Chapter: Essentials of Psychiatry: Time-limited Psychotherapy (Including Interpersonal Therapy)
General Principles of Time-limited Psychotherapy
General
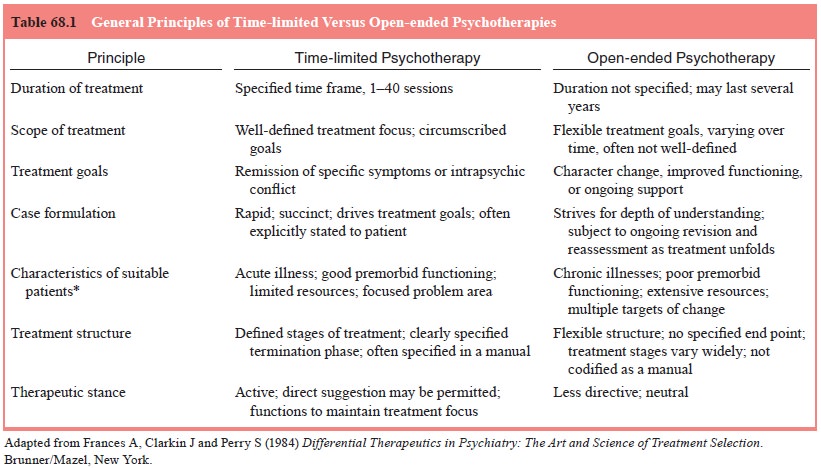
Principles of Time-limited Psychotherapy
The
hallmark of TLP is its specified treatment duration. Because of this
compression, TLPs share attributes that both link them to one another and
distinguish them from long-term treatment mo-dalities. These general principles
are summarized in Table 68.1.
Time Limit
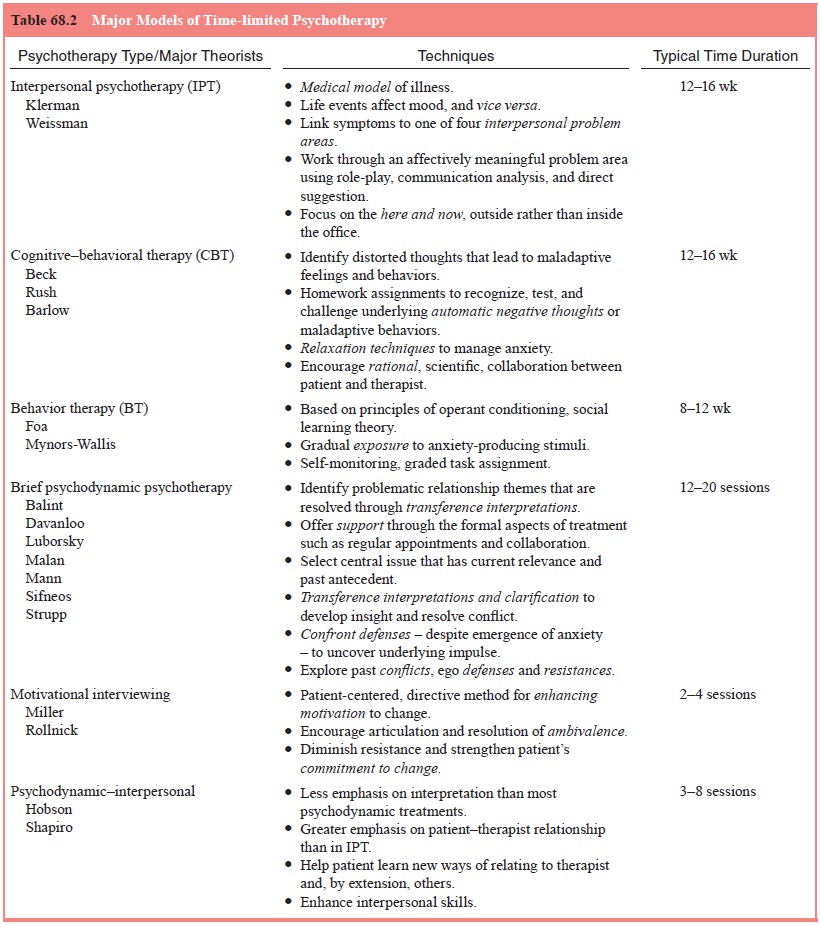
Table
68.2 groups psychotherapies commonly administered in a time-limited format by
treatment approach and lists representa-tive examples of strategies and typical
treatment durations.
TLPs
differ from truncated long-term treatments that are interrupted by attrition,
noncompliance, or the pressures of man-aged care organizations. The duration of
these latter therapies may coincide with that of a TLP, but they do not
constitute fully formed brief treatments. TLPs have distinctly defined
beginnings, middles, and ends – regardless of their absolute duration.
Knowl-edge from the outset that therapy has a defined end-point indeed may
constitute a key active ingredient of time-limited therapy. It suggests that
relief may be near at hand. Marmor speculates that this approach “counters the
patient’s impulse to see him-self as helpless, inadequate, and in need of
dependent support”. Our experience with IPT as a treatment for depression in
individuals who are HIV-seropositive suggests that these individuals, despite
shortened life spans, use the brev-ity of treatment as an impetus to effect
radical, rapid changes in their lives (Swartz and Markowitz, 1998). The time
limit, in a variety of ways, seems to provide an important motivation to speed
the patient toward health.
A meta-analysis
of many psychotherapy studies (none of them TLPs) found that most (75%)
patients achieve symptom relief within 26 sessions of an open-ended treatment
(Howard et al., 1986). Most
treatments included in this meta-analysis were naturalistic (e.g., not controlled) studies of patients suffering
from very heterogeneous symptoms (diagnoses are not specified). This finding
suggests that many patients may respond quickly, even if psychotherapy is
open-ended. Although no studies have com- pared prospectively response rates of
TLPs to open-ended treat-ments, we predict that treatment response would be
more rapid for patients receiving time-limited interventions because of
ex-plicit expectations that therapy will conclude within a specified time
frame. TLPs are generally dosed with a frequency of once a week, although this
varies as well.
The
optimal duration and dosage of TLP, although em-pirical questions, remain
largely unanswered to date. In practice, treatment duration is often defined by
convention, the exigencies of a research protocol or managed care organization,
or even the inclinations of the therapist.
IPT: Duration of Treatment
IPT was
originally designed as a 16-week intervention so that it could be administered
over the same period as an acute course of pharmacotherapy, allowing an
assessment of the relative efficacy of the two interventions (DiMascio et al., 1979). IPT is also administered
as a 14-session intervention (Markowitz unpublished data), a 12-session
intervention (Mufson et al., 1999;
O’Hara et al., 2000) and an
eight-session intervention (Swartz et al.,
2002), but there are no data comparing the relative benefits of varying doses of acute IPT.
Treatment Focus
An
important characteristic of TLP is careful definition of treat-ment goals,
which are usually agreed upon by the patient and therapist, and often specified
at the beginning of treatment. Because therapy is brief, the scope of the
treatment is circum-scribed and focused. TLPs do not attempt sweeping changes
in character. Rather, treatments target a specific diagnosis, set of symptoms,
or a narrow aspect of character. Typical and appro-priate treatment goals for
TLPs include remission of depressive symptoms, reduction in frequency of
binge-eating, and resolu-tion of a specific interpersonal conflict.
Most TLPs
define treatment goals by diagnostic criteria, in much the manner of
pharmacotherapies. IPT focuses on two discrete goals: remission of depressive
symptoms and resolu-tion of an interpersonal problem area (Weissman et al., 2000). Cognitive–behavioral
therapy for panic disorder focuses on reduction in frequency of panic attacks
and relief of general anxiety symptoms (Barlow, 1997). Motivational
interviewing, a brief intervention designed to facilitate behavior change, is
often administered for the sole purpose of helping patients reduce or eliminate
their alcohol consumption (Miller and Rollnick, 1991). Thus, although the
treatments vary in their focus, in all cases their treatment goals are narrow
and usually specified from the outset.
Case Formulation
Treatment
focus is closely allied with the broader concept of case formulation. According
to Eells, psychotherapy case for-mulation is “a hypothesis about the causes,
precipitants, and maintaining influences of a person’s psychological,
interper-sonal, and behavioral problems…. It should serve as a blueprint,
guiding
treatment” (Eells, 1997, pp. 1–2). In TLP, because time is short, the process
of generating a case formulation is also com-pressed. The therapist must
identify the most important compo-nents of the patient’s narrative, balancing
the urge to learn more about the patient’s life circumstances with the time
constraints of the TLP. Thus, the TLP therapist typically conducts an overview
of the patient’s psychosocial circumstances and then selects a few “hot” topics
– relevant both to the current complaint and the nature of the therapy – to
consider in greater depth. This ap-proach allows the therapist to develop an
informed, timely case formulation. The ability rapidly to develop and deliver
such a for-mulation is for many therapists among the more difficult but also
most valuable aspects of learning a TLP.
IPT: Case Formulation
Case
formulation in IPT builds on two core IPT concepts: 1) de-pression is a
treatable illness and 2) events in one’s psychosocial environment affect one’s
mood, and vice versa. The IPT thera-pist defines depression as a medical
illness that, like asthma, is both treatable and affected by the patient’s
circumstances. The therapist notes that, in a biologically vulnerable
individual, when painful events occur, mood worsens and depression may result.
Conversely, depressed mood compromises one’s ability to handle one’s social
role, generally leading to negative events. IPT thera-pists use the connections
among mood, environment and social role to help patients understand their
depressions within an inter-personal context, and to teach them to handle their
social role and environment so as to both solve their interpersonal problems
and relieve their depressive syndrome.
The
therapist’s formulation includes a diagnosis of depres-sion as a medical
illness, the provision of reassurance and hope, the assignment of the sick role
and, most importantly, the identi-fication of one (or at most two)
interpersonal problem areas that become the agenda for the remainder of the
treatment. The thera-pist directly states this case formulation to the patient
and elicits his or her agreement with the proposed strategy before moving ahead
with the next phase of treatment. Thus, in IPT, case for-mulation constitutes
an important treatment tool that links the patient’s mood symptoms to life
events and introduces a specific interpersonal problem area as the focus of
treatment for the ensu-ing sessions (Markowitz and Swartz, 1997).
The
brevity of treatment leaves little room for error in for-mulating the IPT case
– or any TLP case, for that matter. The therapist must use the initial
treatment sessions aggressively to pursue all potential areas and to determine
the treatment focus prior to embarking on the middle phase of treatment. If a
cov-ert and imposing problem area should arise in the middle phase, however,
the therapist would have to renegotiate the treatment contract to address it.
Structured Treatment
In TLP,
the structure of the intervention is clearly delineated and referenced
throughout the treatment period. The therapist will often call the patient’s
attention to important landmarks in the treatment: “Today we’ve reached the
halfway point” or “We only have three sessions left”. In manualized treatments,
each of these time intervals has specified tasks or strategies. For instance,
in IPT, the initial phase can last up to three sessions. During that time, the
therapist has spe-cific tasks (viz., obtain a psychiatric history and
interpersonal inven-tory, offer a case formulation). Similarly, the middle and
end phases of treatment have a specified duration and associated tasks.
In
support of the treatment structure, TLP requires the therapists to make formal
or informal “treatment contracts” in which the patient and therapist explicitly
or implicitly agree to goals, duration and other parameters of treatment. The
thera-pist may discuss with the patient the exact number of sessions planned,
rules for missed sessions or rescheduled sessions, fees and so on. Although
some aspects of treatment contracts are common to all psychotherapies, TLPs
tend to specify more ele-ments in the contract from the outset, including
expected treat-ment responses (e.g., “At the end of 16 weeks, your mood will
likely be much better”) and specific requirements of the patient (e.g.,
homework assignments in Prolonged Exposure and CBT). Patients often find the
transparent structure of TLPs reassuring, removing some of the unnecessary
mystery (and perhaps stigma) historically associated with psychotherapy.
Most TLPs
call for serial assessments of symptoms. In clinical practice (and in clinical
trials), it is often practical to administer a self-report measure such as the
Beck Depression Inventory (Beck and Steer, 1993) or the Beck Anxiety Inventory
(Beck and Steer, 1990). Regardless of the instrument chosen, it is important to
build into the weekly therapy session time to complete and review a
standardized symptom measure and track change over time. Serial symptom
assessment provides the pa-tient with additional psychoeducation (i.e., symptom
recognition) and a reliable means of tracking improvement (or lack thereof).
Active Therapist
In order
to maintain the treatment focus, the therapist must be ac-tive in TLP. He or
she must move the treatment process forward under the pressure of an inexorably
ticking clock. This demands constant attention to the treatment focus and
redirection of the patient if the focus falters. The therapist gently keeps the
patient on task, shaping the treatment rather than simply following the
patient’s lead. A challenge in TLP is to balance strict adherence to the
treatment focus with an empathic stance that supports the treatment alliance.
Although it is important to attend to the agreed upon problem area in IPT, it
is also important that the pa-tient feel “heard” and that the therapist allows
time in the session for the patient to express his or her feelings unimpeded.
Related Topics