Chapter: Essentials of Psychiatry: Childhood Disorders: Elimination Disorders and Childhood Anxiety Disorders
Encopresis
Encopresis
Definition
Encopresis is usually defined as the intentional or
involuntary passage of stool into inappropriate places in the absence of any
identified physical abnormality in children older than 4 years. It may not be
attributable to a medical condition and must occur at least monthly for a
period of three months. The distinction is drawn between encopresis with
constipation (retention with over-flow based on history or physical
examination) and encopresis without constipation. Other classification schemes
include mak-ing a primary–secondary distinction (based on having a 1-year
period of continence) or soiling with fluid or normal feces.
Course and Natural History
Less than one-third of children in the USA have
completed toilet training by the age of 2 years with a mean age of 27.7 months.
Bowel control is usually achieved before bladder control.
The age cutoff for “normality” is set at 4 years,
the age at which 95% of children have acquired fecal continence (Stein and
Susser, 1967). As with urinary continence, girls achieve bowel control earlier
than boys.
Epidemiology
The overall prevalence of encopresis in 7- and
8-year-old children has been shown to be 1.5%, with boys (2.3%) affected more
com-monly than girls (0.7%). There was a steadily rising likelihood of continence
with increasing age, until by age 16 years the re-ported prevalence was almost
zero. Rutter and coworkers (1970) reported a rate of 1% in 10- to 12-year-old
children, with a strong (5 : 1) male/female ratio. Retrospective study of
clinic-referred en-copretic children has shown that 40% of cases are primary
(true failure to gain control), with a mean age of 6.7 years, and 60% of cases
are secondary, with a mean age of 8 years (Levine, 1975). Eighty percent of
patients were constipated, with no difference in this feature seen between
primary and secondary subtypes.
Etiology and Pathophysiology
Within the first year of life, children can show a tendency toward constipation,with concordance for constipation being six times more frequent in monozygotic than in dizygotic twins. Fecal retention and reduced stool frequency between 12 and 24 months of age can predict later encopresis. Encopretic children with constipation and overflow are found to have rectal and colonic distention, massive impaction with hard feces and a number of specific abnormalities of anorectal physiology. These abnor-malities, which may be primary or secondary to constipation, include elevated anal resting tone, decreased anorectal motility and weakness of the internal anal sphincter, and dysfunction of the external anal sphincter. Encopresis may occur after an acute episode of constipation following illness or a change in diet. In addition to the pain caused by attempts to pass an extremely hard stool, a number of specific painful perianal conditions such as anal fissure can lead to stool withholding and later fecal soiling. Stressful events such as the birth of a sibling or attending a new school have been associated with up to 25% of cases of secondary encopresis. In nonretentive encopresis, the main theories center on faulty toilet training. Stress during the training period, co-ercive toileting leading to anxiety and “pot phobia”, and failure to learn or to have been taught the appropriate behavior have all been implicated. True fecal urgency, which may have a physi-ological or pathological basis, may also be important in a small proportion of cases (Woodmansey, 1967).
Diagnosis and Differential Diagnosis
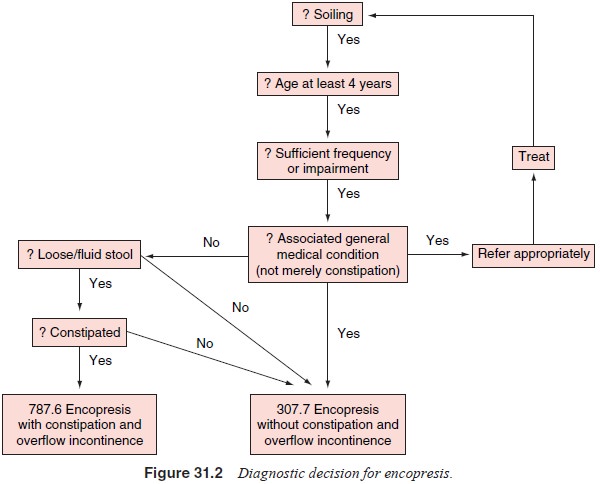
The main efforts during the diagnostic process are
to establish the presence or absence of constipation and, to a lesser extent,
distinguish continuous (primary) from discontinuous (second-ary) soiling
(Figure 31.2). Taylor and Hersov (1994) listed three types of identifiable
encopresis in children: 1) it is known that the child can control defecation,
but she or he chooses to defecate in inappropriate places; 2) there is true
failure to gain bowel con-trol, and the child is unaware of or unable to
control soiling; and 3) soiling is due to excessively fluid feces, whether from
constipa-tion and overflow, physical disease, or anxiety. In practice, there is
frequently overlap among types or progression from one to an-other. Unlike
enuresis, fecal soiling rarely occurs at night or dur-ing sleep, and if
present, is indicative of a poor prognosis. Soiling due to anal masturbation
has been reported, although this causes staining of the sheets rather than full
stools in the bedclothes.
Phenomenology
In the first group, in which bowel control has been
established, the stool may be soft or normal (but different from fluid-type
feces seen in overflow). Soiling due to acute stress events (e.g., the birth of
a sibling, a change of school, or parental separation) is usually brief once
the stress has abated, given a stable home environment and sensible management.
In more severe patho-logical family situations, including punitive management
or frank physical or sexual abuse (Boon, 1991), the feces may be deposited in
places deliberately to cause anger or irritation, or there may be associated
smearing of feces on furniture and walls. Other covert aggressive antisocial
acts may be evident, with considerable denial by the child of the magnitude or
seri-ousness of the problem.
In the second group, in which there is failure to
learn bowel control, a nonfluid stool is deposited fairly randomly in clothes,
at home and at school. There may be conditions such as mental retardation or
specific developmental delay, spina bifida, or cerebral palsy that impair the
ability to recognize the need to defecate and the appropriate skills needed to
defer this function until a socially appropriate time and location. In the
absence of low IQ or pathological physical condition, patients have been
re-ported as having associated enuresis, academic skills problems and
antisocial behavior. They present to pediatricians primarily and are usually
younger (age 4–6 years) than other encopretic individuals. It is thought that
this type of soiling is considerably more common in socially disadvantaged,
disorganized families because of stressful, faulty or inconsistent training.
In the third group, excessively fluid feces are passed, which may result from conditions that cause true diarrhea (e.g., ulcera-tive colitis) or, much more frequently, from constipation with overflow causing spurious diarrhea. A history of retention, either willful or in response to pain, is prominent in the early days of this form of encopresis, although later it may be less apparent be-cause of fecal overflow. Behavior such as squatting on the heels to prevent defecation or marked anxiety about the prospect of using the toilet (although rarely amounting to true phobic avoid-ance) may be described.
Issues and Further Assessment
The comprehensive assessment process should include
a medical evaluation, psychiatric and family interviews, and a systematic
behavioral recording.
The medical evaluation comprises a history, review
of systems, physical examination, and appropriate hematological and
radiological tests. Although the vast majority of patients with encopresis are
medically normal, a small proportion have pathological features of etiological
significance. Physical causes of encopresis without retention include
inflammatory bowel dis-ease (e.g., ulcerative colitis, Crohn’s disease),
central nervous system disorders, sensory disorders of the anorectal region or
pelvic floor muscles (e.g., spina bifida, cerebral palsy). Organic causes of
encopresis with retention include Hirschsprung’s dis-ease (aganglionosis in
intermuscular and submucous plexuses of the large bowel extending proximally
from the anus), neurogenic megacolon, hypothyroidism, hypercalcemia, chronic
codeine or laxative usage, anorectal stenosis and fissure. It should also be
remembered that these conditions rarely have their first presenta-tion with
encopresis alone.
The physical assessment should include an abdominal
and rectal examination, although a plain abdominal radiograph is the most
reliable way to determine the presence of fecal impaction. Anorectal manometry
should be considered in the investigation of children with severe constipation
and chronic soiling, espe-cially those in whom Hirschsprung’s disease is
suspected.
Psychiatric and family interviews should include a
devel-opmental history and a behavioral history of encopresis (ante-cedents,
behavior and consequences). Specific areas of stress, acute or chronic,
affecting the child or family, or both, should be discovered. Associated
psychopathological conditions are more commonly found in the older child, in
secondary encopresis, and when soiling occurs not only in clothes. Anxiety
surrounding toileting may indicate pot phobia, coercive toileting, or a
his-tory of painful defecation. A history should be obtained of the parents’
previous attempts at treatment together with previously prescribed therapy so
that reasons for previous failure can be identified and anticipated in future
treatment planning.
Treatment
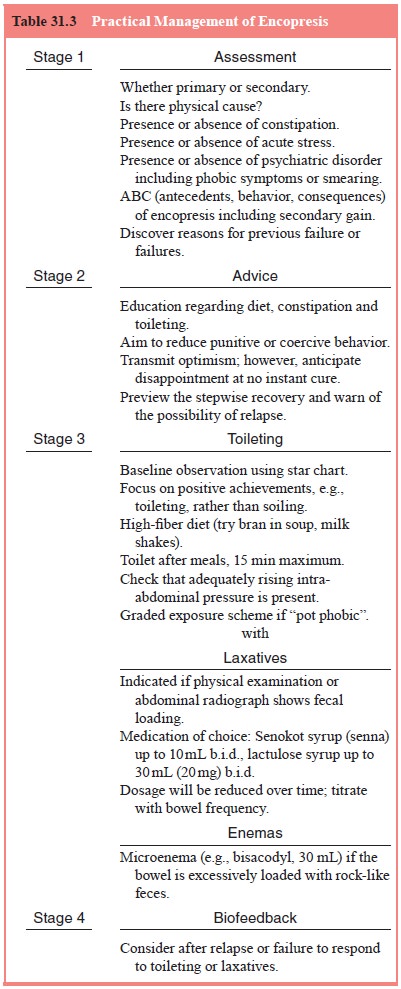
Practical management for encopresis is presented in
Table 31.3.
Standard Treatment
The principal approach to treatment is predicated
on the results of the evaluation and the clinical category assigned. This
differenti-ates between the need to establish a regular toileting procedure in
patients in whom there has been a failure to learn this social behavior and the
need to address a psychiatric disorder, par-ent–child relationship
difficulties, or other stresses in the child who exhibits loss of this
previously acquired skill in association with these factors. In both cases,
analysis of the soiling behavior may identify reinforcing factors important in
maintaining dys-function. Detection of significant constipation will, in
addition, provide an indication for adjuvant laxative therapy.
Behavioral Treatments
Behavioral therapy is the mainstay of treatment for encopresis. In the younger child who has been toilet trained, this focuses on practical elimination skills, for example, visiting the toilet after each meal, staying there for a maximum of 15 minutes, using muscles to increase intra-abdominal pressure and cleaning one-self adequately afterward. Parents or caretakers, or both, need to be educated in making the toilet a pleasant place to visit and should stay with the younger child, giving encouragement and praise for appropriate effort. Small children whose legs may dangle above the floor should be provided with a step against which to brace when straining. Initially, a warm bath before us-ing the toilet may relax the anxious child and make it easier to pass stool. Systematic recording of positive toileting behavior, not necessarily being clean (depending on the level of baseline behavior), should be performed with a personal star chart. For the child with severe anxiety about sitting on the toilet, a graded exposure scheme may be indicated.
Role of the Family in Treatment
Removing
the child’s and family’s attention from the encopresis alone and focusing onto
noticing, recording and rewarding positive behavior often defuses tension and
hostility and provides the opportunity for therapeutic improvement. Identifying
and eliminating sources of secondary gain, whereby soiling is reinforced by
parental (or other individuals’) actions and attention, even if negative or
punitive, make positive efforts more fruitful. Some investigators advocate mild
punishment techniques, such as requiring the child to clean his or her own
clothes after soiling, although care must be taken to prevent this from
becoming too punitive. In certain settings, particularly school, attempts are
made to prevent soiling by extremely frequent toileting that, although keeping
the child clean, does not promote and may even hinder the acquisition of a
regular bowel habit. Formal therapy, either individual or family based, is
indicated in only a minority of patients with an associated psychiatric
disorder, marked behavioral disturbance, or clear remediable family or social
stresses.
Physical Treatments
In
patients with retention leading to constipation and overflow, medical
management is nearly always required, although it is usually with oral
laxatives or microenemas alone. The use of more intrusive and invasive colonic
and rectal washout or sur-gical disimpaction procedures is nearly always the
result of the clinician’s impatience rather than true clinical need.
Uncontrolled
studies of combined treatment with behav-ioral therapy and laxatives reported
marked improvement in symptoms (not cure) in approximately 70 to 80% of
patients. A more recent controlled randomized trial (Nolan et al., 1991) com-paring behavioral therapy in retentive primary
encopresis with and without laxatives showed that at 12-month follow-up, 51% of
the combined treatment (laxative plus behavioral therapy) group had achieved
remission (at least one 4-week period with no soil-ing episodes), compared with
36% of the behavioral therapy only group (P
5 0.08).
Partial remission (soiling no more than once a week) was achieved in 63% of
patients with combined therapy versus 43% with behavioral therapy alone (P 5 0.02). Patients receiving
laxatives achieved remission significantly sooner, and the difference in the
Kaplan–Meier remission curves was most striking in the first 30 weeks of
follow-up (P 5 0.012).
When patients who were not compliant with the toileting program were removed
from the analysis, however, the advantage of combined therapy was not
significant. These results must also be viewed in light of a 50% spontaneous
remission rate at 2 years reported in some studies.
Biofeedback Therapy
The
finding that some children with treatment-resistant retentive encopresis
involuntarily contract the muscles of the pelvic floor and the external anal
sphincter, effectively impeding passage of stool, has led to efforts to use
biofeedback in this instance. It has similarly been reported that as few as six
sessions of bio-feedback therapy can lead to a significant reduction in symptom
frequency for as many as 86% of previously treatment-resistant patients
(Loening-Baucke, 1995). It is possible, however, that bio-feedback is
principally of benefit to nonretentive chronic soilers (van Ginkel et al., 2000).
Related Topics