Chapter: Pathology: Respiratory Pathology
Infiltrative Restrictive Lung Diseases(Diffuse Interstitial Diseases)
INFILTRATIVE RESTRICTIVE LUNG DISEASES(DIFFUSE INTERSTITIAL
DISEASES)
Acute
respiratory distress syndrome (ARDS) refers to
diffuse damage of alveolarepithelium and capillaries, resulting in progressive
respiratory failure that is unre-sponsive to oxygen treatment. Clinicians use
the term ARDS, while pathologists use
the term diffuse alveolar damage (DAD)
to describe the pathologic changes.
ARDS
may be caused by shock, sepsis, trauma, gastric aspiration, radiation, oxygen
toxicity, drugs, or pulmonary infection. Activated neutrophils mediate cell
damage. Clinically, patients show dyspnea, tachypnea, hypoxemia, cyanosis, and
use of acces-sory respiratory muscles. X-rays show bilateral lung opacity
(“white out”).
On
gross pathologic examination affected lungs are heavy, stiff, and
noncompli-ant. Microscopically, there is intra-alveolar edema, and hyaline
membranes line the alveolar spaces. In resolving cases there is proliferation
of type II pneumocytes and interstitial inflammation and fibrosis.
Treatment
is based on treating the underlying cause and on supporting respiration with
mechanical ventilation. The prognosis is problematic even with good care, with
overall mortality 40%.
Respiratory
distress syndrome of the newborn (hyaline membrane
disease of new-borns) is caused by a deficiency of surfactant. It is associated
with prematurity (gestational age of <28 weeks has a 60% incidence),
maternal diabetes, multiple births, male gender, and cesarean section delivery.
Clinically, infants are normal at birth but within a few hours develop
increasing respiratory effort, tachypnea, nasal flaring, use of accessory
muscles of respiration, an expiratory grunt, and cyanosis. Chest radiograph may
demonstrate bilateral “ground- glass” reticulogranular densi-ties. Autopsy
findings include atelectasis and hyaline membranes.
Treatment
is surfactant replacement, mechanical ventilation, and continuous posi-tive
airway pressure (CPAP). Respiratory distress syndrome of the newborn can
sometimes be prevented if labor can be delayed and if corticosteroids are used
to mature the lung. With improved therapies, now >90% of babies survive.
Chronic
interstitial lung disease is a term describing heterogeneous
lung disorderswhich share similar symptomology but vary in prognosis. Patients
present with dys-pnea and cough. Lung biopsy findings can be paired with
clinical information to aid in therapeutic management/palliative care.
·
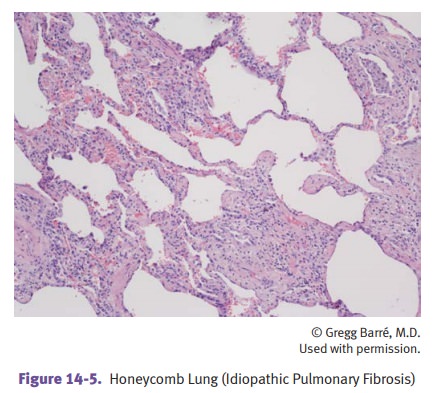
Idiopathic pulmonary fibrosis (IPF) is
a fatal disease. It shows patchy intersti-tial fibrosis and inflammation.
“Honeycomb fibrosis” refers to dilated cystic spaces lined with type II
pneumocytes; this histology is consistent with end-stage lung. Pathologists use
the term usual interstitial pneumonia
for IPF.
·
Nonspecific interstitial pneumonia has
a better prognosis than IPF. There is acellular pattern and a fibrosing
pattern.
·
Cryptogenic organizing pneumonia responds
to steroids. Histologically, thereare plugs of connective tissue inside the
alveolar spaces.
·
Collagen vascular disease pneumonitis has
varied patterns of parenchymaland pleural involvement. The prognosis is poor.
·
Smoking-related pneumonitis.Several
entities have been identified.
o
Desquamative interstitial pneumonia
features alveolar macrophages.
o
Respiratory bronchiolitis features
bronchiolocentric macrophages.
o
Smoking-related interstitial
fibrosis shows septal collagen deposition without significant associated
inflammation.
·
Hypersensitivity pneumonitis.After
exposure to a sensitizing agent such asmoldy hay, patients present with a
febrile acute reaction or a chronic disease with weight loss. Biopsy shows
peribronchiolar acute and chronic interstitial inflam-mation +/- noncaseating
granulomas. The disease is immunologically mediated.
Eosinophilic pneumonia describes
a group of diseases with varying clinicalfeatures but a common histologic
finding of a mixed septal inflammatory infiltrate and eosinophils within
alveolar spaces. Loeffler’s syndrome
is a self-limiting type of eosinophilic pneumonia with peripheral blood eosinophilia.
Occupation-associated
pneumoconiosis is a common cause of chronic interstitiallung disease. It is
considered separately here to show the full spectrum of disease since neoplasia
may occur during its course.
·
Pneumoconioses are fibrosing pulmonary diseases
caused by inhalation of anaerosol (mineral dusts, particles, vapors, or fumes).
Key factors affecting their development include the type of aerosol and its
ability to stimulate fibrosis; the dose and duration of exposure; and the size
of the particle, with only particles <10 microns entering the alveolar sac.
Coal
worker’s pneumoconiosis is an important pneumoconiosis that
isdue to anthracosis, in which carbon pigment (anthracotic
pigment) fromcoal mining accumulates in macrophages along the pleural
lymphaticsand interstitium. Clinically, the disease may progress through
severalstages. The earliest stage is asymptomatic.
Simple
coal worker’s pneumoconiosis (black lung disease) is character- ized
by coal-dust macules and nodules in the upper lobes that producelittle
pulmonary dysfunction.
Complicated
coal worker’s pneumoconiosis is characterized by progres-sive
massive fibrosis that is accompanied by increasing respiratory dis- tress,
secondary pulmonary hypertension, and cor pulmonale.
Caplan
syndrome is the term when pneumoconiosis (of any type) accom- panies
rheumatoid arthritis.
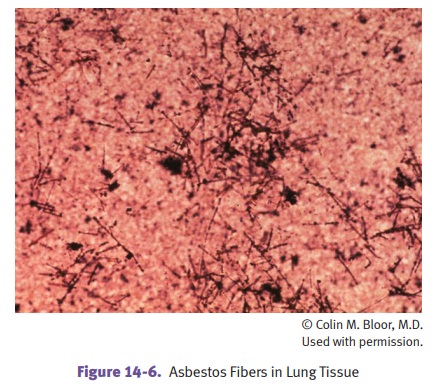
· Asbestosis
is caused by members of a family of crystalline silicates.
Occupa-tions in which asbestos exposure may occur include shipyard work,
insulation and construction industries, brake-lining manufacture.
Serpentine
asbestos is composed of curved, flexible fibers, with the most
common type of serpentine asbestos being chrysotile.
Amphibole
asbestos is composed of straight, brittle fibers. Important types
include crocidolite, tremolite, and amosite. Amphibole asbestos is more
pathogenic than serpentine asbestos, and is highly associated with
mesotheliomas.
The
pulmonary pathology of asbestosis is a diffuse interstitial fibrosis
that begins in the lower lobes; it causes slowly progressive dyspnea which may
eventually be complicated by secondary pulmonary hypertension and cor
pulmonale. Pulmonary biopsy may demonstrate asbestos bodies that have become
coated with iron (ferruginous bodies). Otherwise, the findings are the same as
usual interstitial pneumonia.
Pleural
involvement may take the form of parietal pleural plaques (acel- lular
type I collagen deposition) in a symmetrical distribution involving the domes
of the diaphragm and posterolateral chest walls on chest x-ray.
The
apices and costophrenic angles are spared. Plaques on the anterior chest wall
may be seen on CT. Fibrous pleural adhesions may occur on the visceral pleura.
Lung
cancer is the most common tumor in asbestos-exposed individu- als;
there is a strong synergistic effect between smoking and asbestos exposure.
Malignant
mesothelioma is a rare, highly malignant neoplasm associ- ated with
occupational exposure to asbestos in 90% of cases. It presents with recurrent
pleural effusions, dyspnea, and chest pain. The tumor grossly encases and
compresses the lung; microscopic exam exhibits car- cinomatous and sarcomatous
elements (biphasic pattern), while electron microscopy shows long, thin
microvilli on some tumor cells. The prog- nosis of mesothelioma is poor. Other problems
include increased risk of laryngeal, stomach, and colon cancers. Family members
also have increased risk of cancer due to the worker bringing home clothing
cov- ered with asbestos fibers.
· Silicosis
is due to exposure to silicon dioxide (silica). It is seen
most frequentlywith occupational exposure (sandblasters, metal grinders,
miners). The pul-monary pathology shows
dense nodular fibrosis of the upper lobes whichmay progress to massive
fibrosis; birefringent silica particles can be seen with polarized light.
Patients
present with insidious onset of dyspnea that is slowly progressive despite
cessation of exposure. X-ray shows fibrotic nodules in the upper zones of the
lungs. There is an increased risk of TB.
·
Berylliosis is an allergic granulomatous
reaction due to workplace exposureto beryllium in the nuclear, electronics, and
aerospace industries. Genetic susceptibility appears to play a role, as does a
type IV hypersensitivity reac-tion, resulting in granuloma formation.
Clinically, acute exposure causes acute pneumonitis, while chronic exposure
causes pulmonary noncaseating granu-lomas and fibrosis, hilar lymph node
granulomas, and systemic granulomas
Related Topics