Chapter: Obstetrics and Gynecology: Hypertension in Pregnancy
Hypertension in Pregnancy: Pathophysiology
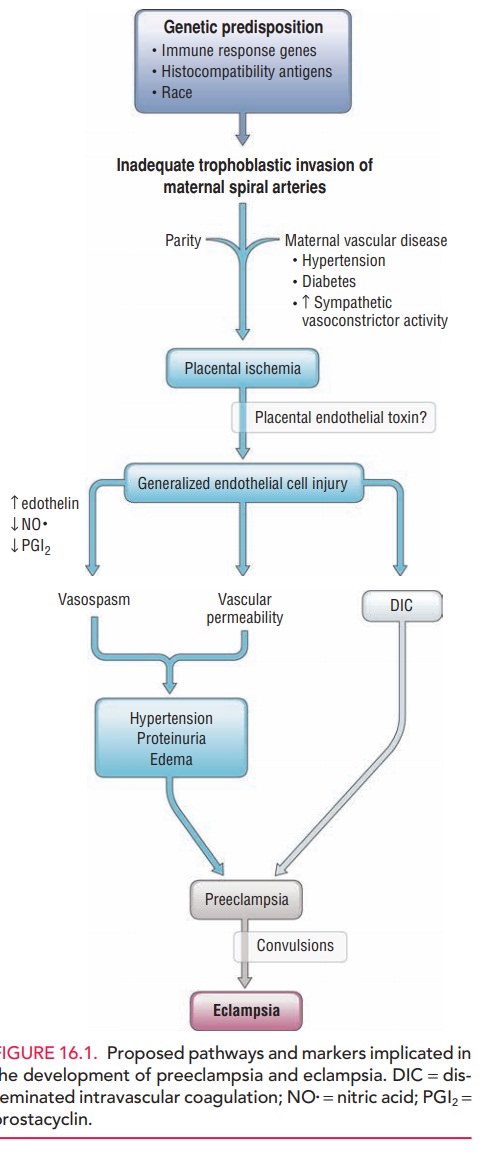
PATHOPHYSIOLOGY
Hypertension in pregnancy affects
the mother and new-born to varying degrees. Given the characteristic
multi-system effects, it is clear that several pathophysiologic mechanisms are
involved (Fig. 16.1). The predominant
patho-physiologic finding in preeclampsia and gestational hypertension is maternal vasospasm.Several
potential causes for mater-nal vasospasm have been postulated:
·
Vascular
changes: Instead of noting the
physiologictrophoblast-mediated vascular changes in the uterine vessels
(decreased musculature in the spiral arterioles leads to the development of a
low-resistance, low-pressure, high-flow system), inadequate maternal vas-cular
response is seen in cases of preeclampsia and/or intrauterine fetal growth
restriction. Endothelial dam-age is also noted within the vessels.
·
Hemostatic
changes: Increased platelet activationwith increased
consumption in the microvasculature is noted during the course of preeclampsia.
Endothelial fibronectin levels are increased and antithrombin III and α2-antiplasmin
levels are decreased, reflecting en-dothelial damage. Low antithrombin III
levels are per-missive for microthrombi development. Endothelial damage is then
thought to promote further vasospasm.
· Changes in prostanoids: Prostacyclin (PGI2) andthromboxane (TXA2) are increased during pregnancy, with the balance in favor of PGI2. In patients who develop preeclampsia, the balance shifts to favor TXA2. Again, PGI2 functions to promote vasodilatation and decrease platelet aggregation, and TXA2 promotes vaso-constriction and platelet aggregation. Because of this imbalance, vessel constriction occurs.
·
Changes
in endothelium-derived factors: Nitricoxide, a potent
vasodilator, is decreased in patients with preeclampsia and may explain the
evolution of vaso-constriction in these patients.
·
Lipid
peroxide, free radicals, and antioxidant release: Lipid
peroxides and free radicals have been implicated in vascular injury and are
increased in pregnancies com-plicated by preeclampsia. Decreased antioxidant
levels are also noted.
·
These five mechanisms, in any
combination or permutation, are thought to contribute to the following common
patho-physiologic changes seen in patients with preeclampsia:
·
Cardiovascular
effects: Elevated blood pressure is seenas the result of
potential vasoconstriction as well as an increase in cardiac output.
·
Hematologic
effects: Plasma volume contractionmay develop, with risk of
rapid onset hypovolemic shock, if hemorrhage occurs. Plasma volume con-traction
is reflected in increased hematocrit values. Thrombocytopenia/disseminated
intravascular coag-ulation may also develop from microangiopathic he-molytic
anemia. Involvement of the liver may lead to hepatocellular dysfunction and
further evolution of coagulopathy. Third spacing of fluid may be noted, because
of increased blood pressure and decreased plasma oncotic pressure.
·
Renal
effects: Decreased glomerular filtration rate(increasing
serum creatinine) and proteinuria (urine protein levels greater than 300 mg per
24 hours) develop secondary to atherosclerotic-like changes in the renal
vessels (glomerular endotheliosis). Uric acid filtration is decreased;
therefore, elevated maternal serum uric acid levels may be an indication of
evolving disease.
·
Neurologic
effects: Hyperreflexia/hypersensitivity maydevelop. In
severe cases, grand mal (eclamptic) seizures may develop.
·
Pulmonary
effects: Pulmonary edema may occur andcan be related to
decreased colloid oncotic pressure, pulmonary capillary leak, left heart
failure, iatrogenic fluid overload, or a combination of these factors.
·
Fetal
effects: Decreased intermittent placental perfu-sion
secondary to vasospasm is thought to be responsi-ble for the increased
incidence of intrauterine growth restriction (<10% estimated fetal weight
for gesta-tional age), oligohydramnios, and increased perinatal mortality of
infants born to mothers with preeclamp-sia. An increased incidence of placental
abruption is also seen. With the stress of uterine contractions dur-ing labor,
the placenta may be unable to adequately oxygenate the fetus. This may result
in signs of intra-partum uteroplacental insufficiency. Specifically, a
non-reassuring fetal-heart-rate pattern may necessitate cesarean delivery.
Presumably
because of vasospastic changes, placental size and func-tion are decreased. The
results are progressive fetal hypoxiaand malnutrition, as well as an increase
in the incidence of intrauterine growth restriction and oligohydramnios.
Related Topics