Chapter: Obstetrics and Gynecology: Immediate Care of the Newborn
Initial Care of the Ill Newborn
INITIAL CARE OF THE ILL NEWBORN
Although most deliveries are
uncomplicated, requiring only basic neonatal care, resuscitation may be necessary in up to 10% of all deliveries; 1%
of these require major resuscitative efforts. The need for these efforts increases
in circumstances such as premature birth, low–birth-weight infants, prolonged
labor, and non-reassuring measures of fetal well-being. Not all deliveries
occur in a setting with intensive pediatric care immediately available. In the
absence of such staff and facilities, maternal transport to a facility with a
greater capacity to provide appropriate care should be attempted before
delivery. Alternatively, the transport of a neonatal team from a tertiary care
center to the primary care site is an option.
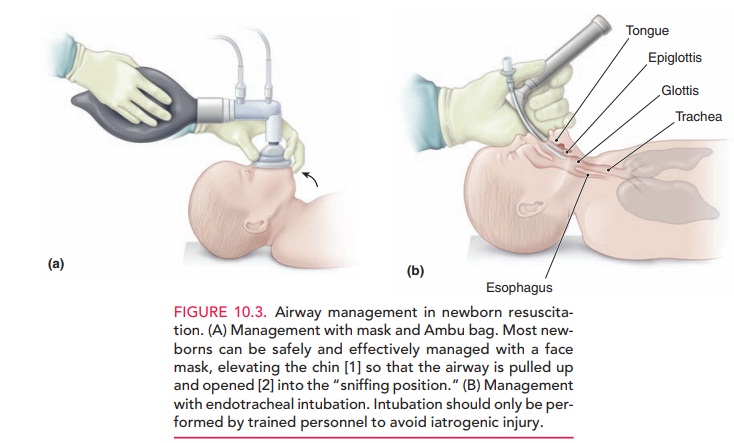
Neonatal Resuscitation
The normal newborn breathes
within seconds of delivery and usually has established regular respirations
within 1 minute of delivery. If the neonate is having difficulty breathing,
ventilation, chest compression, and epineph-rine should be instituted, as shown
in the protocol in Figure 10-2. If an infant does not respond to epinephrine,
hypovolemic shock should be considered, especially if there is evidence of
blood loss. In this case, intravenous normal
saline at 10 mL/kg should be given.
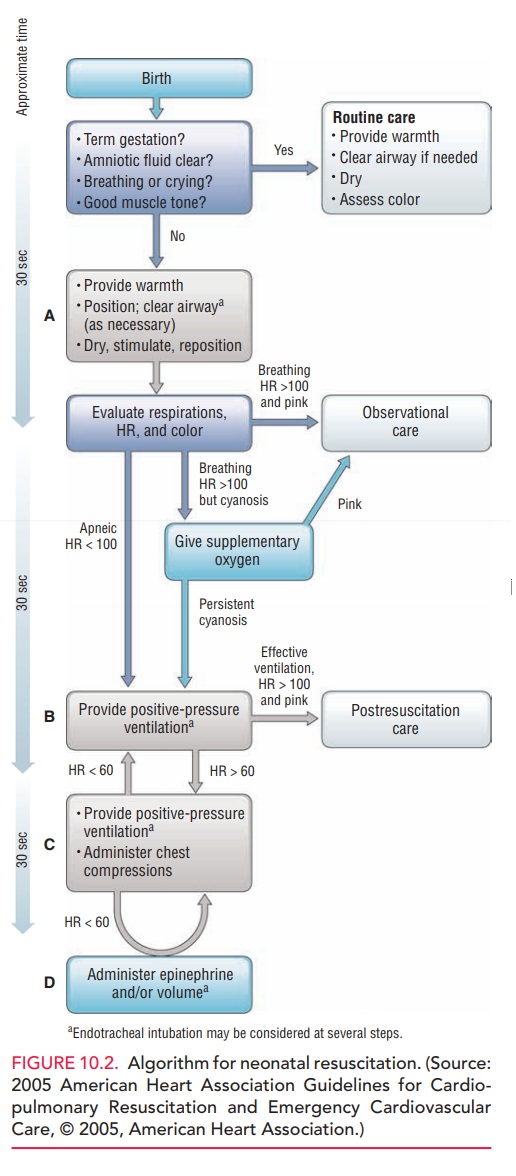
The same principles of adult resuscitation (airway, breath-ing, and circulation) apply to neonatal resuscitation (Figure10.3). First, the newborn is transported to a radiant warm-ing unit to be thoroughly dried. When drying the infant, it is important to remove wet towels to minimize the effect of evaporation that would otherwise lead to a rapid drop in core body temperature. The nose and oropharynx are suc-tioned to ensure an open airway as the infant is placed in the supine position.
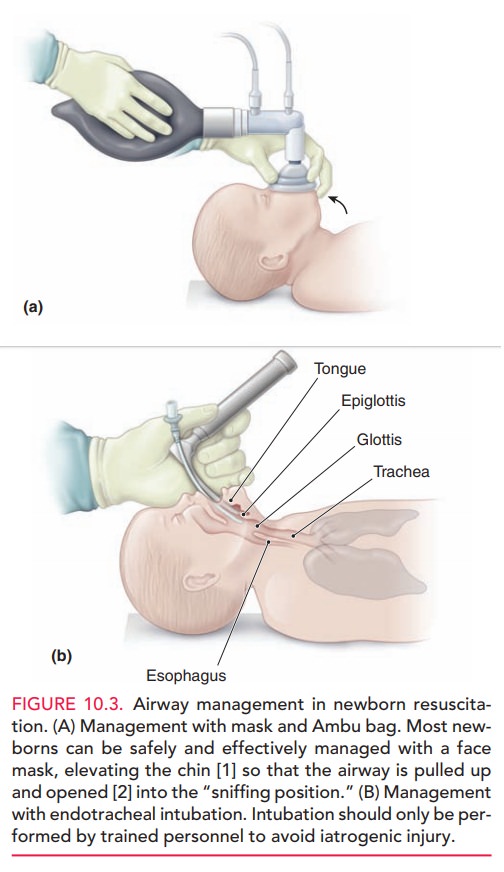
The head should be positioned with the neck slightly extended—the “sniffing position”—to allow for maximal air entry. Drying and suctioning, along with providing mild stimulation by rubbing the back or soles of the feet—or flicking the soles of the feet—help to stimulate the infant to breathe and cry.
Respiratory distress may occur as
a consequence of maternal narcotic administration during labor. A narcoticantagonist can be considered
only if severe respiratory pres-sure ventilation has improved the heart rate
and color, and the mother received narcotics within 4 hours of delivery.
In
infants born to a narcotic-addicted mother, naloxone iscontraindicated because the immediate withdrawal
symp-tom that ensues can be life-threatening.
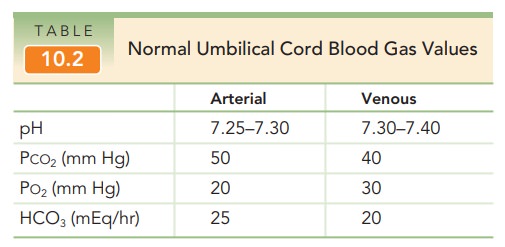
Umbilical Cord Blood Gases
During the resuscitation process,
the metabolic well-being of an ill newborn is most accurately assessed using umbil-ical cord blood gases. Cord blood
gases should be obtainedin cases of cesarean delivery for fetal compromise, a
low 5-minute Apgar score, severe growth restriction, abnormal fetal heart rate
tracing, maternal thyroid disease, intra partum fever, and multifetal
gestations. A segment of umbilical cord is double-clamped and cut and placed on
the delivery table pending assessment of the 5-minute Apgar score, so that it
may be taken for assessment of pH, PO2, PCO2, HCO3,
and base deficit. It should be remem-bered that, in the fetus, freshly
oxygenated blood from the placenta travels to the fetus through the umbilical
vein, and blood metabolized by the fetus travels back to the placenta through
two umbilical arteries. The most
meaningful assess-ment of metabolic status of the infant at the time of
delivery is through analysis of umbilical artery blood gases. Analysis
ofpaired arterial and venous specimens should prevent debate over whether a
true arterial specimen was obtained. There-fore, where possible, obtaining both
venous and arterial samples (paired specimen) is recommended. Normal val-ues
for umbilical arterial and venous samples are given in Table 10.2.
Acidemia is
generally accepted as an increase inhydrogen ion concentration in an umbilical
arterial sam-ple resulting in a pH of <7.20. Fetal asphyxia is defined as a condition of impaired blood gas
exchange leading to progressive hypoxemia and hypercapnia with a significant
metabolic acidosis (base deficit >=12 mmol/L).
The base
deficit can be used to predict metabolic acidosis sig-nificant enough to cause
newborn complications.
Ten percent of newborns with a
base deficit of 12 to 16 mmol/L and 40% of newborns with a base deficit of
>16 mmol/L will have moderate to severe complications, such as newborn
encephalopathy and cardiovascular and respiratory complications. The terms acidemia, acidosis, andasphyxia
should be used carefully when applied to the newborn condition, because each
term defines a series of changes that may or may not represent true metabolic
compromise.
Umbilical Cord Blood Banking
Umbilical cord blood is now known to contain potentially life-saving hematopoietic stem cells for possible adult trans-plant for the correction of inborn errors of metabolism, hematopoietic malignancies, and genetic disorders of the blood and immune system. If a patient requests information on umbilical cord banking, balanced and accurate informa-tion regarding the advantages and disadvantages of public or private banking should be provided.
The remote chance ofan autologous unit of umbilical cord blood being
used for a child or a family member (approximately 1 in 2700 individuals)
should also be disclosed.
Related Topics