Chapter: Medical Physiology: Cardiac Failure
Edema in Patients with Cardiac Failure
Edema in Patients with Cardiac Failure
Inability of Acute Cardiac Failure to Cause Peripheral Edema.
Acute left heart failure can cause terrific and rapid congestion of the lungs, with development of pul-monary edema and even death within minutes tohours.
However, either left or right heart failure is very slow to cause peripheral edema. This can best be explained by referring to Figure 22–3. When a previ-ously healthy heart acutely fails as a pump, the aortic pressure falls and the right atrial pressure rises. As the cardiac output approaches zero, these two pressures approach each other at an equilibrium value of about 13 mm Hg. Capillary pressure also falls from its normal value of 17 mm Hg to the new equilibrium pressure
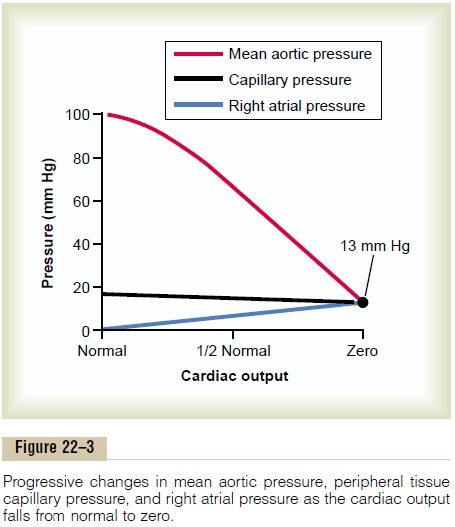
of 13 mm Hg. Thus, severe acute cardiac failure oftencauses a fall in peripheral capillary pressure rather than a rise. Therefore, animal experiments, as well as expe-rience in humans, show that acute cardiac failure almost never causes immediate development of peri-pheral edema.
Long-Term Fluid Retention by the Kidneys— The Cause of Peripheral Edema in Persisting Heart Failure
After the first day or so of overall heart failure or of right-ventricular heart failure, peripheral edema does begin to occur principallybecause of fluid retention bythe kidneys. The retention of fluid increases the meansystemic filling pressure, resulting in increased ten-dency for blood to return to the heart. This elevates the right atrial pressure to a still higher value and returns the arterial pressure back toward normal. Therefore, the capillary pressure now also risesmarkedly, thus causing loss of fluid into the tissues anddevelopment of severe edema.
There are three known causes of the reduced renal output of urine during cardiac failure, all of which are equally important but in different ways.
1. Decreased glomerular filtration. A decrease incardiac output has a tendency to reduce the glomerular pressure in the kidneys because of (1) reduced arterial pressure and (2) intensesympathetic constriction of the afferent arterioles of the kidney. As a consequence, except in themildest degrees of heart failure, the glomerular filtration rate becomes less than normal. That even a slight decreasein glomerular filtration often markedly decreases urine output. When the cardiac output falls toabout one-half normal, this can result in almost complete anuria.
2. Activation of the renin-angiotensin system and increased reabsorption of water and salt by the renal tubules. The reduced blood flow to thekidneys causes marked increase in renin secretion by the kidneys, and this in turn causes the formation of angiotensin. The angiotensin in turn has a direct effect on the arterioles of the kidneys to decrease further the blood flow through the kidneys, which especially reduces the pressure in the capillaries surrounding the renal tubules, promoting greatly increased reabsorption of both water and salt from the tubules. Therefore, loss of water and salt into the urine decreases greatly, and large quantities of salt and water accumulate in the blood and interstitial fluids everywhere in the body.
3. Increased aldosterone secretion. In the chronicstage of heart failure, large quantities of aldosterone are secreted by the adrenal cortex. This results mainly from the effect of angiotensin to stimulate aldosterone secretion by the adrenal cortex. But some of the increase in aldosterone secretion often results from increased plasma potassium. Excess potassium is one of the most powerful stimuli known for aldosterone secretion, and the potassium concentration rises in response to reduced renal function in cardiac failure.
The elevated aldosterone level further increases the reabsorption of sodium from the renal tubules. This in turn leads to a secondary increase in water reabsorption for two reasons: First, as the sodium is reabsorbed, it reduces the osmotic pressure in the tubules but increases the osmotic pressure in the renal interstitial fluids; these changes promote osmosis of water into the blood. Second, the absorbed sodium and anions that go with the sodium, mainly chloride ions, increase the osmotic concentration of the extracellular fluid everywhere in the body. This elicits antidiuretic hormone secretion by thehypothalamic–posterior pituitary gland system. The antidiuretic hormone in turn promotes still greater increase in tubular reabsorption of water.
Role of Atrial Natriuretic Factor to Delay Onset of Cardiac Decompensation. Atrial natriuretic factor (ANF)is ahormone released by the atrial walls of the heart when they become stretched. Because heart failure almost always causes excessive increase in both the right and left atrial pressures that stretch the atrial walls, the cir-culating levels of ANF in the blood increase fivefold to tenfold in severe heart failure. The ANF in turn has a direct effect on the kidneys to increase greatly their excretion of salt and water. Therefore, ANF plays a natural role to help prevent extreme congestive symp-toms during cardiac failure.
Acute Pulmonary Edema in Late-Stage Heart Failure—Another Lethal Vicious Circle
A frequent cause of death in heart failure is acute pul-monary edema occurring in patients who have alreadyhad chronic heart failure for a long time. When this occurs in a person without new cardiac damage, it usually is set off by some temporary overload of the heart, such as might result from a bout of heavy exer-cise, some emotional experience, or even a severe cold. The acute pulmonary edema is believed to result from the following vicious circle:
1. A temporarily increased load on the already weak left ventricle initiates the vicious circle. Because of limited pumping capacity of the left heart, blood begins to dam up in the lungs.
2. The increased blood in the lungs elevates the pulmonary capillary pressure, and a small amount of fluid begins to transude into the lung tissues and alveoli.
3. The increased fluid in the lungs diminishes the degree of oxygenation of the blood.
4. The decreased oxygen in the blood further weakens the heart and also weakens the arterioles everywhere in the body, thus causing peripheral vasodilation.
5. The peripheral vasodilation increases venous return of blood from the peripheral circulation still more.
6. The increased venous return further increases the damming of the blood in the lungs, leading to still more transudation of fluid, more arterial oxygen desaturation, more venous return, and so forth. Thus, a vicious circle has been established.
Once this vicious circle has proceeded beyond a certain critical point, it will continue until death of the patient unless heroic therapeutic measures are used within minutes. The types of heroic therapeutic meas-ures that can reverse the process and save the patient’s life include the following:
1. Putting tourniquets on both arms and legs to sequester much of the blood in the veins and, therefore, decrease the workload on the left side of the heart
2. Bleeding the patient
3. Giving a rapidly acting diuretic, such as furosemide, to cause rapid loss of fluid from the body
4. Giving the patient pure oxygen to breathe to reverse the blood oxygen desaturation, the heart eterioration, and the peripheral vasodilation
5. Giving the patient a rapidly acting cardiotonic drug, such as digitalis, to strengthen the heart
This vicious circle of acute pulmonary edema can proceed so rapidly that death can occur in 20 minutes to 1 hour. Therefore, any procedure that is to be suc-cessful must be instituted immediately.
Related Topics