Chapter: Obstetrics and Gynecology: Immediate Care of the Newborn
Initial Care of the Well Newborn
INITIAL CARE OF THE WELL NEWBORN
Delivery Room Assessment
In accordance with the American
Heart Association (AHA) and the American Academy of Pediatrics (AAP), at least
one person skilled in neonatal assessment and resuscitation should be available
at every delivery to care for the newborn.
Every
delivering physician should be familiar with the ini-tial assessment,
resuscitation, and care of a newborn infant.
Immediately following delivery,
the newborn infant should first be assessed to decide whether resuscitation is
necessary. Four characteristics define a newborn who requires no additional
resuscitation:
·
A full-term infant
·
Clear amniotic fluid with no
evidence of meconium and infection
·
Spontaneous breathing and crying
·
Good muscle tone
In an effort to predict which
newborns will require more intensive resuscitation, the gestational age should
be esti-mated as accurately as possible prior to delivery. This allows the
appropriate neonatal team to be present and prepared for resuscitation. It is
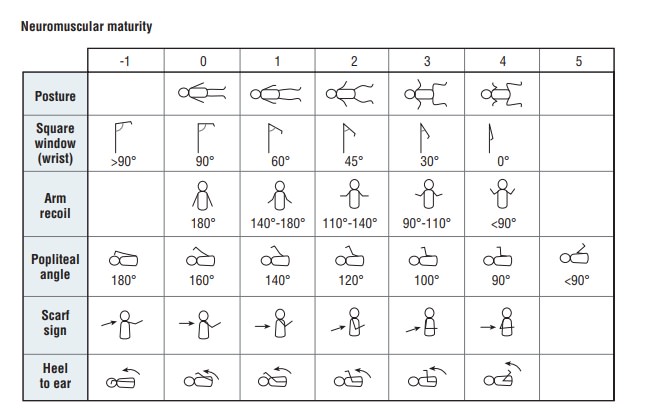
also possible to assess the infant after delivery using the Ballard scoring system, which evaluates
neuromuscular and physical maturity (Fig. 10.1).
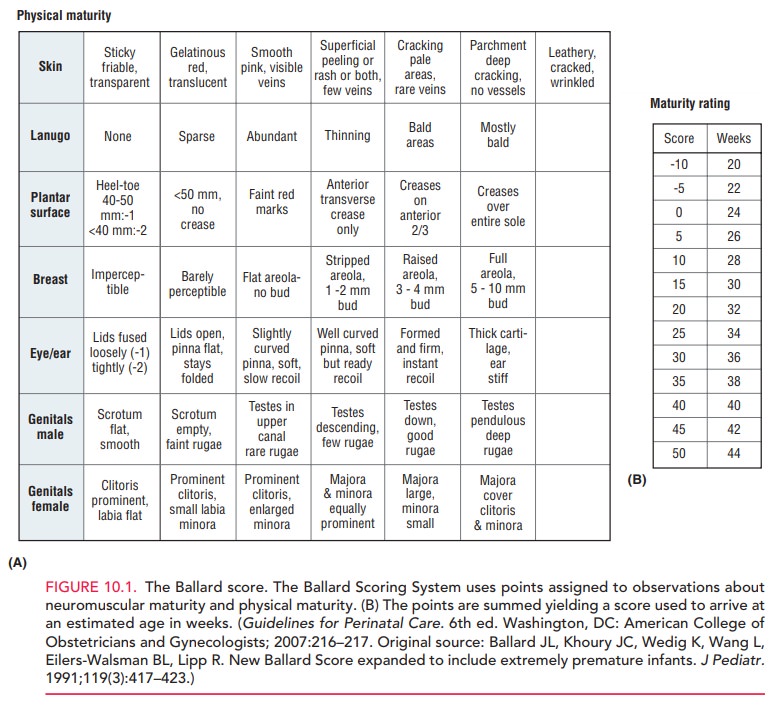
The Apgar Scoring system is commonly used as an objective means to
assess the newborn’s condition (Table 10.1). Five signs are given scores of 0,
1, or 2, for a total of up to 10. Scores are assigned at 1 and 5 minutes, and
at every 5 minutes until 20 minutes thereafter, if the 5-minute Apgar score is
less than 7. Although these continued assess-ments are not part of the original
Apgar scoring system, many clinicians find them to be of value in evaluating
how an infant is responding to resuscitation. An Apgar score of 7 to 10 is indicative
of an infant who requires no active resuscitative intervention; a score of 4 to
7 is considered indicative of a mildly to moderately depressed infant; and a
score of less than 4 is suggestive of a severely depressed infant who requires
immediate resuscitative efforts.
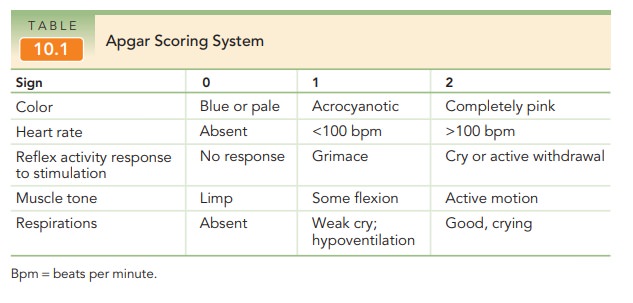
The Apgar
score should not be used to define birth asphyxia, because it is not designed
to do so and, indeed, does not pro-vide such information.
Likewise, the Apgar score cannot be used to identify the causes of the newborn illness. In general, a low 1-minute Apgar score identifies the newborn who requires particu-lar attention. The 5-minute Apgar score can be used to evaluate the effectiveness of any resuscitative efforts that have been undertaken, or to identify an infant who needs more evaluation and management. It should not be used to predict neurologic outcome in term infants.
Routine Care
Basic routine care is necessary
for all newborn infants, regardless of the need for resuscitative efforts. For
infants who do not require resuscitation at birth, routine care is performed
immediately following delivery.
First, the newborn infant is
thoroughly dried to main-tain appropriate body temperature. Warm blankets,
skin-to-skin contact with the mother, or a radiant warmer can all accomplish
this task.
For
healthy, vigorous, term neonates, skin-to-skin contact promotes maternal–infant
bonding and initiation of breast-feeding in the first hour or life.
Premature infants have more
difficulty maintaining their body temperature and are more susceptible to cold
stress. These infants require warming pads, heated towels, and a preheated
radiant warmer to stay warm.
Second, after the umbilical cord is clamped and cut, it
is left exposed to air to facilitate drying and separation. Local application
of antimicrobial agents (e.g., triple-dye, iodophor ointment, hexachlorophene
powder) is com-mon. The umbilical cord loses its bluish-white appearance within
the first 24 hours after delivery. After a few days, the blackened, dried stump
sloughs, leaving a granulating wound. If cord blood banking has been requested,
the sample should be obtained and stored at this time.
Another essential component of
routine care is the assessment of vital signs. An infant’s temperature, heart
and respiratory rate, core and peripheral color, level of alertness, tone, and
activity should be monitored at deliv-ery and every 30 minutes thereafter until
these measures are stable for at least 2 hours.
If the mother plans to
breastfeed, the newborn should be placed at the breast in the delivery room
within the first hour after delivery. In general, healthy neonates should
remain with their mothers.
Related Topics