Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Hepatitis Viruses
Hepatitis B Disease : Clinical Aspects
HEPATITIS B DISEASE : CLINICAL ASPECTS
MANIFESTATIONS
The clinical picture of hepatitis B is highly variable. The incubation period may be as brief as 7 days or as long as 160 days (mean, approximately 10 weeks). Acute hepatitis B is usually manifested by the gradual onset of fatigue, loss of appetite, nausea and pain, and fullness in the right upper abdominal quadrant. Early in the course of disease, pain and swelling of the joints and occasional frank arthritis may occur. Some patients develop a rash. With increasing involvement of the liver, there is increasing cholestasis and, hence, clay-colored stools, darkening of the urine, and jaundice. Symptoms may persist for sev-eral months before finally resolving.
In general, the symptoms associated with acute hepatitis B are more severe and more prolonged than those of hepatitis A; however, anicteric disease and asymptomatic infec-tion occur. The infection-to-disease ratio, which varies according to age and method of acquisition, has been estimated to be approximately 6:1 or 7:1. Fulminant hepatitis, lead-ing to extensive liver necrosis and death, develops in less than 1% of cases. One impor-tant difference between hepatitis A and hepatitis B is the development of chronic hepati-tis. This occurs in approximately 10% of all patients with hepatitis B infection, but the risk is much higher for newborns (~100%), children (50%) and the immunocompromised. Chronic infection is associated with ongoing replication of virus in the liver and usually with the presence of HBsAg in serum. Chronic hepatitis may lead to cirrhosis, liver fail-ure, or hepatocellular carcinoma, in up to 25% of patients.
DIAGNOSIS
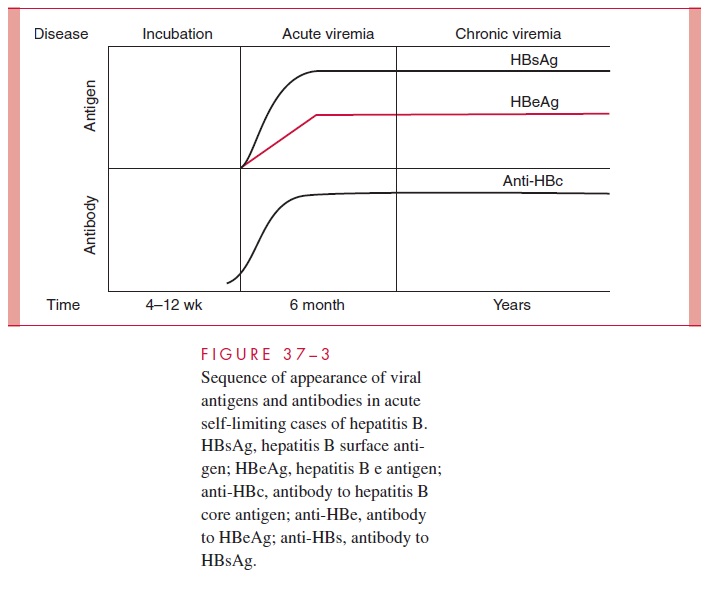
The nomenclature of hepatitis B antigens and antibodies is shown in Table 37–2 and the sequence of their appearance in Figure 37–3. During the acute episode of disease, when there is active viral replication, large amounts of HBsAg and hepatitis B virus DNA can be detected in the serum, as can fully developed virions and high levels of DNA polymerase and HBeAg. Although HBcAg is also present, antibody against it in-variably occurs and prevents its detection. With resolution of acute hepatitis B, HBsAg and HBeAg disappear from serum with the development of antibodies (anti-HBs and anti-HBe) against them. The development of anti-HBs is associated with elimination of infection and protection against reinfection. Anti-HBc is detected early in the course of disease and persists in serum for years. It is an excellent epidemiologic marker of infection, but is not protective. The laboratory diagnosis of acute hepatitis B is best made by demonstrating the IgM antibody to hepatitis B core antigen in serum. Al-most all patients who develop jaundice are anti-HBc IgM positive at the time of clinical presentation. HBsAg may also be detected in serum. Past infection with hepatitis B is best determined by detecting IgG anti-HBc, anti-HBs, or both.
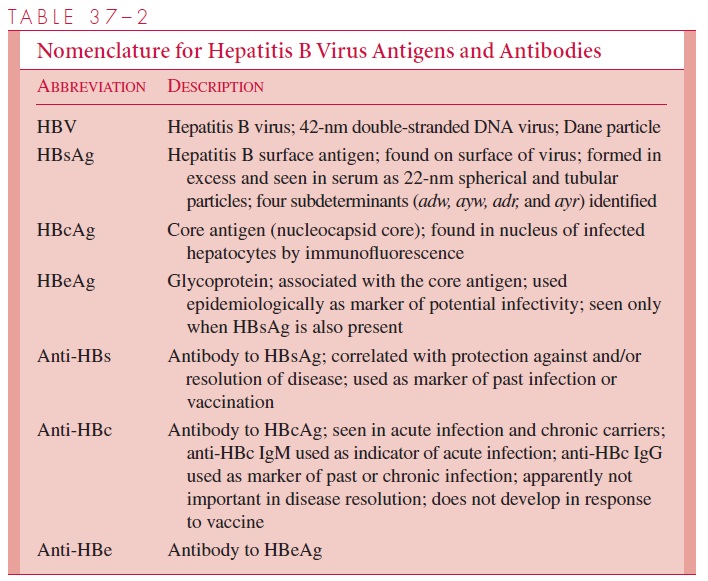
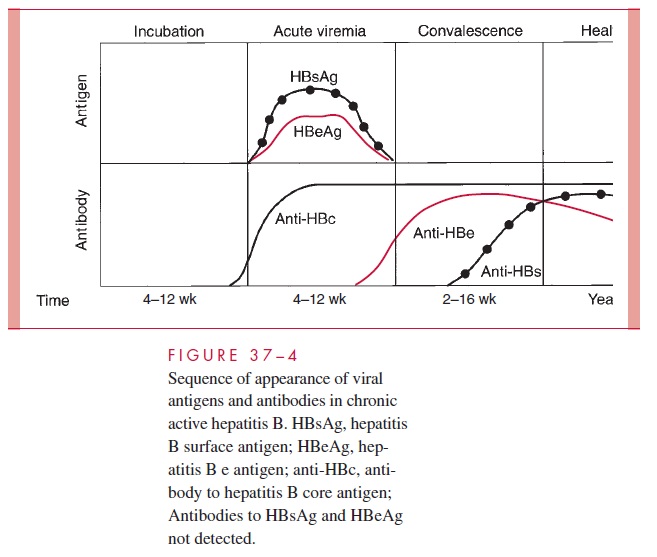
In patients with chronic hepatitis B, evidence of viral persistence can be found in serum (Figure 37–4). HBsAg can be detected throughout the active disease process and anti-HBs does not develop, which probably accounts for the chronicity of the disease. However, anti-HBc is detected. Two types of chronic hepatitis can be distinguished. In one, HBsAg is detected but not HBeAg; these patients usually show minimal evidence of liver dysfunction. In the other, both antigens are found; the process is more active, with continued hepatic damage that may result in cirrhosis. Chronic infection with hepatitis B is best detected by persistence of HBsAg in blood for more than 6 to 12 months.
TREATMENT
There is no specific treatment for acute hepatitis B. A high-calorie diet is desirable. Corticosteroid therapy has no value in uncomplicated acute viral hepatitis, and recent studies suggest that it may increase the severity of chronic hepatitis caused by hepatitis B virus.
For chronic hepatitis B diseases, interferon alpha 10 million units three times weekly for 4 months provides long-term benefit in a minority (~33%) of patients, usu-ally those who already demonstrate an acute immune response with low serum viral DNA levels. Lamivudine (3TC), a potent inhibitor of HIV is also active versus hepati-tis B virus both in vitro and in initial clinical trials, but resistance to this agent devel-ops in about 25% of patients after 12 months of therapy. Adefovir, a nucleotide analog of adenosine monophosphate, is newly approved for the treatment of chronic hepatitis B. Treatment should be considered for patients exhibiting chronic hepatitis B for more than 6 months with detectable serum levels of HBsAg, HBcAg, and hepatitis B DNA.
PREVENTION
Safe sex practices and avoidance of needlestick injuries or injection drug use are ap-proaches to diminishing the risk of hepatitis B infection. Both active prophylaxis and pas-sive prophylaxis of hepatitis B infection can be accomplished. Most preparations of ISG contain only moderate levels of anti-HBs; however, specific hepatitis B immune globulin (HBIG) with high titers of hepatitis B antibody is now available. HBIG is prepared from sera of subjects who have high titers of antibody to HBsAg but are free of the antigen itself. Administration of HBIG soon after exposure to the virus greatly reduces the devel-opment of symptomatic disease. Postexposure prophylaxis with HBIG should be fol-lowed by active immunization with vaccine. Inactivated hepatitis B vaccines have been available for several years. The first was developed by purification and inactivation of HBsAg from the blood of chronic carriers, but this is no longer in use. The current vac-cine is a recombinant product derived from HBAg grown in yeast. Excellent protection has been shown in studies on homosexual men and medical personnel. These groups and others, such as laboratory workers and injection drug users who come into contact with blood or other potentially infected materials, should receive hepatitis B vaccine as the preferred method of preexposure prophylaxis. Recently, immunization of all children has been recommended.
A combination of active and passive immunization is the most effective approach to prevent neonatal acquisition and the development of chronic carriage in the neonate. Most hospitals recommend routine screening of pregnant women for the presence of HBsAg. Infants born to those who are positive should receive HBIG in the delivery room followed by three doses of hepatitis B vaccine beginning 24 hours after birth. A similar combination of passive and active immunization is used for unimmunized persons who have been exposed by needlestick or similar injuries. The procedure varies depending on the hepatitis B status of the “donor” case linked to the injury.
Related Topics