Chapter: Basic & Clinical Pharmacology : Sulfonamides,Trimethoprim,& Quinolones
Dna Gyrase Inhibitors : Fluoroquinolones
DNA GYRASE INHIBITORS
FLUOROQUINOLONES
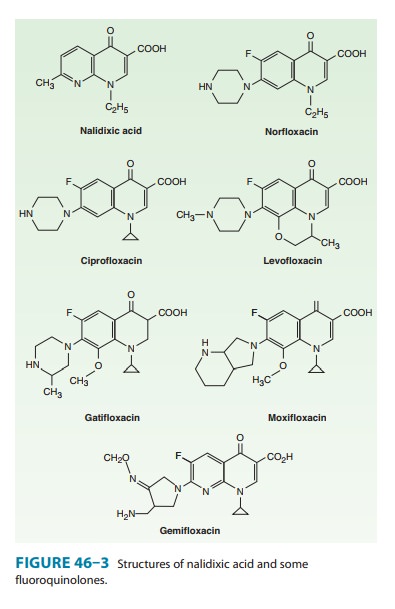
The important
quinolones are synthetic fluorinated analogs of nalidixic acid (Figure 46–3).
They are active against a variety of gram-positive and gram-negative bacteria.
Mechanism of Action
Quinolones
block bacterial DNA synthesis by inhibiting bacterial topoisomerase II (DNA gyrase)
and topoisomerase IV. Inhibition of DNA gyrase prevents the relaxation of
positively supercoiled DNA that is required for normal transcription and
replication. Inhibition of topoisomerase IV interferes with separation of
replicated chromo-somal DNA into the respective daughter cells during cell
division.
Antibacterial Activity
Earlier quinolones
such as nalidixic acid did not achieve systemic antibacterial levels and were
useful only in the treatment of lower urinary tract infections. Fluorinated
derivatives (ciprofloxacin, levofloxacin, and others; Figure 46–3 and Table
46–2) have greatly improved antibacterial activity compared with nalidixic acid
and achieve bactericidal levels in blood and tissues.
Fluoroquinolones were
originally developed because of their excellent activity against gram-negative
aerobic bacteria; they had limited activity against gram-positive organisms.
Several newer agents have improved activity against gram-positive cocci.
Thisrelative activity against gram-negative versus gram-positive species is
useful for classification of these agents. Norfloxacin is the least active of
the fluoroquinolones against both gram-negative and gram-positive organisms,
with minimum inhibitory concentrations (MICs) fourfold to eightfold higher than
those of ciprofloxacin. Ciprofloxacin, enoxacin, lomefloxacin, levofloxacin,
ofloxacin, and pefloxacin comprise a second group of similar agents possessing
excellent gram-negative activity and moderate to good activity against
gram-positive bacteria. MICs for gram-negative cocci and bacilli, including Enterobacter sp, P aeruginosa, Neisseria
menin-gitidis, Haemophilus sp,
and Campylobacter jejuni, are 1–2
mcg/mLand often less. Methicillin-susceptible strains of S aureus are gener-ally susceptible to these fluoroquinolones, but
methicillin-resistant strains of staphylococci are often resistant.
Streptococci and entero-cocci tend to be less susceptible than staphylococci,
and efficacy in infections caused by these organisms is limited. Ciprofloxacin
is the most active agent of this group against gram-negative organisms, P aeruginosa in particular.
Levofloxacin, theL-isomer of
ofloxacin,has superior activity against gram-positive organisms, including Streptococcus pneumoniae.
Gatifloxacin,
gemifloxacin, and moxifloxacin make up a third group of fluoroquinolones with
improved activity against gram-positive organisms, particularly S pneumoniae and some staphylo-cocci.
Gemifloxacin is active in vitro against ciprofloxacin-resistant strains of S pneumoniae, but in vivo efficacy is
unproven. Although MICs of these agents for staphylococci are lower than those
of ciprofloxacin (and the other compounds mentioned in the para-graph above),
it is not known whether the enhanced activity is sufficient to permit use of
these agents for treatment of infections caused by ciprofloxacin-resistant
strains. In general, none of these agents is as active as ciprofloxacin against
gram-negative organ-isms. Fluoroquinolones also are active against agents of
atypical pneumonia (eg, mycoplasmas and chlamydiae) and against intra-cellular
pathogens such as Legionella pneumophila
and some myco-bacteria, including Mycobacterium
tuberculosis and Mycobacteriumavium complex.
Moxifloxacin also has modest activity againstanaerobic bacteria. Because of
toxicity, gatifloxacin is no longer available in the United States.
Resistance
During fluoroquinolone therapy, resistant organisms emerge in about one of every 107–109 organisms, especially among staphylo-cocci, P aeruginosa, and Serratia marcescens. Resistance is due to one or more point mutations in the quinolone binding region of the target enzyme or to a change in the permeability of the organism. However, this does not account for the relative ease with which resistance develops in exquisitely susceptible bacteria. More recently two types of plasmid-mediated resistance have been described. The first type utilizes Qnr proteins, which protect DNA gyrase from the fluoroquinolones. The second is a variant of an aminoglycoside acetyltransferase capable of modifying ciprofloxacin. Both mecha-nisms confer low-level resistance that may facilitate the point muta-tions that confer high-level resistance. Resistance to one fluoroquinolone, particularly if it is of high level, generally confers cross-resistance to all other members of this class.
Pharmacokinetics
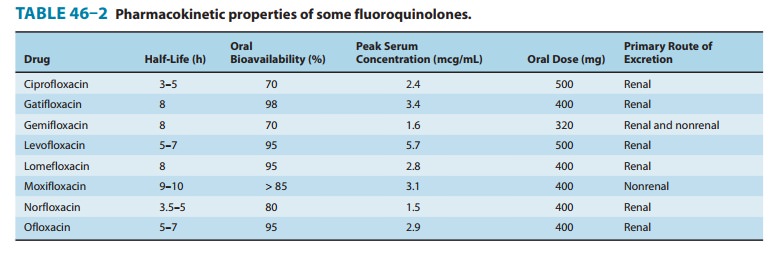
After oral
administration, the fluoroquinolones are well absorbed (bioavailability of
80–95%) and distributed widely in body fluids and tissues (Table 46–2). Serum
half-lives range from 3 to 10 hours. The relatively long half-lives of
levofloxacin, gemifloxacin, gati-floxacin, and moxifloxacin permit once-daily
dosing. Oral absorp-tion is impaired by divalent and trivalent cations,
including those in antacids. Therefore, oral fluoroquinolones should be taken 2
hours before or 4 hours after any products containing these cat-ions. Serum
concentrations of intravenously administered drug are similar to those of
orally administered drug. Most fluoroqui-nolones are eliminated by renal
mechanisms, either tubular secre-tion or glomerular filtration (Table 46–2).
Dosage adjustment is required for patients with creatinine clearances less than
50 mL/min, the exact adjustment depending on the degree of renal impair-ment and
the specific fluoroquinolone being used. Dosage adjust-ment for renal failure
is not necessary for moxifloxacin. Nonrenally cleared fluoroquinolones are
relatively contraindicated in patients with hepatic failure.
Clinical Uses
Fluoroquinolones
(other than moxifloxacin, which achieves rela-tively low urinary levels) are
effective in urinary tract infections caused by many organisms, including P aeruginosa. These agents are also
effective for bacterial diarrhea caused by Shigella,
Salmonella, toxigenic E coli, and Campylobacter. Fluoroquinolones (except norfloxacin, which does not
achieve adequate systemic concentra-tions) have been used in infections of soft
tissues, bones, and joints and in intra-abdominal and respiratory tract
infections, including those caused by multidrug-resistant organisms such as Pseudomonas and Enterobacter. Ciprofloxacin is a drug of choice for prophylaxis and
treatment of anthrax, although the newer fluoroquinolones are active in vitro
and very likely in vivo as well.
Ciprofloxacin and
levofloxacin are no longer recommended for the treatment of gonococcal
infection in the United States as resis-tance is now common. However, both
drugs are effective in treat-ing chlamydial urethritis or cervicitis.
Ciprofloxacin, levofloxacin, or moxifloxacin is occasionally used for treatment
of tuberculosisand atypical mycobacterial infections. These agents may be
suit-able for eradication of meningococci from carriers or for prophy-laxis of
infection in neutropenic cancer patients.With their enhanced gram-positive
activity and activity against atypical pneumonia agents (chlamydiae, Mycoplasma, and Legionella), levofloxacin, gatifloxacin, gemifloxacin, and
moxifloxacin— so-called respiratory fluoroquinolones—are effective and used
increasingly for treatment of upper and lower respiratory tract infections.
Adverse Effects
Fluoroquinolones are
generally well tolerated. The most common effects are nausea, vomiting, and
diarrhea. Occasionally, headache, dizziness, insomnia, skin rash, or abnormal
liver function tests develop. Photosensitivity has been reported with
lomefloxacin and pefloxacin. QTc prolongation may occur with gatifloxacin, levo-floxacin,
gemifloxacin, and moxifloxacin, which should be avoided or used with caution in
patients with known QTc interval prolon-gation or uncorrected hypokalemia; in those
receiving class IA (eg, quinidine or procainamide) or class III antiarrhythmic
agents (sotalol, ibutilide, amiodarone); and in patients receiving other agents
known to increase the QTc interval (eg, erythromycin, tricy-clic antidepressants).
Gatifloxacin has been associated with hyper-glycemia in diabetic patients and
with hypoglycemia in patients also receiving oral hypoglycemic agents. Because
of these serious effects (including some fatalities), gatifloxacin was
withdrawn from sales in the United States in 2006; it may be available
elsewhere.
Fluoroquinolones may
damage growing cartilage and cause an arthropathy. Thus, these drugs are not
routinely recommended for patients under 18 years of age. However, the
arthropathy is revers-ible, and there is a growing consensus that
fluoroquinolones may be used in children in some cases (eg, for treatment of
pseudomonal infections in patients with cystic fibrosis). Tendonitis, a rare
com-plication that has been reported in adults, is potentially more seri-ous
because of the risk of tendon rupture. Risk factors for tendonitis include
advanced age, renal insufficiency, and concur-rent steroid use.
Fluoroquinolones should be avoided during preg-nancy in the absence of specific
data documenting their safety.
Related Topics