Chapter: Pathology: Skin Pathology
Epidermal and Dermal Lesions
EPIDERMAL AND DERMAL LESIONS
Acanthosis
nigricans causes thickened, hyperpigmented skin of the posterior
neck,axillae, and groin; it is often associated with obesity and
hyperinsulinism. On rare occasions it is associated with internal malignancy
(stomach and other gastrointes-tinal malignancies).
Seborrheic
keratoses are benign squamoproliferative neoplasms that are very
com-mon in middle-aged and elderly individuals; they may occur on the trunk,
head, neck, and the extremities. The lesions are tan to brown coin-shaped
plaques that have a granular surface with a “stuck on” appearance,
characterized microscopi-cally by basaloid epidermal hyperplasia and “horn
cysts” (keratin-filled epidermal pseudocysts). They are usually left untreated,
but may be removed if they become irritated or for cosmetic purposes. The sign
of Leser-Trélat (paraneoplastic syn-drome) is the sudden development of
multiple lesions which may accompany an internal malignancy.
Psoriasis
is an autoimmune disorder with a clear genetic component
that causesincreased proliferation and turnover of epidermal keratinocytes; it
affects 1% of the U.S. population. The most common form is psoriasis vulgaris.
Common sites of involvement include the knees, elbows, and scalp; the classic
skin lesion is a well-demarcated erythematous plaque with a silvery scale.
Removal of scale results in pinpoint bleeding (Auspitz sign). Nail beds show
pitting and discoloration. Psoriasis may be associated with arthritis,
enteropathy, and myopathy.

Microscopically, the lesions show epidermal
hyperplasia (acanthosis), patchyhyperkeratinization with parakeratosis, uniform
elongation and thickening of the rete ridges, thinning of the epidermis over
the dermal papillae, and Munro microabscesses.
Treatment
is topical steroids and ultraviolet irradiation; severe systemic dis-ease may
be treated with methotrexate.
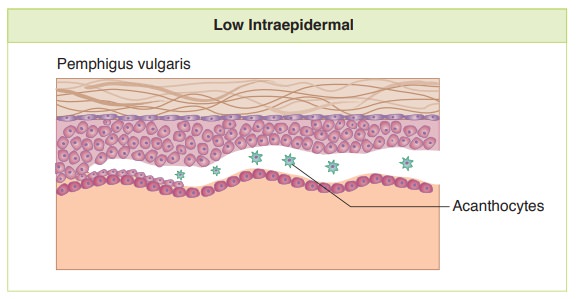
Pemphigus
is a rare, potentially fatal autoimmune disorder that is
characterized byintraepidermal blister formation. Pemphigus vulgaris is the
most common form. The pathogenesis involves the production of autoantibodies
directed against a part of the keratinocyte desmosome called desmoglein 3, with
resulting loss of intercellu-lar adhesion (acantholysis) and blister formation.
Pemphigus causes mucosal lesions and easily ruptured, flaccid blisters. Oral
involvement is common.
·
Microscopic examination shows intraepidermal
acantholysis; the acantholy-sis leaves behind a basal layer of keratinocytes,
which has a tombstone-like arrangement. Immunofluorescence shows a net-like
pattern of IgG staining between the epidermal keratinocytes that create bullae.
·
Treatment is with immunosuppression.
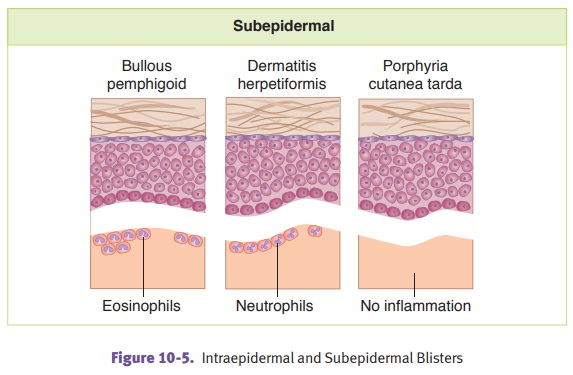
Bullous
pemphigoid is a relatively common autoimmune disorder of older
individu-als characterized by subepidermal blister formation with tense bullae
that do not rupture easily. The condition results from production of autoantibodies
directed against a part of the keratinocyte hemidesmosome called bullous pemphigoidantigens 1 and 2.
Immunofluorescence shows linear deposits of IgG at the dermal-epidermal
junction.
Dermatitis
herpetiformis is a rare immune disorder that is often associated
withceliac sprue; it is characterized by subepidermal blister formation with
itchy, grouped vesicles and occasional bullae on the extensor surfaces.
Production of IgA antibodies directed against gliadin and other antigens
deposit in the tips of the dermal papillae and result in subepidermal blister
formation. Routine microscopy shows microabscesses at the tips of the dermal
papillae that can lead to eventual subepidermal separation results in blister
formation; immunofluorescence shows granular IgA deposits at the tips of the
dermal papillae. Dermatitis herpetiformis often responds to a gluten-free diet.
Porphyria
cutanea tarda is an acquired and familial disorder of heme
synthesis.Patients experience upper extremity blistering secondary to sun exposure
and minor trauma. Microscopically, there are subepidermal blisters with minimal
inflamma-tion. Dermal vessels are thickened. Direct immunofluorescence shows
deposition of immunoglobulins and complement at the epidermal basement membrane
and around dermal vessels.
Ichthyosis
vulgaris is a common inherited (autosomal dominant) skin
disordercharacterized by a thickened stratum corneum with absent stratum
granulosum. Onset is in childhood. Patients have hyperkeratotic, dry skin on
the trunk and extensor surfaces of limb areas.
Xerosis is
a common cause of pruritus and dry skin in the elderly that is due todecreased
skin lipids. Cancer patients receiving epidermal growth factor receptor
inhibitor are susceptible. Treatment is with emollients.
Eczema is
a group of related inflammatory skin diseases characterized by pruritusand
epidermal spongiosis (edema).
·
Acute eczema causes a vesicular,
erythematous rash.
·
Chronic eczema develops following
repetitive scratching, and is characterized by dry, thickened, hyperkeratotic
skin.
·
Atopic dermatitis is often
inherited. Defects in the keratinocyte barrier are due to mutations in the
filaggrin gene (FLG).
·
Contact dermatitis can be either
allergic type (poison ivy, nickel in jewelry) or photodermatitis type (such as
photosensitivity reaction after tetracycline).
Polymorphous
light eruption is the most common idiopathic form of photoder-matosis and
causes pruritic erythematous macules, papules, plaques, or vesicles on exposure
to sunlight. There is dermal edema and inflammation.
Verrucae
(warts) are caused by human papillomavirus. Verruca vulgaris is the
mostcommon type.
Cutaneous
lupus erythematosus may be acute (facial butterfly
rash), subacute (pho-tosensitive rash on anterior chest, upper back and upper
extremities), or chronic (dis-coid plaques, usually above the neck). Direct
immunofluorescence shows deposition of immunoglobulin and complement at the
dermal-epidermal junction. Serologies for autoantibodies and clinical correlation
help establish the diagnosis.
Erythema
multiforme is a hypersensitivity skin reaction to infections (Mycoplasmapneumoniae, herpes simplex) or
drugs (sulfonamides, penicillin, barbiturates, phe-nytoin) characterized by
vesicles, bullae, and “targetoid” erythematous lesions. The most severe form is
Stevens-Johnson syndrome, which has extensive involvement of skin and mucous
membranes.
Pityriasis
rosea
causes a pruritic rash that starts with an oval-shaped
“herald patch”and progresses to a papular eruption of the trunk to produce a
“Christmas tree” distribution. It is clinically diagnosed, self-limiting and
possibly a viral exanthem.
Granuloma
annulare is a chronic inflammatory disorder that causes papules
andplaques. Palisaded granulomas are present microscopically. The pathogenesis
is immunologic, but most cases occur in healthy patients.
Erythema
nodosum causes raised, erythematous, painful nodules of
subcutaneousadipose tissue, typically on the anterior shins, which can be
associated with granu-lomatous diseases and streptococcal infection.
Epidermoid
cyst is a common benign skin cyst lined with stratified squamous
epi-thelium and filled with keratin debris.