Chapter: Clinical Anesthesiology: Clinical Pharmacology: Hypotensive Agents
Hypotensive Agents
Hypotensive Agents
A multitude of drugs are capable of
lowering blood pressure, including volatile anesthetics, sympathetic
antagonists and agonists, calcium channel block-ers, β-blockers, and
angiotensin-converting enzyme inhibitors.
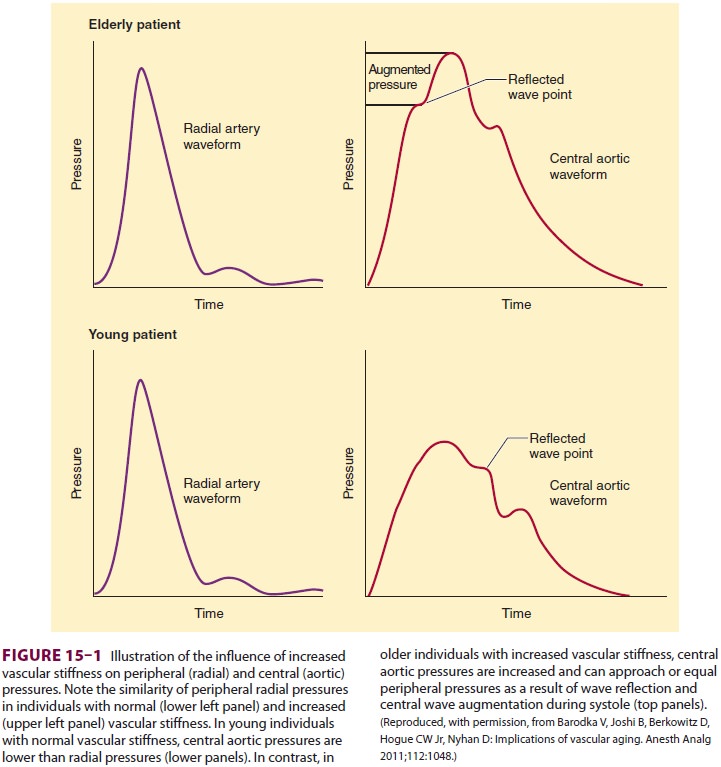
In patients with “older” vasculature,
the wave arrives sooner, being conducted back by the noncompli-ant vasculature
during late systole, which causes an increase in cardiac workload and a
decrease in dia-stolic pressure (Figure 15–1). Thus, older patientsdevelop
increased systolic pressure and decreased diastolic pressure.
Widened pulse pressures (the difference
between systolic and diastolic pressures) have been associated with both
increased incidence of postop-erative renal dysfunction and increased risk of
cere-bral events in patients undergoing coronary bypass
surgery. Consequently, control of blood
pressure is essential to mitigate postoperative morbidity, espe-cially as
patients of advanced vascular age present for surgery.
β-Blocker therapy should be maintained
peri-operatively in patients who are being treated with β-blockers as a part of
their routine medical regimen. Furthermore, according to the American College
of Cardiology, β-blockers are also of potential benefit to patients with more
than one cardiac risk factor, espe-cially those who are undergoing vascular
surgery. However, the routine administration of high-dose β-blocker therapy
may, in the absence of dose titra-tion, be harmful in patients not taking
β-blockers. The American College of Cardiology/American Heart Association guidelines
for β-blocker use peri-operatively should be closely followed. Adherence to
such guidelines is used by third parties as a “quality” performance indicator
for anesthesia delivery. Thus, anesthesia providers should periodically review
recommendations regarding β-blocker therapy, as guidelines evolve as new
evidence becomes available and older evidence is refuted. β-Blockers (esmolol,
metoprolol, and others) were previously discussed for the treatment of
transient perioperative hyper-tension and are routinely used by anesthesia
provid-ers.
Along with increased vascular age,
diastolic dysfunction is often underestimated in patients, as it can present in
individuals with preserved sys-tolic function. Acute diastolic heart failure
can develop in the perioperative period secondary to hypertensive crisis.
Diastolic dysfunction occurs due to the inability of the heart to relax
effectively. Failure to actively sequester calcium ion into the sarcoplasmic
reticulum (an energy-dependent process) impedes relaxation. Acute hypertension
can produce diastolic dysfunction perioperatively, leading to elevated left
ventricular end-diastolic pressures, myocardial ischemia, and pulmonary edema.
Consequently, as increasing numbers of patients have diastolic dysfunction, tight
control of blood pressure perioperatively is essential for safe anesthetic
practice.
Blood pressure is essentially the
product of car-diac output and systemic vascular resistance. Agents that lower
blood pressure either reduce the force of myocardial contraction and/or produce
vasodilata-tion of the arterial and venous capacitance vessels. Agents used to
lower blood pressure include nitro-vasodilators, calcium antagonists, dopamine
ago-nists, anesthetic agents, and angiotensin-converting enzyme inhibitors.
β-Blockers have been previously discussed.
Related Topics