Chapter: Clinical Cases in Anesthesia : Labor And Delivery
Explain the risk factors, presentation, and treatment of uterine atony
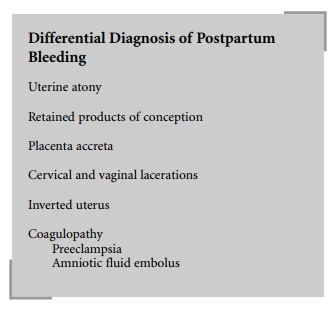
Explain the risk factors,
presentation, and treatment of uterine atony.
Any condition associated with overdistention of
the uterus, such as multiple births, polyhydramnios, or a large baby, is a risk
factor for uterine atony. Other risk factors include multiparity, retained
placenta, prolonged labor, previous tocolysis, β-agonists, prolonged general anesthe-sia with
potent inhaled anesthetic agents, ruptured uterus, and chorioamnionitis.
Uterine atony presents as continued painless
vaginal bleeding after delivery. The noncontracting uterus appears boggy and
large. Obstetric management is aimed at increasing myometrial tone. Massaging
the uterus through the abdominal wall or directly via the vagina is initially
attempted to induce contractions. If massaging does not work, oxytocin and
ergot derivatives are administered intravenously as well as prostaglandin F2α directly into the uterus to induce contractions.
Anesthetic management is initially aimed at
maternal resuscitation. Intravascular volume is restored with crystal-loid,
colloid, and/or blood. Massive blood loss may lead to shock. Coagulation factor
replacement may be required. Vaginal examination and suturing in attempts to
stop the bleeding require anesthesia; however, conduction techniques are
hazardous in the face of hypovolemia. Intravenous sedation with small amounts
of fentanyl, ketamine, and/or midazolam generally suffices. If sedation is
inadequate, a rapid sequence induction of general anesthesia with endo-tracheal
intubation is required to reduce the risk of mater-nal aspiration.
Continued hemorrhage may require hypogastric
artery ligation or hysterectomy, which necessitate general anes-thesia.
Anesthetic management for these procedures is the same as for placenta previa.
Pelvic artery embolization, usually performed in the radiology suite, can
sometimes reduce the bleeding and prevent the need for a hysterectomy. Although
general anesthesia is not required, maternal fluid resuscitation must be
continued during embolization.
Frequent vital sign monitoring is required and
resuscitative equipment must be available.
Successful intraoperative cell salvage (cell
saver) have been reported in obstetrics. The major concern with its usage is
that the amniotic fluid will not be completely removed during the centrifuging
and cleansing process leading to iatrogenic amniotic fluid embolism.
Recommendations for its use include discarding all surgi-cal field fluids
before collecting blood with the cell saver device. Use of this technique
should be reserved for situa-tions where there is no other blood available or
the patient refuses autologous blood transfusion (Jehovah’s witness).
Related Topics