Chapter: Medical Immunology: Transplantation Immunology
Donor-Recipient Matching - Transplantation Immunology
DONOR-RECIPIENT MATCHING
Prevention of rejection is more desirable than trying to treat established rejection and is achieved by careful matching of donor and recipient and by manipulation of the recipient’s immune response. Avoidance of antigenic differences between the donor and recipient is a crucial factor for the success of a transplant. Although many different antigenic systems show allotypic variation, in transplantation practice only the ABO blood groups and the HLA system are routinely typed.
ABO incompatibility is generally considered an insurmountable obstacle to trans-plantation since it leads to an accelerated rejection response, called hyperacute rejection , probably because A and B antigens are expressed on vascular endothelium. How-ever, some groups have reported successful grafting of HLA-compatible but ABO-incom-patible organs after removing anti-A and/or anti-B isohemagglutinins by plasmapheresis or by extracorporeal immunoadsorption. In extremely urgent cases of liver transplantation, ABO matching is sometimes ignored, and reasonable graft function and survival can be seen.
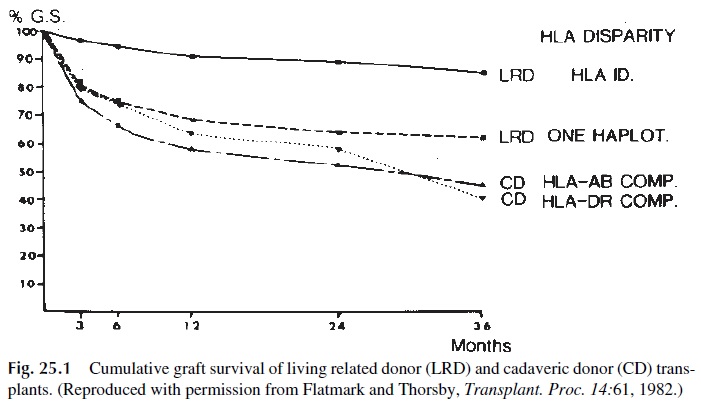
HLA matching is done routinely with the goal of matching donor and recipient as well as possible. However, the practical significance of HLA matching varies depending on the organ to be transplanted. In kidney transplantation HLA matching is considered important, since there is a positive correlation between the number of HLA antigens common to the donor and recipient and the survival of the transplanted kidney. When grafting kidneys from living relatives, HLA-identical sibling grafts have the best outcome, followed by hap-loidentical grafts, which in turn do better than two haplotype-incompatible grafts (Fig. 25.1). Cadaveric transplants matched for HLA-A, B, and DR achieve survivals similar to those ob-tained with transplants between two haplotype-matched living related individuals. Data demonstrating that kidney transplants matched only for HLA-B and HLA-DR have an ex-cellent outcome (83% graft survival at 12 months) support the significance of MHC-II typ-ing. MHC class II matching appears also to be important for survival of pancreatic grafts.
It is also important to check for cytotoxic antibodies in the recipient’s serum directed against the donor’s lymphocytes, as this could be a sign that the recipient is already immune to a potential donor. This is achieved by means of a test called a cross-match. The recipi-ent’s serum is tested against lymphocytes from the potential donor(s) and against a cell panel of known phenotypes. This test is useful to prevent rapid rejection of the grafted tis-sue or organ.
In bone marrow transplantation HLA typing is also very important, but this type of transplant presents a special problem in that it is necessary to avoid both the rejection of the grafted tissue by the host and the damage of host tissue by the transplanted lymphocytes, a phenomenon called graft-versus-host disease. A living relative of the recipient is therefore usually the preferred donor, and by order of preference an identi-cal twin, an HLA-identical sibling (with six identical specificities for HLA-A, B, and DR), or an haplotype-identical relative (with three identical specificities for HLA-A, B, and DR) is selected. Mixed lymphocyte cultures can be also used to try to avoid the graft-versus-host reaction, which could emerge even in HLA-identical siblings due to incompatibilities in nontested minor antigenic systems. Cultures are set up by mixing the recipient’s lympho-cytes with lymphocytes from potential donors. A well-matched donor-recipient pair should react minimally to one another in these cultures.
In the case of liver transplantation, HLA matching is not important for graft accep-tance and survival. This unexpected finding may be due to the remarkable regenerative ca-pacity of the liver. HLA matching is also not generally performed in the case of heart, lung, and small bowel transplantation, because of the scarcity of available donor organs.
Related Topics