopy in which the bronchi and alveoli are infused with saline, which is aspirated back through the bronchoscope.
Specimens obtained by BAL have been increasingly useful for demonstration of or-ganisms such as Pneumocystis carinii that were previously only seen in open lung biop-sies. Because BAL involves initial passage of the instrument through the upper airway, in-terpretation must take into account the possibility of some contamination with oropharyngeal secretions. Aspirates taken through tracheostomies or endotracheal tubes are of almost no value, because these sites become colonized with Gram-negative bacteria within hours of their implantation. Direct aspiration through the chest wall can be used for diagnosis of pneumonia or empyema if the involved area can be well localized and is at the lung periphery. In some cases an open lung biopsy is the only way to obtain diag-nostic material. Bacteremia may occur in acute pneumonia, particularly in its early stages. A blood culture should be part of the evaluation of every acute pneumonia. If posi-tive, it can confirm or overrule a diagnosis based on expectorated sputum culture.
Once an appropriate specimen is obtained, diagnosis is usually readily made by cul-ture and in the sections on the individual etio-logic agents. Only specimens collected by one of the invasive techniques should be used for anaerobic culture, because expectorated sputum is invariably contaminated with oropharyngeal anaerobes and results are meaningless.
GENERAL PRINCIPLES OF MANAGEMENT
The general principles of management of lower respiratory tract infections are similar to those of middle tract infections. Drainage or surgical measures are needed more often as adjuncts to antimicrobial therapy in cases of chronic pneumonia, lung abscess, and empyema. When bacterial infection is considered, empirical therapy is usually given until the results of cultures and antimicrobial susceptibility tests are available. Treatment may vary from penicillin alone for a previously healthy individual in whom the most reason-able nonviral possibility is S. pneumoniae, to multiple drugs for a debilitated or immuno-compromised patient, in whom the possibilities are much broader.
Related Topics