Chapter: Essentials of Psychiatry: Psychosocial Rehabilitation
Issues in the Design of Psychosocial Interventions
Issues
in the Design of Psychosocial Interventions
The
potential benefits of psychosocial treatment are often not achieved in the
community due to poor understanding of the spe-cial needs and liabilities of
schizophrenia patients. Five factors need to be taken into account when
implementing psychosocial interventions and evaluating the results: 1) timing
and duration of treatment; 2) individual differences in treatment needs; 3) the
role of the patient in treatment; 4) the limitations imposed by impairments in
information processing; and 5) the need to base interventions on a compensatory
model.
Timing and Duration of Treatment
The APA Practice Guidelines for the Treatment of
Patients with Schizophrenia makes a number of important points that are
germane to rehabilitation programming, not the least of which pertains to the
need for multimodal, long-term care: “Schizophrenia is a chronic condition that
frequently has devastating effects on many aspects of the patient’s life and
carries a high risk of suicide and other life-threatening conditions. The care
of most patients involves multiple efforts to reduce the frequency and severity
of episodes and to reduce the overall morbidity and mortality of the disorder.
Many patients require comprehensive and continuous care over the course of
their lives with no limits as to duration of treatment”. This guideline is
widely reflected in case management and pharmacotherapy but has not been
adequately addressed in rehabilitation programs.
The role
for psychosocial treatment and rehabilitation in-creases as the patient becomes
more stable and shifts from support and stress reduction to specific
rehabilitation strategies such as social skills training and cognitive rehabilitation.
This three stage model and associated treatment emphasis has good face
validity.
Treatment
planning must be individualized. While this might seem like a given, many
outpatient treatment systems are designed with a one-size-fits-all model, in which most patients are assigned to a
standard set of group treatments paired with case management. This is a
strategy that maximizes dropouts and minimizes effec-tiveness. This is a
population that is difficult to treat effectively under the best of
circumstances. Positive outcomes are likely only if both the content of
treatment and the format of treatment are tai-lored to the individual patient’s
needs and learning capacities.
The
combination of psychosis, thought disorganization and negative symptoms
(especially anergia, apathy and anhedonia) often lead to the false assumption
that patients are not capable of being active participants in their own
treatment. Indeed, many patients seem unmotivated and are noncompliant, but
such seeming disinterest and passivity should not be interpreted as accurate
reflections of the person’s goals and desires or as immutable traits. Negative
symptoms are not always stable, and they may be secondary to demoralization,
psychotic symptoms, medication side effects and other factors that vary over
time (Carpenter et al., 1988;
McGlashan and Fenton, 1992). Paul and Lentz (1977) have shown that even
extremely withdrawn, chronic schizophrenia patients can be motivated by a
systematic incentive program. Similarly, desire to change and inclination to do
the work required for treatment also vary over time in the same way that
motivation to lose weight or quit smoking varies in nonpatient populations.
As
cogently argued by Strauss (1989), schizophrenia pa-tients have an active
“will”. Much of their behavior is goal di-rected and reflects an attempt to
cope with the illness as best they can. Consequently, it is essential to view
the patient as a potentially active partner and involve him or her in goal
setting and treatment planning. Too often, treatments are imposed on patients
by the treatment team and family members, with little consideration of the
patient’s own desires or capacities. It should not be surprising in such
circumstances if the patient fails to adhere to treatment recommendations,
increasing the risk of re-lapse and creating tensions in relationships with
family members and treatment providers. To be sure, engaging the patient to
es-tablish treatment goals can be a long, arduous process, but failure to do so
courts the larger risk of undermining the very purpose of the intervention.
Impairments in Information Processing
It is now
well established that impaired information process-ing represents one of the
most significant areas of dysfunction in schizophrenia. The illness is marked
by neuropsychological deficits in multiple domains, including verbal memory,
work-ing memory, attention, speed of processing, abstract reasoning and
sensorimotor integration (Braff, 1991; Green and Nuech-terlein, 1999). These
deficits are highly related to social func-tioning and role performance in the
community, as well as to performance in skills training programs (Green, 1996;
Green et al., 2000).
A related
issue concerns the impact of neurocognitive defi-cits on the generalization of
treatment effects. A basic assumption of all psychotherapies is that skills
acquired in treatment sessions must be transferred or generalized to the
patient’s natural envi-ronment. Yet, such generalization is contingent upon
cognitive processes that are often disrupted in schizophrenia, especially
“executive functions” mediated by the dorsolateral prefrontal cortex
(Weinberger, 1987).
Unfortunately,
clinical rehabilitation programs have lagged behind the experimental literature
in this arena and neu-rocognitive deficits generally are not well addressed in
a system-atic manner.
Adoption of a Compensatory Model
A
rehabilitation model is more appropriate for treatment of most patients with
schizphrenia than the standard treatment model as: 1) it implies a narrower
focus on specific skills and behaviors, and 2) it aims to improve functioning
in specific areas, rather than eliminating or curing an entire condition. As
indicated above, cognitive impairment is a central feature of the disorder,
evident in childhood and progressing sharply with the onset of psychotic
illness. It is reasonable to speculate that the impairments observed in ill
adult patients are at least of two types: 1) those present from early in
development; and 2) those that are related to clinical psychotic illness. The
existence of such early, developmentally based impairments suggest that the
concept of “premorbid” functioning in schizophrenia may no longer be tenable;
rather, there is a prepsychotic period during which there is subtle evidence of
the “morbid” process. Thus, the challenge confronting attempts at cognitive
enhancement may not be restoration of function, but instead may be the
development of critical competencies and strategies for coping with deficits.
Consistent
with this hypothesis, a compensatory approach to treatment may be more
appropriate than the restorative or reparative approach characteristic of most
treatment programs. Cognitive adaptation training (CAT) is a creative
compensatory approach developed by Velligan and colleagues (2000). Case
managers provide patients with home-based, compensatory en-vironmental
strategies to help structure the patient’s living en-vironment which maximizes
the likelihood that she/he can com-plete requisite activities of daily living.
Examples include posting reminders about appointments on the exit door from the
apart-ment, listing items of clothing to be worn on the closet door, and
placing
medications in a location that makes it maximally likely that the patient will
see it and be reminded to take it. Prompts and other environmental aides are
individually tailored to the pa-tients’ level of apathy, disinhibition and
executive dysfunction. CAT can be administered in a time limited fashion, but
may be a lifelong service for severely impaired patients. Velligan and
colleagues found 9-months of CAT to be superior to an atten-tion placebo and
standard outpatient care on positive symptoms, negative symptoms, motivation,
community functioning, global functioning and incidence of rehospitalization.
This is an excel-lent model for compensatory interventions, and warrants
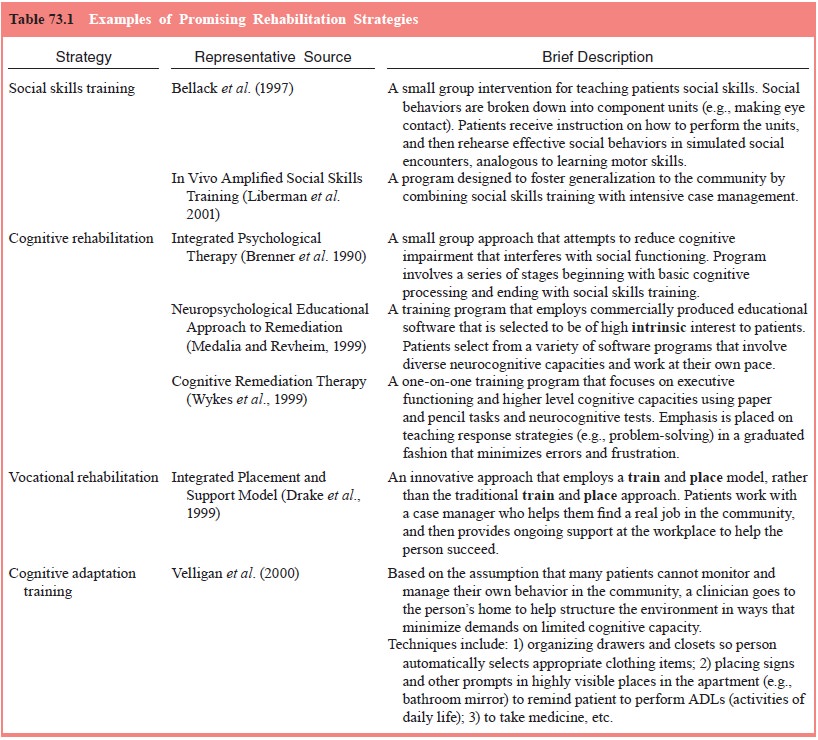
further study (Table 73.1).
Related Topics