Chapter: Obstetrics and Gynecology: Gynecological Procedures
Gynecological Procedures: Imaging Studies
IMAGING STUDIES
Gynecologic imaging plays an
important role in the diag-nostic evaluation of women for a variety of
reproductive health conditions. Although the ability to image various parts and
organs of the body has dramatically enhanced clinicians’ diagnostic
capabilities, these methods do not replace a careful and thoughtful history and
physical eval-uation. However, they can add more detail, which assists in both
medical and surgical management. The effective use of these modalities requires
that the physician be famil-iar with the benefits and limitations of each
method.
Ultrasonography
Ultrasonography
remains the most common modalityfor evaluation of
the female pelvis. It uses high-frequency sound reflections to identify
different body tissues and structures. Short bursts of low-energy sound waves
are sent into the body. When these waves encounter the interface between two
tissues that transmit sound differently, some of the sound energy is reflected
back toward the sound source. The returning sound waves are detected, and the
distance from the sensor is deduced using the elapsed time from transmission to
reception. An image is then created and displayed on a monitor. Ultrasonography is safe for preg-nant and
nonpregnant patients.
Most ultrasonography produces
two-dimensional images. Three-dimensional studies can be used for vol-ume
calculation and to provide detail about the surfaces of particular structures.
In gynecology, three-dimensional ultrasonography is especially useful in the
evaluation of müllerian abnormalities.
Four-dimensional ultrasonography, which shows movement, is also
available.
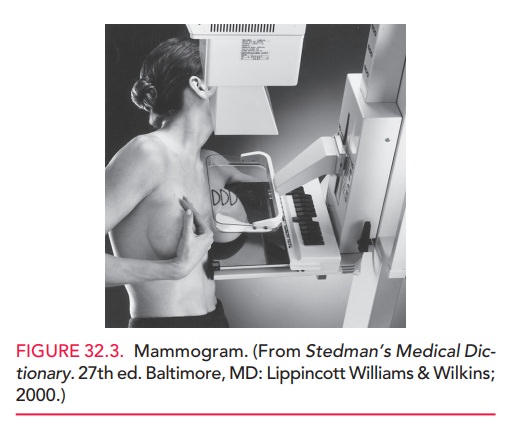
Two kinds of probes are used in
ultrasonography: trans-abdominal and transvaginal (Fig. 32.1). A transabdominal
probe has an increased depth of penetration, which allows for the assessment of
large uterine or adnexal masses. However, in obese patients, it may not allow
proper imag-ing of pelvic structures. A transvaginal probe can be placed
internally; thus, it often gives improved views of the cervix, uterus, ovaries,
and tubes. Also, it has a higher frequency and shorter depth of penetration,
which result in enhanced image clarity.
One of
the most valuable uses for ultrasonography in gyne-cology is for imaging
masses. The imaging technique helps dis-tinguish between
cystic and solid adnexal masses. Although magnetic resonance imaging (MRI) or
computed tomogra-phy (CT) can also be used for evaluation of ovarian cysts,
ultrasonography is far less costly; for this purpose, experts consider it
superior to either MRI or CT. It is also possible to delineate leiomyoma
(fibroid) size and number using ultrasonography.
Use of the endometrial stripe
thickness for evaluation of postmenopausal bleeding has been studied extensively.
Following menopause, the endometrium becomes atrophic and its thickness
decreases, remaining relatively constant without hormonal stimulation.
Ultrasonographic evalua-tion of the endometrial stripe involves measuring the
thick-est portion of the endometrial echo in the sagittal plane. An endometrial
stripe thickness of 5 mm or greater should be interpreted as abnormal in
postmenopausal women not tak-ing hormone therapy. These patients should receive
histo-logic assessment of an endometrial tissue sample to exclude endometrial
carcinoma.
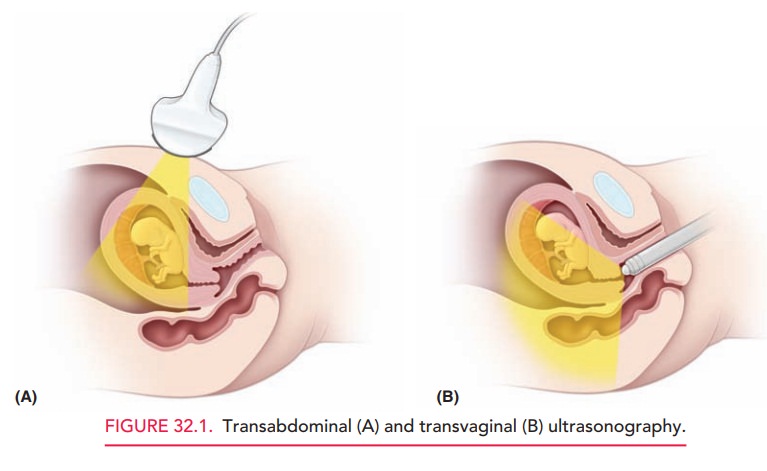
Saline infusion during ultrasonography (sonohys-terography, or SHG) can aid in the visualization of theendometrial cavity and can often identify intrauterine polyps or submucosal leiomyomas (Fig. 32.2). In this technique, saline is infused via a transcervically inserted catheter. The saline acts as a contrast agent to delineate the endometrium and intracavity masses. The primary role of SHG is in the diagnosis of the cause of abnormal uterine bleeding (AUB). It is preferred over unenhanced ultrasonography in the evaluation of AUB because of its increased diagnostic accuracy and greater cost-effectiveness.
Computed Axial Tomography
Computed
axial tomography (CT or CAT) scanninguses computer algorithms
to construct cross-sectional images based on x-ray information. With the use of
oral or intravenous contrast agents, CT scanning can help evaluate pelvic
masses, identify lymphadenopathy, or plan radiation therapy.
CT involves slightly greater radiation exposure than conventional single-exposure radiograph, but provides significantly more information. The radiation dose of an abdominal CT is still below that thought to cause fetal harm.
Nevertheless, because of CT’s increased risk of
fetal effects, magnetic resonance imaging
or ultra-sonography should be used for imaging instead of CT, whenever
possible in pregnancy.
Magnetic Resonance Imaging
Magnetic
resonance imaging (MRI) is based on themagnetic
characteristics of various atoms and molecules in the body. Because of the
variations in chemical composition of body tissues (especially the content of
hydrogen, sodium, fluoride, or phosphorus), MRI can distinguish between types
of tissues, such as blood and fat. This distinction is useful in visualizing
lymph nodes, which are usually sur-rounded by fat; in characterizing adnexal
masses; and in locating hemorrhage within organs. MRI is also useful for
visualizing the endometrium, myometrium, and cystic structures in the ovaries.
Emerging areas of clinical applic-ability include assessment of lesions in the
breast and stag-ing of cervical cancer.
Breast Imaging
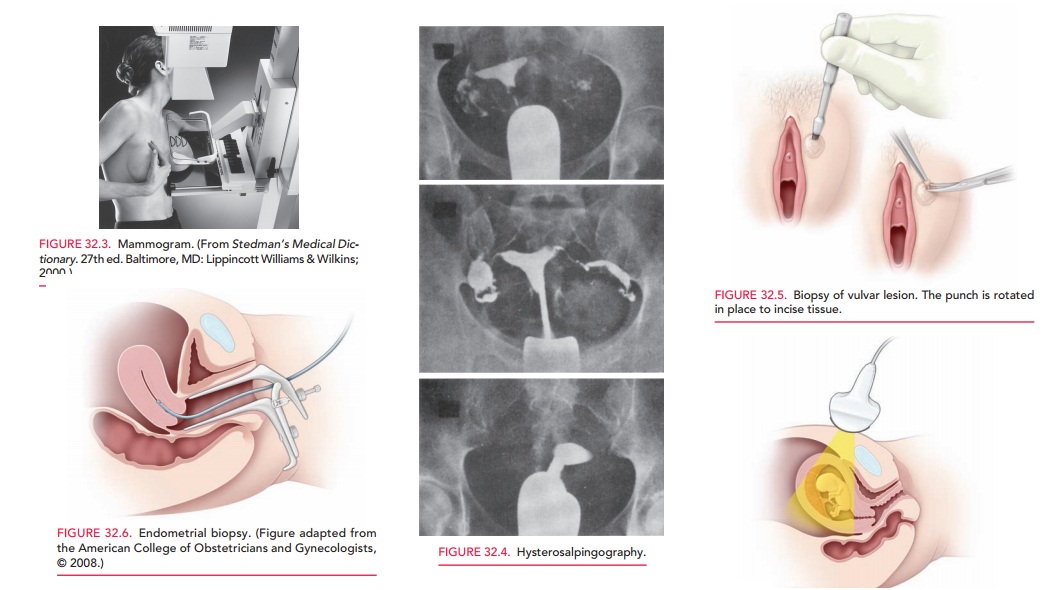
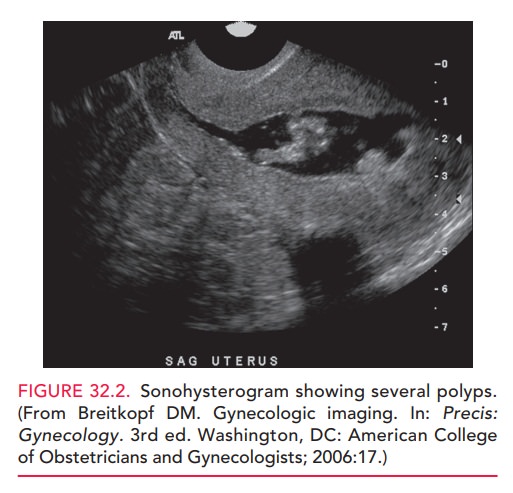
Mammography
is an x-ray procedure used to screen forbreast
cancer. It is performed by passing a small amount of radiation through
compressed breast tissue (Fig. 32.3). Because mammography has a high
false-positive rate (10% per screening in postmenopausal women and as high as
20% per screening in obese or premenopausal women), additional testing may be
required. Digital mammography allows better visualization of dense breast
tissue than con-ventional mammography.
Ultrasonography is also used to evaluate cystic or solid breast masses and guide aspiration of cysts. MRI may also be used as an imaging technique for breast tissue.
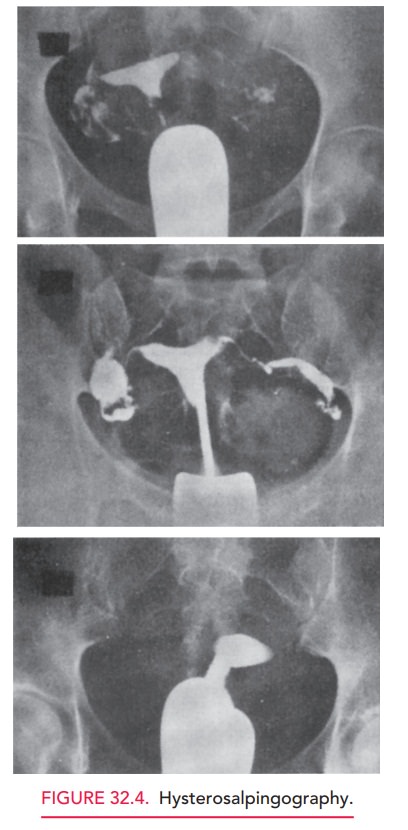
Hysterosalpingography
Hysterosalpingography
(HSG) is most often used toevaluate the patency of the
fallopian tubes in women who may be infertile. After a radio-opaque dye is
injected trans-cervically, fluoroscopy (live x-ray) is used to determine
whether dye spills into the peritoneal cavity (Fig. 32.4). HSG can also be used
to define the size and shape of the uterine cavity and to detect developmental
abnormalities, such as a unicornuate, septate, or didelphic uterus. It also can
demon-strate most endometrial polyps, submucous myomata, or intrauterine
adhesions that are significant enough to have important reproductive
consequences.
Related Topics