Chapter: Essentials of Psychiatry: Factitious Disorders
Factitious Disorders: Treatment and Prognosis
Treatment and Prognosis
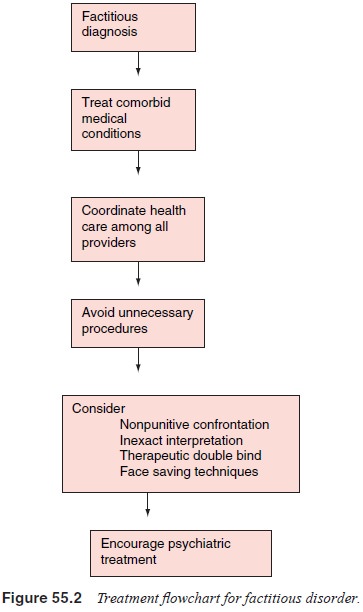
The goals in treating patients with factitious disorder are twofold;
first to minimize the damage done by the disorder to both the patient’s own
health and the health care system. The second goal is to help patients recover,
at least partially, from the disorder. These goals are furthered by treating
comorbid medical illnesses, avoiding unnecessary procedures, encouraging
patients to seek psychiatric treatment and providing support for health care
clini-cians. Because the literature is based exclusively on case reports and
series, determining treatment effectiveness is difficult. As mentioned before,
patients with true Munchausen’s syndrome (including antisocial traits,
pathological lying, wandering and poor social support) are felt to be
refractory to treatment. While factitious disorder is extremely difficult to
cure, effective tech-niques exist to minimize morbidity, and some patients are
able to benefit greatly from psychiatric intervention.
The course of untreated factitious disorder is variable. While patients
with factitious disorder commonly suffer a great deal of morbidity, fatal cases
appear to be less common. One sur-vey of 41 cases noted only one fatality,
though many of the other cases were life-threatening (Reich and Gottfried,
1983). However, patients with psychological signs and symptoms are reported to
have a high rate of suicide and a poor prognosis.
Soon after the widely noted publication of the first arti-cle on
factitious disorders (Asher, 1951) many patients with fac-titious disorder were
vigorously confronted once the nature of their illness was discovered.
Unfortunately, most patients would deny their involvement and seek another
provider who was una-ware of their diagnosis (Eisendrath, 2001). In addition,
the idea of “blacklists” was proposed in order to aid detection of these
pa-tients. However, issues regarding patient confidentiality as well as
concerns about cursory medical evaluations that might miss genuine physical
illness prevented this idea from being adopted. Although aggressive
confrontation is usually unsuccessful, sup-portive, nonpunitive confrontation
may be helpful for some. In one case series, 33 patients were confronted with
the factitious nature of their illness. While only 13 admitted feigning
illness, most of the patients’ illnesses subsequently improved, at least in the
short term (Reich and Gottfried, 1983).
Eisendrath suggested three alternatives to confrontation that he found
effective. First is inexact interpretation, in which the psy-chiatrist
interprets the psychodynamics thought to be underlying the patient’s behavior
without explicitly identifying the factitious behavior. He gave the example of
a patient suspected of having fac-titious disorder who developed septicemia after
her boyfriend pro-posed marriage. The consultant suggested that the patient
might feel a need to punish herself when good things happened to her. She
agreed and, soon after, admitted that she had injected a con-taminant
intravenously (Eisendrath, 2001). The second technique is the therapeutic
double-blind. The physician presents the patient with a new medical
intervention to treat his or her illness. The patient is told that one
possibility is that the patient’s illness has a factitious origin, and that, if
so, the treatment would not be ex-pected to work while, if the illness is
biological, the treatment will work and the patient will improve. The patient
must decide to give up the factitious illness or admit it. A third technique is
to provide the patient with a face-saving way, such as hypnosis or
biofeed-back, of giving up his or her symptoms without admitting that they are
not genuine. Eisendrath (2001) points out that in emergent situ-ations, there
may not be time for nonconfrontational techniques, and more directly
confrontational means may be necessary.
Another important component in the treatment of patients with factitious
disorder is the coordination of health care amongall providers. This allows for
fewer unnecessary interventions, minimizes splitting among the health care
team, and allows the health care team to vent and process the strong emotions
that arise when caring for factitious patients. This decreases both the
negative impact on the providers and the chance that anger will be acted out on
the patient.
There are no clear data supporting the effectiveness of medications in
treating factitious disorder. There is a case report of effective pimozide
treatment in a patient thought to have de-lusional symptoms (Prior and Gordon,
1997), as well as a case report of a factitious patient with comorbid
depression improv-ing when treated with an antidepressant in addition to
intensive psychotherapy.
While many patients with factitious disorder are hesitant to pursue
psychiatric treatment, there are numerous case reports of successful treatment
of the disorder with long-term psycho-therapy. In many of these cases, the
therapy lasted several years, including one patient who received treatment
while imprisoned for over 10 years. Plassman reports a case series of 24
factitious patients. Twelve of these patients accepted psychotherapy and 10
continued with long-term treatment, lasting up to 4½ years. He reports
“significant, or at least marked, improvement” in those 10 patients (Plassmann,
1994b). These case reports support the idea that treatment of patients with
factitious disorder is not im-possible, and these patients can improve.
However, expectations must be realistic as improvement in the disorder itself
can take several years. Techniques that target short-term reduction in the
production of factitious symptoms can be effective more quickly. See Figure
55.2 for a treatment flowchart for factitious disorder.
Related Topics