Chapter: Essentials of Psychiatry: Factitious Disorders
Factitious Disorders: Diagnosis and Differential Diagnosis, Epidemiology, Etiology
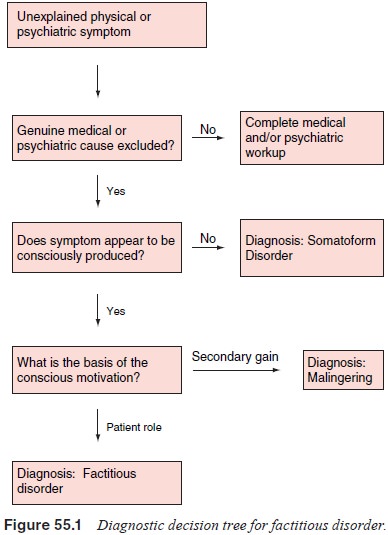
Diagnosis and Differential Diagnosis
The diagnosis of factitious disorder is made in several ways.
Fac-titious disorder is occasionally diagnosed accidentally when the patient is
discovered in the act of creating symptoms. A history of inconsistent or
unexplainable signs and symptoms or failure to respond to appropriate treatment
can prompt health care provid-ers to probe for evidence of the disorder, as can
evidence of per-egrination or pathological lying. In some cases, it is a
diagnosis of exclusion in an otherwise inexplicable case. The differential
diagnosis of factitious disorder includes rare or complex physi-cal illness,
somatoform disorders, malingering, other psychiatric disorders and substance
abuse. It is especially important to rule out genuine physical illness since
patients with factitious disor-der often induce real physical illness.
Furthermore, it is always important to remember the patients with factitious
disorder are certainly not immune to the physical illnesses that plague the
general population.
If there is suspicion of factitious disorder, confirmation can be
difficult. Laboratory examination can confirm some fac-titious diagnoses such
as exogenous insulin or thyroid hormone administration. Collateral information
from family members or previous health care providers can also be extremely
helpful. Factitious disorder with psychological signs and symptoms can
be particularly difficult to diagnose, as so much of psychiat-ric
diagnosis relies on the patient’s report. However, there is some evidence that
neuropsychological testing may be helpful in making the diagnosis. There are
conflicting reports about the ability to detect over 90% of cases of factitious
post traumatic stress disorder using the MMPI. In addition, there is a report
of MMPI test results being used to support a diagnosis of facti-tious disorder
with psychological features in a woman thought to be feigning symptoms of
multiple personality disorder (see Figure 55.1).
Epidemiology
The nature of factitious disorder makes it difficult to determine how
common it is within the population. Patients attempt to conceal themselves,
thereby artificially lowering the prevalence. The tendency of patients to
present several times at different facilities, however, may artificially raise
the prevalence. Most estimates of the prevalence of the disease, therefore,
rely on the number of factitious patients within a given inpatient popula-tion.
Such attempts have generated estimates that 0.5 to 3% of medical and
psychiatric inpatients suffer from factitious disor-der. Of 1288 patients
referred for psychiatric consultation at a Toronto general hospital, 10 (0.8%) were
diagnosed with facti-tious disorder. A prospective examination of all 1538
patients hospitalized in a Berlin neurology department over 5 years found five
(0.3%) cases of factitious disorder. An examination of 506 patients with fever
of unknown origin (FUO) revealed that 2.2% of the fevers were of factitious
origin, and a review of 199 Belgian patients with FUO found seven of 199 (3.5%)
to be factitious. A similar study of patients with FUO at the National
Institutes of Health (NIH) revealed that 9.3% of the fevers were
factitious. The increased prevalence found at the NIH may be due to the fact
that the study was undertaken in a more terti-ary setting, and it is a reminder
that the prevalence of factitious disorder likely varies widely depending on
the population and the setting. Gault and colleagues (1988) examined 3300 renal
stones brought in by patients and found that 2.6% of these stones were mineral
and felt to be submitted by factitious or malin-gering patients. There is much
less data on the prevalence of factitious disorder with psychological features.
A study of psy-chiatric inpatients showed a prevalence of 0.5% of admissions
determined to be a result of a factitious psychological condition. There are
few data about the prevalence of factitious disorder in an outpatient
population. Because factitious patients do not readily identify themselves in
large community surveys, it is not currently possible to determine the
prevalence of the disorder in the general population.
Etiology
Both psychological and biological factors have been postulated to play a
role in the etiology of factitious disorder. Although nu-merous case reports
have generated speculation that factitious disorder may run in families, this
could be explained by environ-mental factors, genetic factors, or both. The
presence of central nervous system (CNS) abnormalities in some patients with
fac-titious disorders have led some to hypothesize that underlying brain
dysfunction contributes to factitious disorder. One review of factitious patients
with pseudologia fantastica found CNS abnormalities (such as EEG abnormality,
head injury, imaging abnormalities, or neurological findings) in 40% of the
patients (King and Ford, 1988). There have been case reports of MRI and SPECT
abnormalities, but it is unknown if these abnormalities were related to the
disorder.
In addition, childhood developmental disturbances are thought to
contribute to factitious disorder. Predisposing fac-tors are thought to include
1) serious childhood illness or ill-ness in a family member during childhood,
especially if the illness was associated with attention and nurturing in an
other-wise distant family, 2) past anger with the medical profession, 3) past
significant relationship with a health care provider, and 4) factitious
disorder in a parent (McKane and Anderson, 1997).
Patients with factitious disorder create illness in pursuit of the sick
role. For these patients, being in the sick role allows them to compensate for
an underlying psychological deficit. Most authors identify several common
psychodynamic motiva-tions for factitious disorder. First, patients with little
sense of self may seek the sick role in order to provide a well-defined
iden-tity around which to structure themselves. Others may seek the sick role
in order to meet dependency needs which have gone unmet elsewhere. As a
patient, they receive the attention, caring and nurturing of the health care
environment and are relieved of many of their responsibilities. In addition,
some patients may engage in factitious behaviors for masochistic reasons. They
feel they deserve punishment for some forbidden feelings and thus they should
suffer at the hands of their physicians. Other patients may be motivated by
anger at physicians and dupe them in re-taliation. Patients with a history of
childhood illness or abuse may attempt to master past traumas by creating a
situation over which they have control. Finally, some authors have speculated
that some patients may be enacting suicidal wishes through their factitious behavior.
Related Topics