Chapter: Modern Pharmacology with Clinical Applications: Drug Metabolism and Disposition in Pediatric and Gerontological Stages of Life
Drug Disposition in Geriatric Patients
DRUG DISPOSITION
IN GERIATRIC PATIENTS
The elderly (individuals over
65 years of age) constitute more than 13% of the population. This figure is
increas-ing steadily and is expected to reach 50 million by the year 2020. This
segment of our society is the most highly drug-treated and accounts for about
25% of prescrip-tion drugs dispensed. The average Medicare patient in an
acute-care hospital receives approximately 10 differ-ent drugs daily, and this
translates into a higher inci-dence of adverse drug reactions in geriatric
patients than in the general population.
Chronological aging may not
necessarily be an accu-rate index of biological aging, which is the result of
many genetic and environmental factors. While most 20-year-olds have a similar
response to a given drug, it is difficult to predict the response among
80-year-olds. A clear relationship between the appearance of untoward effects
to drugs and aging has been demonstrated only for about 10 drugs. For some 90
other drugs in common clinical use, age alone was not a major determinant of
clinical toxicity. It is apparent that an increase in life span is accompanied
by an increase in chronic illnesses such as hypertension, congestive heart
failure, arthritis, and diabetes. The pharmacological management of these
conditions, especially when the same person has several diseases, becomes
increasingly complex.
Age-related alterations in
pharmacokinetics (ab-sorption, distribution, metabolism, and excretion) have
received considerable attention. Thus, physiological changes in elderly
patients, when taken together, may contribute to impairments in drug clearance
in this seg-ment of the population (Table 6.5).
Absorption
Elderly patients may absorb
drugs less completely or more slowly because of decreased splanchnic blood flow
or delayed gastric emptying. Reduced gastric acidity may decrease the
absorption of drugs that require high acidity.
Distribution
Drug distribution in elderly patients may be altered by hypoalbuminemia, qualitative changes in drug-binding sites, reductions in relative muscle mass, increases in the proportion of body fat, and decreases in total body water. The plasma level of free, active drug is often a di-rect function of the extent of drug binding to plasma proteins. There is a well-documented age-dependent decline (about 20%) in plasma albumin concentration in humans due to a reduced rate of hepatic albumin synthesis.
These changes in
serum albumin may affect the free drug concentration for a number of highly
bound drugs, such as phenytoin, warfarin, and meperidine.
Metabolism
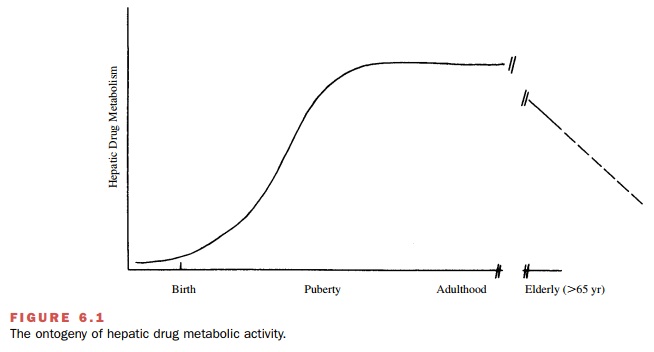
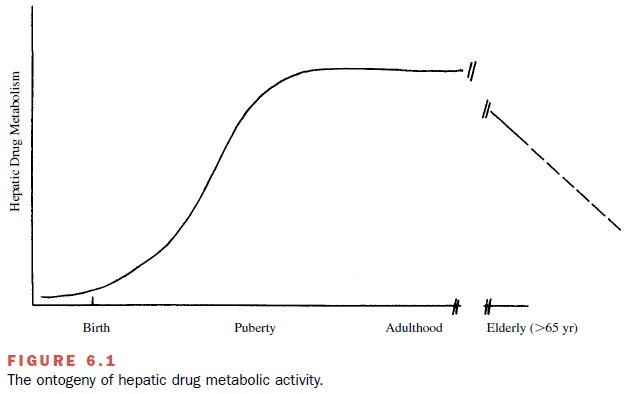
In addition to changes in
metabolism that occur as a re-sult of reduced hepatic enzyme activity,
metabolism may be impaired by a reduction in hepatic mass, vol- ume, and blood
flow (Fig. 6.1). Phase I oxidative path-ways are decreased with age, while
phase II conjugation pathways are unchanged.
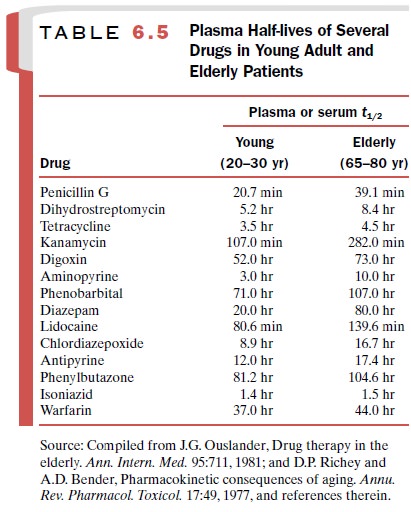
In a carefully controlled
clinical study, the plasma half-life of diazepam (Valium), a widely used
antianx-iety agent, exhibited a striking age dependency. In pa-tients aged 20
years, the t1/2was about 20 hours, and this increased linearly with
age to about 90 hours at 80 years. Half-lives of other drugs in young and old
pa-tients are presented in Table 6.5. These data demon-strate changes in drug
half-life with increasing age, suggesting that at least for some drugs, elderly
patients have reduced metabolism, drug clearance, or both.
Excretion
Renal elimination of foreign
compounds may change dramatically with increasing age by factors such as
re-duced renal blood flow, reduced glomerular filtration rate, reduced tubular
secretory activity, and a reduction in the number of functional nephrons. It
has been esti-mated that in humans, beginning at age 20 years, renal function declines
by about 10% for each decade of life. This decline in renal excretion is
particularly important for drugs such as penicillin and digoxin, which are
elim-inated primarily by the kidney.
Adverse Drug Effects
The incidence of iatrogenic complications is three to five times greater in the elderly than in the general pop-ulation. Adverse drug reactions account for 20 to 40% of these complications. Inappropriate drug use has been noted in almost half of hospitalized elderly patients. One-fourth of these patients were receiving contraindi-cated drugs, and three-fourths were receiving unnecessary drugs. Half of adverse drug reactions occur in pa-tients receiving inappropriate drugs.
Delirium and cognitive
impairment are common ad-verse reactions in the elderly. While almost every
class of drugs has the potential to produce delirium in the elderly, it is most
frequent with psychoactive drugs. The risk increases with the number of drugs
the patient is re-ceiving, reaching a 14-fold increase in risk for patients
taking more than 6 drugs.
Special Considerations
The following should be
considered when prescribing drugs for elderly patients.
Drugs should be prescribed
only if nonpharmaco-logical techniques are ineffective, such as for problems
like sleeplessness and anxiety. When drugs are pre-scribed for these
conditions, they should be given for a limited time and the patient closely
monitored for ad-verse effects. Dosage should start at or below the lowest
recommended levels.
Keep it simple. Prescribe
drugs only if you have available extensive experience and prescribing
informa-tion for that drug in elderly patients. Use the least num-ber of drugs
and doses per day Reevaluate the continued use of all medications the patient
is receiving, including over-the-counter medica-tions, on a regular basis.
Noncompliance is a
significant problem, with almost 50% of elderly patients failing to take their
medications as prescribed. Some of the reasons for noncompliance are inability
to pay for the drug, side effects, mental impair-ment, and inability to
understand complex instructions.
Related Topics