Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Enteric Infections and Food Poisoning
Epidemiologic Setting - Enteric Infections and Food Poisoning
EPIDEMIOLOGIC SETTING
The epidemiologic setting of the infection is of great importance in assessing the relative probability of the infectious agents. When combined with clinical findings, the differen-tial diagnosis can often be limited to two or three organisms. The major epidemiologic settings are (1) endemic infection, (2) epidemic infection, (3) traveler’s diarrhea, (4) food poisoning, and (5) hospital-associated diarrhea.
Endemic Infections
By definition, endemic diarrheas are those that occur sporadically in the usual living circumstances of the patient (from the Greek “endemos,” dwelling in a place). Some or-ganisms are endemic worldwide, whereas others are geographically limited. There are also seasonal variations and age-related attack rates within the endemic foci. In developedcountries the most common causes of endemic gastrointestinal infections are rotaviruses,caliciviruses, Campylobacter, Salmonella, and Shigella. All are more common in infantsand children because they are more prone to fecal – oral spread and because developmentof immunity is related to age. Rotaviruses account for 40 to 60% of diarrheal infectionsoccurring during the cooler months in infants and children less than 2 years of age but areuncommon in older persons.
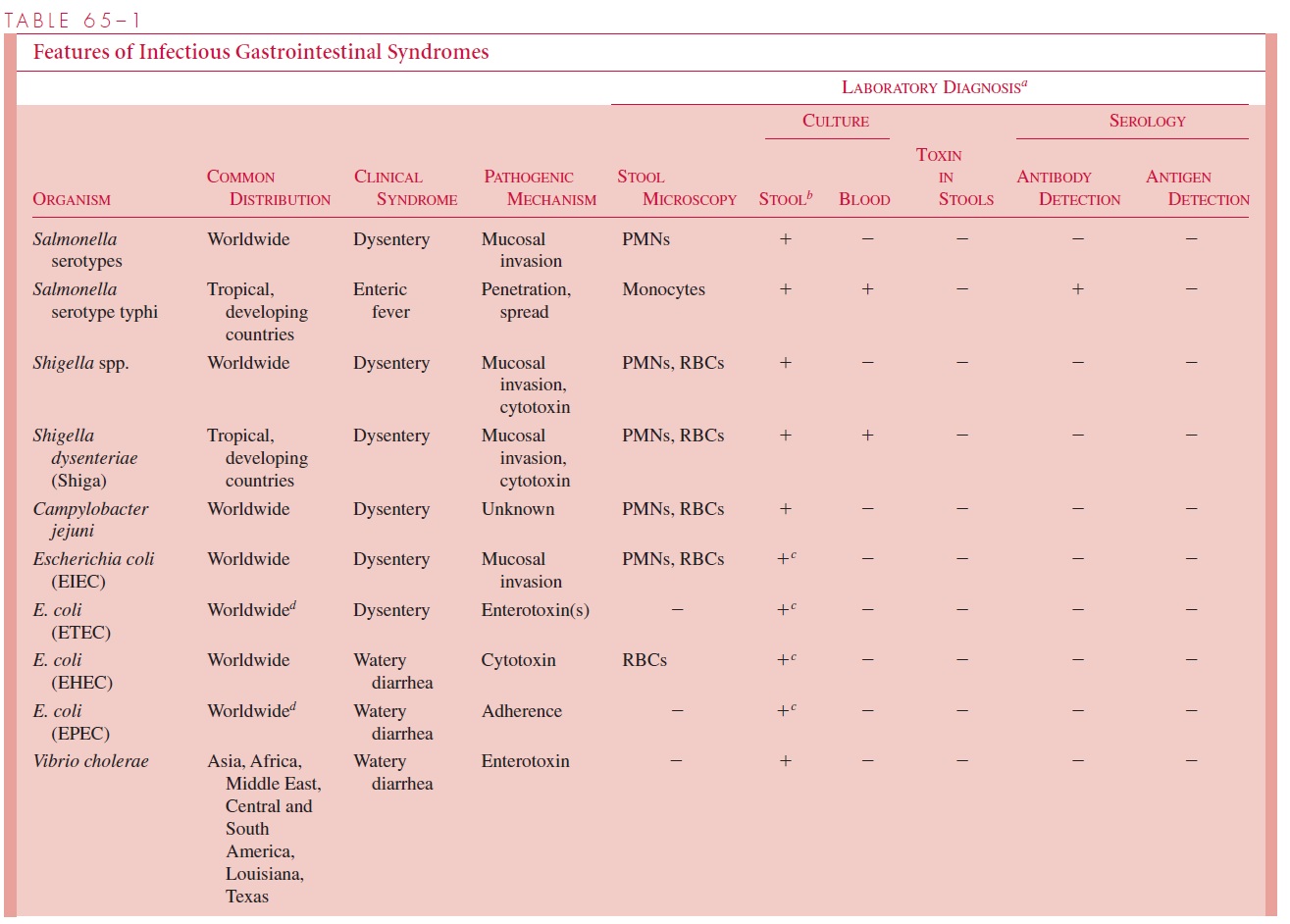
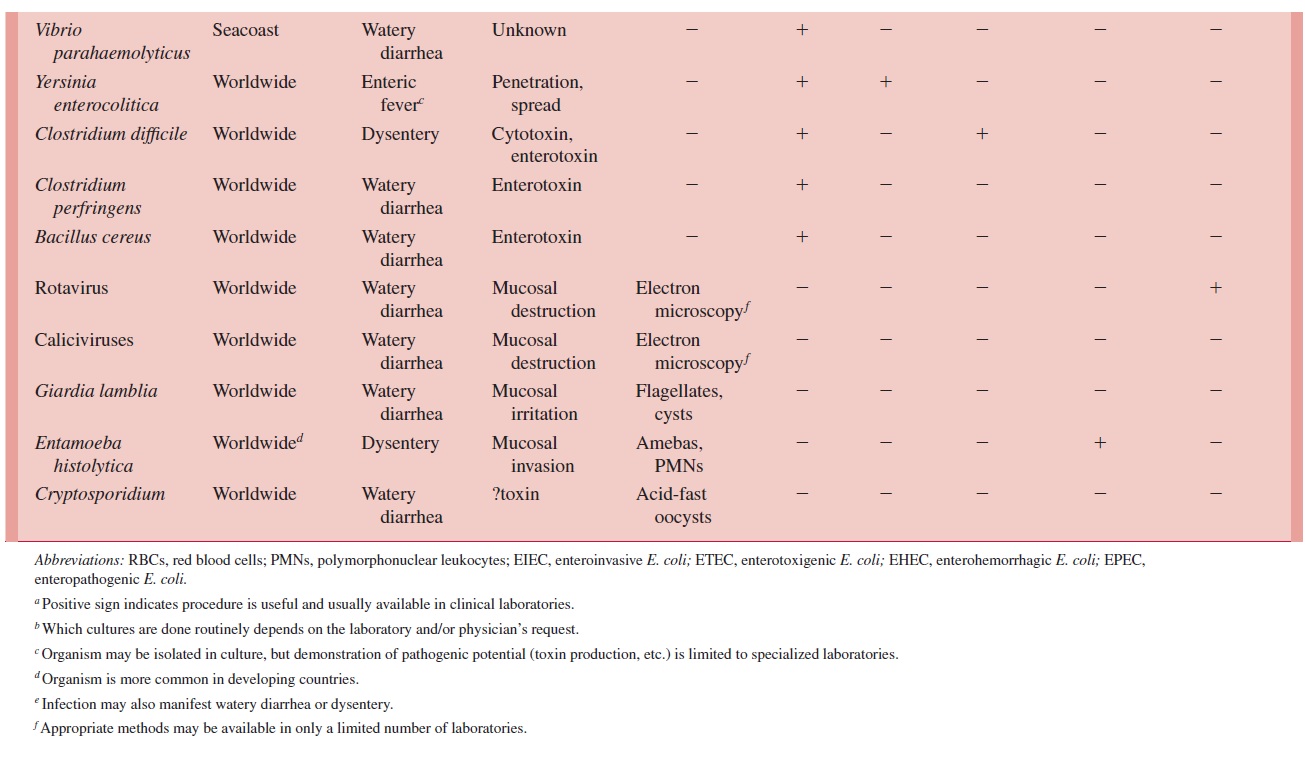
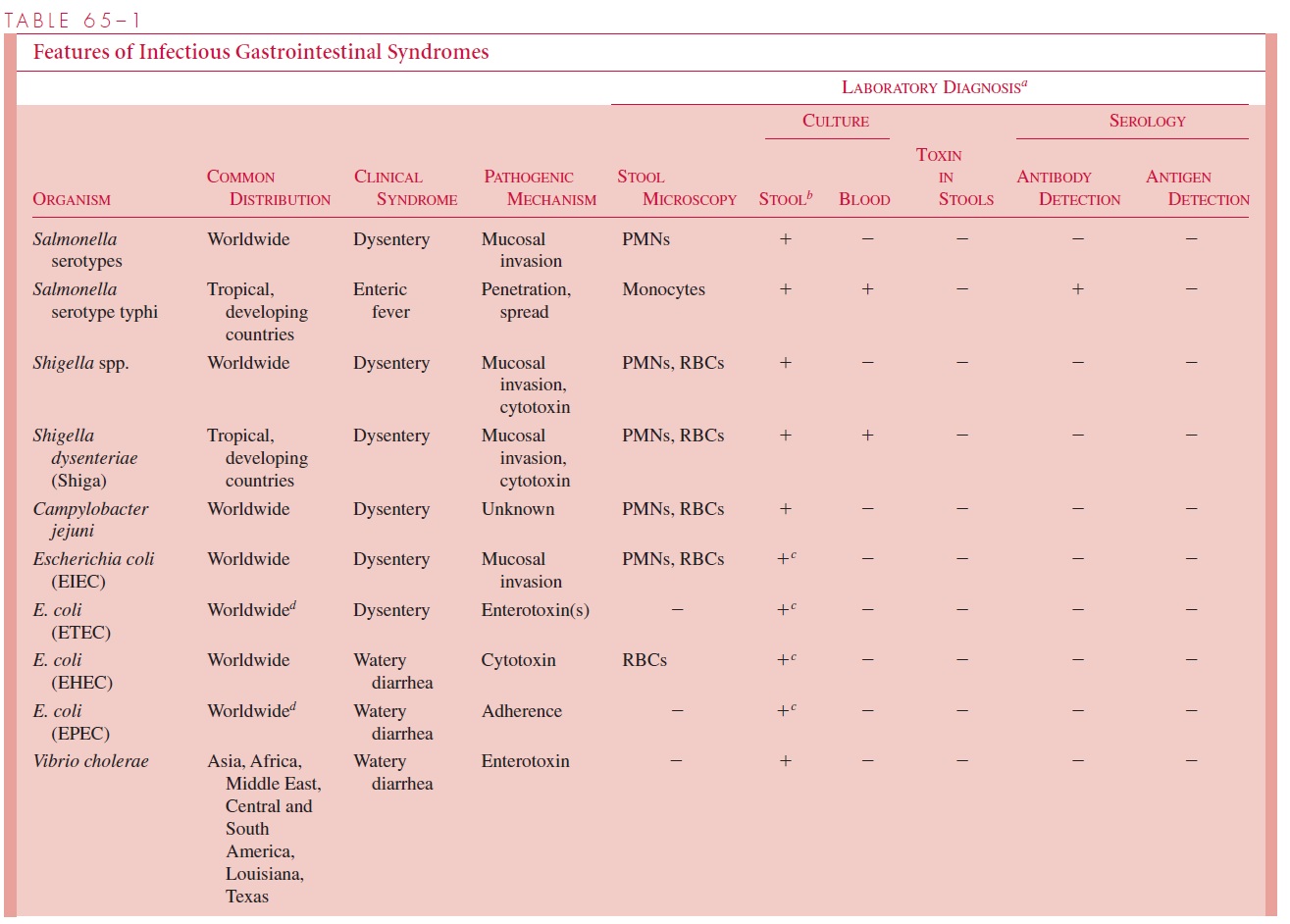
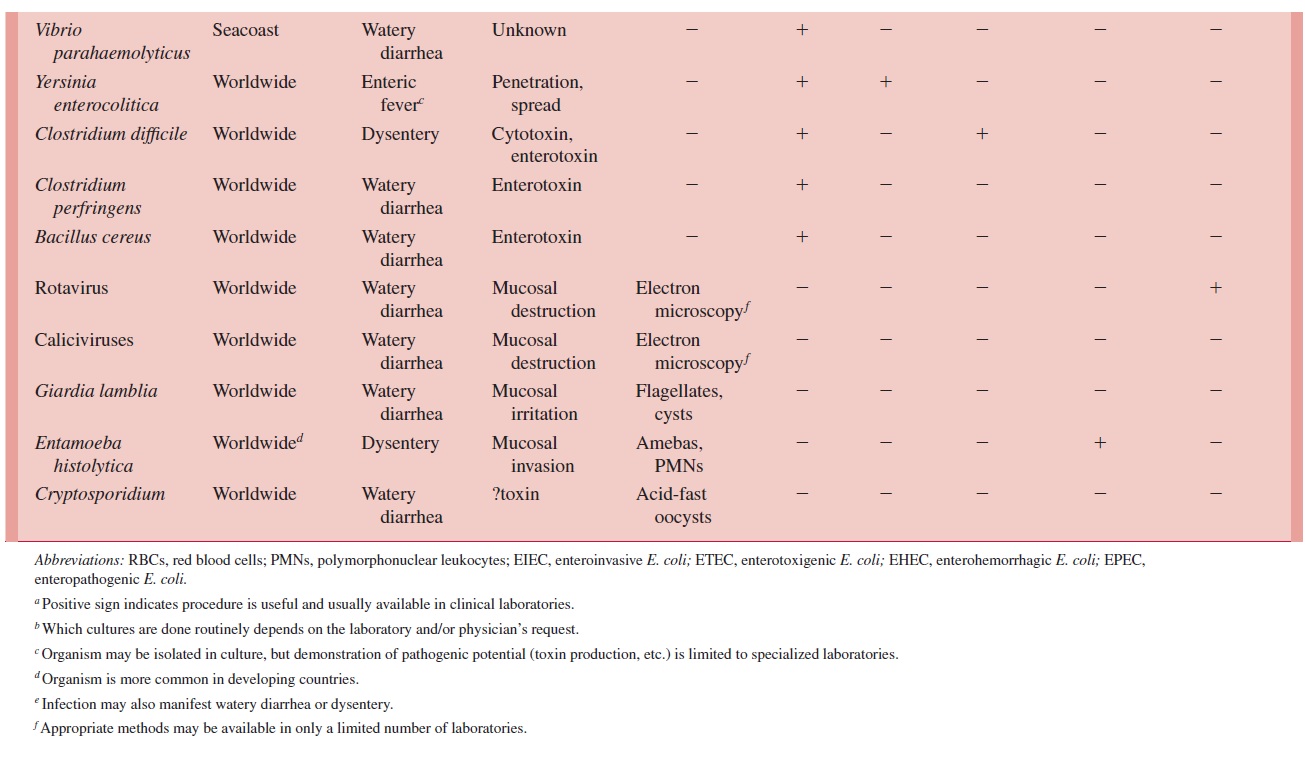
The geographically limited agents are common only in the areas listed (see Table 65 – 1). These distributions are not fixed, making it necessary to keep abreast of geo-graphic changes in the distribution of established agents as well as the recognition of new ones. For example, cholera has long been limited to warm-climate river deltas in Asia,Africa, and the Middle East, but recently it has spread to South and Central America andthe Gulf Coast of Louisiana and Texas.
Epidemic Infections
Under certain epidemiologic conditions some of the organisms responsible for endemic infections can spread beyond the family unit to cause epidemics involving regional, na-tional, and even international populations. The diarrheal diseases most frequently associ-ated with epidemics are typhoid fever, cholera, and shigellosis. For all three, epidemics are related to the failure of basic public health sanitary measures. For example, Salmo-nella serotype Typhi and Vibrio cholerae may be spread for some distance through thewater supply, a route blocked by modern sewage and water treatment practices. When these procedures are not employed or are interrupted by equipment failure or natural dis-asters (floods, earthquakes), these diseases can and do recur in epidemic form. Epidemics of shigellosis may be water-borne under the same conditions, butShigella dysentery is more typically a disease “of wars and armies, and of crowds and movement.”* The very low infecting dose of Shigella can make spreading through direct contact reach epidemic proportions when crowding and poor sanitary facilities are combined. Giardia, Cryp-tosporidium, and E. coli O157:H7 were the most frequent identified causes of recent wa-terborne epidemics in the United States.
Although such epidemics are usually associated with the 19th century, it is clear that the potential remains. In the late 1970s large epidemics of both typhoid fever and shigel-losis spread through Central and South America. In 1973 more than 200 cases of typhoid fever in Florida were associated with a defective chlorinator in the local water system. The current cholera epidemic claimed thousands of lives in South America in the last decade of the 20th century.
Traveler’s Diarrhea
From 20% to 50% of travelers from developed countries who go to less developed coun-tries experience a diarrheal illness in the first week that is usually brief but can be serious. The common names applied to this syndrome, such as “Delhi belly” and “Montezuma’s revenge,” reflect geographic associations and the cumulative frustration of those forced to spend part of their vacation next to the toilet rather than the swimming pool.
The most extensive studies of traveler’s diarrhea have involved travelers from the United States to Latin American countries, particularly Mexico. In nearly 50% of these cases, the diarrhea is caused by enterotoxigenic strains of E. coli acquired during travel. Shigella in-fections account for another 10 to 20%, and the remaining cases are attributable to various pathogens or unknown causes. Ingestion of uncooked or incompletely cooked foods is the most likely source of infection, but most epidemiologic studies have not shown specific food associations. An exception is the strong relationship between toxigenic E. coli diarrhea and the consumption of salads containing raw vegetables. “Don’t drink the water” still seems like sound advice for travelers to countries where hygiene remains poor, but the adage is not well supported by studies relating infection to water or ice consumption.
Food Poisoning
Many gastrointestinal infections involve food as a vehicle of transmission. The term “food poisoning,” however, is usually reserved for instances in which a single meal can be incriminated as the source. This situation typically arises when multiple cases of the same gastrointestinal syndrome develop at the same time among persons whose only common experience is a meal shared at a social event or restaurant. The probable etio-logic agent can usually be assessed from knowledge of the incubation period, the food ve-hicle, and the clinical findings. Changes in the importation, processing, and distribution of foods have increased the complexity and potential for food-borne transmission of en-teric pathogens. Outbreaks that in the past might have been limited, may now be widely distributed by fast-food chains or airline catering services.
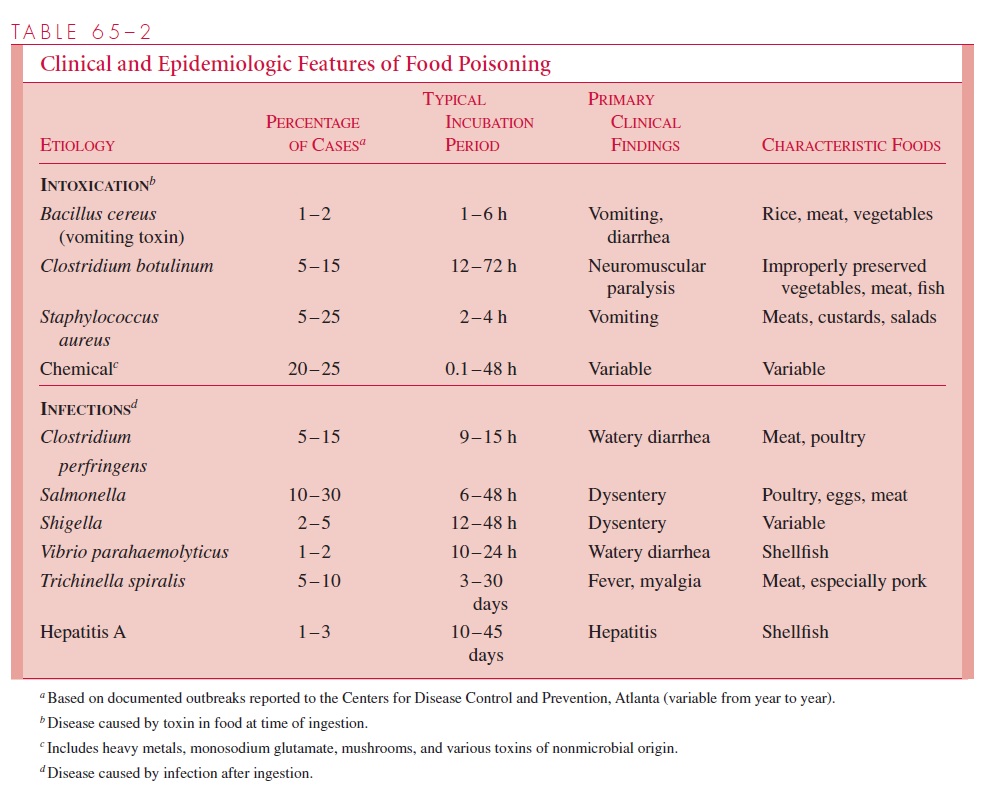
The most common causes of food poisoning are shown in Table 65 – 2. Some are not infections but intoxications, caused by ingestion of a toxin produced by bacteria in the food before it was eaten. Intoxications have shorter incubation periods than infections and may involve extraintestinal symptoms (eg, the neurologic damage in botulism). Infectious food poisoning does not differ from endemic diarrheal infections caused by the same species. The length of the incubation period and the severity of the symptoms are gener-ally related to the number of organisms ingested.
The epidemiologic circumstances of food poisoning vary with the etiologic agent but virtually always involve a breach in the recommended procedures for handling food. The organisms may be present as contaminants in raw food before cooking or introduced by a carrier or contaminated utensil involved in preparation.
Causes of bacterial food poisoning include failure to kill the organisms by adequate cooking, almost always followed by a pe-riod of warming (incubation) long enough for the organisms to multiply to infectious num-bers or, in the case of toxigenic disease, to produce sufficient toxin to cause disease. In 80 to 90% of investigated outbreaks of bacterial food poisoning, the most important contribut-ing factor is the use of improper storage temperatures for the food. This factor may obtain in home-cooked meals as well as those prepared in restaurants, in schools, or at large so-cial events such as community picnics.
The relative frequency of each etiologic agent and the foods most frequently involved are also shown in Table 65 – 2. This information is based on outbreaks investigated by public health agencies, but it is generally accepted that these represent the “tip of the iceberg” due to underreporting. Large outbreaks, restaurant-associated outbreaks, and outbreaks involving serious illness with hospitalization or death are more likely to be reported to health authori-ties than are mild diarrheas after a dinner party or airline meal. In recent years, of the 400 to 500 outbreaks (10,000 to 15,000 cases) reported each year in the United States, fewer than 200 are “solved.” Food poisoning characterized by a short incubation period (eg Staphylo-coccus aureus) is more likely to be recognized because it can easily be associated with a spe-cific meal and because the food itself may still be available for examination. There are also large geographic differences in reporting. For example, in 1979, New York City, in which 50% of the state population resides, reported 98% of New York state’s food-borne outbreaks, and Connecticut reported more outbreaks than all of the southeastern states combined.
Sampling problems aside, the food poisoning syndromes listed in Table 65 – 2 are well recognized, with Salmonella, Clostridium perfringens, and S. aureus accounting for more than 70% of those for which a microbial etiology can be found. For bacterial infections such as Salmonella and Shigella, which are not normal members of the stool flora, establishing the diagnosis by isolating the causative organism is relatively easy. If the circumstances indicate C. perfringens or S. aureus food poisoning, investi-gation involves cultures of vomitus, stool from several cases, and the suspect food. In some cases, toxin detection is required to establish the etiology and source. Such in-vestigations are best coordinated by public health authorities, who can also address the legal and community implications of the outbreak. For example, one investigation ofSalmonella food poisoning led to the discovery that the owner of a restaurant waskeeping and slaughtering chickens at the restaurant. Although this practice may have provided very fresh chicken, it guaranteed Salmonella contamination of the entire kitchen.
Hospital-associated Diarrhea
The hospital environment should not allow spread of the usual causes of endemic intesti-nal infection. When such infection occurs, it can usually be traced to an employee who continues working while ill or to contaminated food prepared outside the hospital that is “smuggled” in by the patient’s friends. Two special causes of hospital-associated diarrhea are caused by E. coli in infants and Clostridium difficile in patients treated with antimi-crobial agents. Fortunately, E. coli outbreaks have become rare.C. difficile accounts for more than 90% of cases of a syndrome that ranges from mild diarrhea to fulminant pseudomembranous colitis during or after treatment with antibiotics. The responsible tox-igenic C. difficile may be resident in the patient’s intestinal flora before administration of antimicrobics or be acquired by spread from other patients in the hospital. Rotaviruses can also cause hospital outbreaks in infants.
Related Topics