Chapter: Clinical Cases in Anesthesia : Labor And Delivery
Explain the advantages and disadvantages of various regional anesthetic techniques for labor and delivery
Explain
the advantages and disadvantages of various regional anesthetic techniques for
labor and delivery.
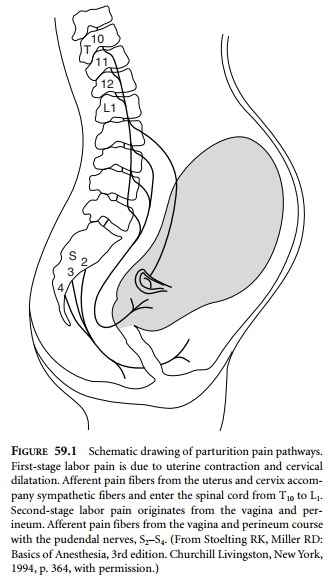
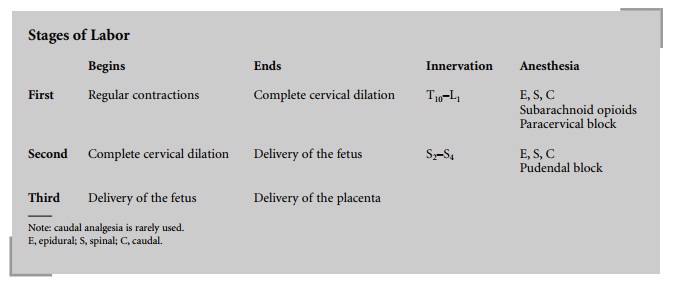
Rational use of regional anesthesia
necessitates an understanding of the pain pathways involved during labor. Labor
is traditionally divided into three distinct stages:
·
First
stage: begins with the onset of regular contractions and ends with complete
cervical dilation.
·
Second
stage: begins when the cervix is completely dilated and ends with delivery of
the fetus.
·
Third
stage: begins after delivery of the fetus and con-cludes with delivery of the
placenta.
The first stage of labor is associated with
uterine and cer-vical pain mediated by spinal segments T10–L1
(Fig. 59.1). Local anesthetics administered to the epidural, spinal, or caudal
spaces readily anesthetize these pain pathways. In addition, subarachnoid
opioids and paracervical blocks can be used for pain relief during the first
stage of labor.
Caudal anesthesia is rarely used because of the
risk of inadvertent fetal scalp penetration and the associated high fetal
levels of local anesthetic.
The second stage of labor is associated with
perineal and vaginal distention mediated by spinal segments S2–S4.
Epidural, spinal, and caudal anesthetics are also effective during the second
stage of labor. In addition, pudendal nerve blocks can be used for second-stage
analgesia.
Epidural analgesia is the most popular
technique for the relief of labor pain. Its popularity is first and foremost
related to its efficacy. Women can obtain almost complete relief from the pain
of labor. From the anesthesiologist’s perspective, because a catheter is
threaded into the epidural space, it is also a versatile technique. During the
earlier stages of labor, dilute solutions of local anesthetic can be used to
achieve analgesia. As labor progresses, a more con-centrated solution of local
anesthetic may be necessary or an adjunct, such as an opioid, may be needed.
Additionally, the epidural catheter can be utilized to maintain a low dermatomal
level of anesthesia for labor (T10–L1) and, when needed,
the dermatomal level can be raised to T4 for cesarean section.
Patient-controlled epidural analgesia (PCEA) is
a tech-nique that allows the patient to self-medicate, thereby controlling her
own analgesia. Compared with continuous infusion or intermittent bolus
techniques, PCEA is associ-ated with a lower total dose of local anesthetic,
less motor blockade, and fewer interventions by anesthesiologists. Although
maternal satisfaction may be greater with PCEA, the above-stated advantages
have not been documented in all studies. Therefore, this technique is not
routinely offered.
A commonly used PCEA regimen is bupivacaine
0.0625% with fentanyl 2 ÎĽg/mL with the following PCEA settings: basal
rate of 10 mL/hr, bolus dose of 5 mL, 10 minute lockout, and a 30 mL/hr maximum
limit. A basal rate is not always used because it may be associated with a
greater total milligram dose of local anesthetic when compared with the total
milligram dose when a basal rate is used. Theoretical risks of PCEA, such as
high der-matomal levels or overdose, have been described in the general
surgical patient. Overdose occurs because of catheter migration into the
subarachnoid space or from excessive administration by the patient or a helpful
family member. To date, these complications have not been reported in the
parturient during labor.
There are a number of disadvantages with labor
epidural analgesia that have prompted the search for alter-native techniques.
One disadvantage is the time it takes to provide analgesia to the patient. The
time from epidural catheter placement until the patient is comfortable is
vari-able, but depending on the local anesthetic used can take up to 30
minutes. Other disadvantages of labor epidural analgesia include: maternal
hypotension, inadequate anal-gesia (15–20% of cases), and motor blockade, even
with the very dilute local anesthetic solutions.
Subarachnoid opioids offer rapid, intense
analgesia with minimal changes in blood pressure or motor function. Most
patients can, if desired, ambulate with this technique. The opioid is usually
administered as part of a combined spinal-epidural (CSE) technique where a
spinal and an epidural are performed at the same time. After locating the
epidural space in the usual manner, a long small-gauge spinal needle is
inserted through the epidural needle into the subarachnoid space. An opioid
(usually fentanyl 25 ÎĽg or sufentanil 5 ÎĽg), either alone or in combination with a local anesthetic, is
administered through the spinal needle. The spinal needle is removed and an
epidural catheter is inserted for future use. Analgesia begins within 3–5
min-utes and lasts 1–1.5 hours.
There are several advantages to the CSE
technique. The primary advantage is the rapid (3–5 min) onset of analge-sia.
There is also less motor blockade. Because of these advantages there is greater
satisfaction by women who receive a CSE than those who receive the “standard”
epidural technique of bupivacaine 0.25%.
There are some concerns about CSE, most of
which are only theoretical but have not been documented. There is no increased
risk of subarachnoid catheter migration of the epidural catheter. Metallic
particles are not produced as a result of passing one needle through another.
The incidence of postdural puncture headache is not increased by the
intentional dural puncture. Fetal bradycardia in association with a hypertonic
uterus may occur immedi-ately or shortly after induction of either epidural or
subarachnoid labor analgesia. There does not appear to be any difference in the
incidence of fetal heart rate decel-erations or emergent cesarean section
following labor epidural or spinal anesthesia. One proposed theory for
increased uterine tone after CSE is related to the rapid decrease in maternal
catecholamines associated with the rapid onset of pain relief. The decrease in
circulating β-adrenergic agonists results in a predominance of α activ-ity, which causes uterine contractions. If this should occur,
treatment is with subcutaneous terbutaline or intravenous nitroglycerin.
Related Topics