Chapter: Psychiatric Mental Health Nursing : Somatoform Disorders
Etiology - Somatoform Disorders
ETIOLOGY
Psychosocial Theories
Psychosocial theorists believe that people with somatoform
disorders keep stress, anxiety, or frustration inside rather than expressing
them outwardly. This is called internalization. Clients express these
internalized feelings and stress through physical symptoms (somatization).
Both internalization and somatization are unconscious defense
mechanisms. Clients are not consciously aware of the process, and they do not
voluntarily control it.
People with somatoform disorders do not readily and directly
express their feelings and emotions verbally. They have tremendous difficulty
dealing with interpersonal conflict. When placed in situations involving
conflict or emotional stress, their physical symptoms appear to worsen. The
worsening of physical symptoms helps them to meet psychologic needs for
security, attention, and affection through primary and secondary gain
(Hollifield, 2005). Primary gains
are the direct external benefits that being sick provides, such as relief of
anxiety, conflict, or distress. Secondary
gains are the internal or personal ben-efits received from others because
one is sick, such as attention from family members and comfort measures (e.g.,
being brought tea, receiving a back rub). The person soon learns that he or she
“needs to be sick” to have their emotional needs met.
Somatization is associated most often with women, as evidenced by
the old term hysteria (Greek for
“wandering uterus”). Ancient theorists believed that unexplained female pains
resulted from migration of the uterus through-out the woman’s body.
Psychosocial theorists posit that increased incidence of somatization in women
may be related to various factors:
·
Boys in the United States are taught to be stoic and to “take it
like a man,” causing them to offer fewer physi-cal complaints as adults.
·
Women seek medical treatment more often than men, and it is more
socially acceptable for them to do so.
·
Childhood sexual abuse, which is related to somatiza-tion, happens
more frequently to girls.
·
Women more often receive treatment for psychiatric disorders with
strong somatic components such as depression.
Biologic Theories
Research has shown differences in the way that clients with
somatoform disorders regulate and interpret stimuli. These clients cannot sort
relevant from irrelevant stimuli and respond equally to both types. In other
words, they may experience a normal body sensation such as peristal-sis and
attach a pathologic rather than a normal meaning to it (Hollifield, 2005). Too
little inhibition of sensory input amplifies awareness of physical symptoms and
exag-gerates response to bodily sensations. For example, minor discomfort such
as muscle tightness becomes amplified because of the client’s concern and
attention to the tight-ness. This amplified sensory awareness causes the person
to experience somatic sensations as more intense, noxious, and disturbing
(Andreasen & Black, 2006).
Somatization disorder is found in 10% to 20% of female first-degree
relatives of people with this disorder. Conver-sion symptoms are found more
often in relatives of people with conversion disorder. First-degree relatives of
those with pain disorder are more likely to have depressive disor-ders, alcohol
dependence, and chronic pain (APA, 2000).
Cultural Considerations
The type and frequency of somatic symptoms and their meaning may
vary across cultures. Pseudoneurologic symptoms of somatization disorder in
Africa and South Asia include burning hands and feet and the nondelu-sional
sensation of worms in the head or ants under the skin. Symptoms related to male
reproduction are more common in some countries or cultures—for example, men in
India often have dhat, which is a
hypochondriacal concern about loss of semen. Somatization disorder is rare in
men in the United States but more common in Greece and Puerto Rico.
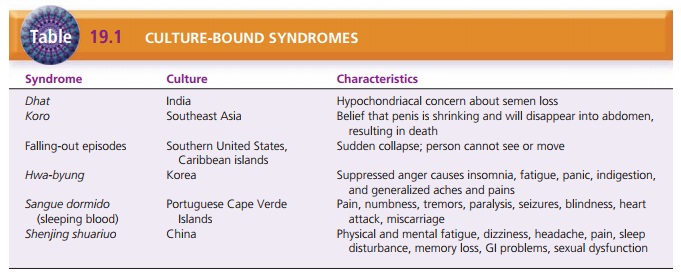
Many culture-bound syndromes have corresponding somatic symptoms
not explained by a medical condition (Table 19.1). Koro occurs in Southeast Asia and may be related to body dysmorphic
disorder. It is characterized by the belief that the penis is shrinking and
will disap-pear into the abdomen, causing the man to die. Falling-out episodes,
found in the southern United States and the Caribbean islands, are
characterized by a sudden collapse during which the person cannot see or move. Hwa-byung is a Korean folk syndrome
attributed to the suppression of anger and includes insomnia, fatigue, panic,
indiges-tion, and generalized aches and pains. Sangue dormido (sleeping blood) occurs among Portuguese Cape Verde
Islanders who report pain, numbness, tremors, paralysis, seizures, blindness,
heart attacks, and miscarriages. Shenjing
shuariuo occurs in China and includes physical and mental fatigue, dizziness, headache, pain, sleep dis-turbance,
memory loss, gastrointestinal problems, and sexual dysfunction (Mojtabai,
2005).
Treatment
Treatment focuses on managing symptoms and improving quality of
life. The health care provider must show empathy and sensitivity to the
client’s physical complaints. A trusting relationship helps to ensure that clients
stay with and receive care from one provider instead of “doctor shopping.”
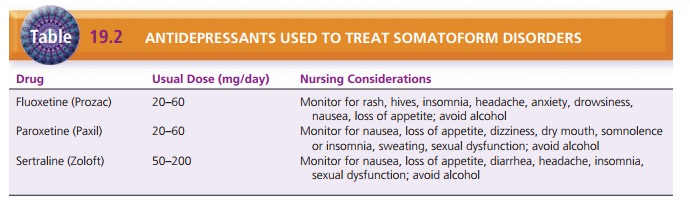
For many clients, depression may accompany or result from
somatoform disorders (Ferrari, Galeazzi, Mackinnon, Rigatelli, 2008). Thus,
antidepressants help in some cases. Selective serotonin reuptake inhibitors
such as fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil) are
used most commonly (Table 19.2).
For clients with pain disorder, referral to a chronic pain clinic
may be useful. Clients learn methods of pain management such as visual imaging
and relaxation. Ser-vices such as physical therapy to maintain and build
mus-cle tone help to improve functional abilities. Providers should avoid
prescribing and administering narcotic anal-gesics to these clients because of
the risk for dependence or abuse. Clients can use nonsteroidal
anti-inflammatory agents to help reduce pain.
Involvement in therapy groups is beneficial for some people with
somatoform disorders. Studies of clients with somatization disorder who participated
in a structured cognitive-behavioral group showed evidence of improved physical
and emotional health 1 year later (Hollifield, 2005). The overall goals of the
group were offering peer support, sharing methods of coping, and perceiving and
expressing emotions. Abramowitz and Braddock (2006) found that clients with
hypochondriasis who were willing to participate in cognitive-behavioral therapy
and take medications were able to alter their erroneous perceptions of threat
(of illness) and improve. Cognitive-behavioral therapy also produced
significant improvement in clients with somatization disorder (Allen, Woolfolk,
Escobar, Gara, & Hamer, 2006).
Related Topics