Chapter: Nutrition and Diet Therapy: Diet During Childhood and Adolescence
Diet of Children Ages 1 to 12

CHILDREN AGES 1 TO 12
Eating habits develop
during childhood. Once developed, poor eating habits will be difficult to
change. They can exacerbate emotional and physical prob-lems such as
irritability, depression, anxiety, fatigue, and illness.
Because children learn
partly by imitation, learning good eating habits is easier if the parents have
good habits and are calm and relaxed about the child’s. Nutritious foods should
be available at snack time as well as at meal-time (Figure 13-1), and meals
should include a wide variety of foods to ensure good nutrient intake.
Parents should be
aware that it is not uncommon for children’s appetites to vary. The rate of
growth is not constant. As the child ages, the rate of growth actually slows.
The approximate weight gain of a child during the second year of life is only 5
pounds. In addition, children’s attention is increasingly focused on their
environment rather than their stomachs. Consequently, their appe-tites and
interest in food commonly decrease during the early years. Children between the
ages of 1 and 3 undergo vast changes. Their legs grow longer, they develop muscles,
they lose their baby shape, they begin to walk and talk, and they learn to feed
and generally assert themselves (Figure 13-2). A 2-year-old child’s statement
“No!” is his or her way of saying “Let me decide!”
As children continue
to grow and develop, they will increasingly and healthfully assert themselves.
They want and need to show their growing independence. Parents should respect
this need as much as possible. Children’s likes and dislikes may change. New
foods should be introduced gradually, in small amounts, and as attractively as
possible. Allowing the child to assist in purchasing and preparing a new food
is often a good way of arousing interest in the food and a desire to eat it.
Children
should be offered nutrient-dense foods because the amount eaten often will be
small. Fats should not be limited before the age of 2 years, but meals
Whole milk is recommended until the age
of 2, but low-fat or fat-free should be served from 2 on. The guideline for fat
intake is 30% to 35% of calories from fat for 2- to 3-year-olds and 25% to 35%
of calories from fat for 4- to 18-year-olds, with no more than 7% from
saturated fats. It is recommended that children not salt their food at the
table or have foods prepared with a lot of salt.
Young
children are especially sensitive to and reject hot (temperature) foods, but
they like crisp textures, mild flavors, and familiar foods. They are wary of
foods covered by sauce or gravy. Parents should set realistic goals and
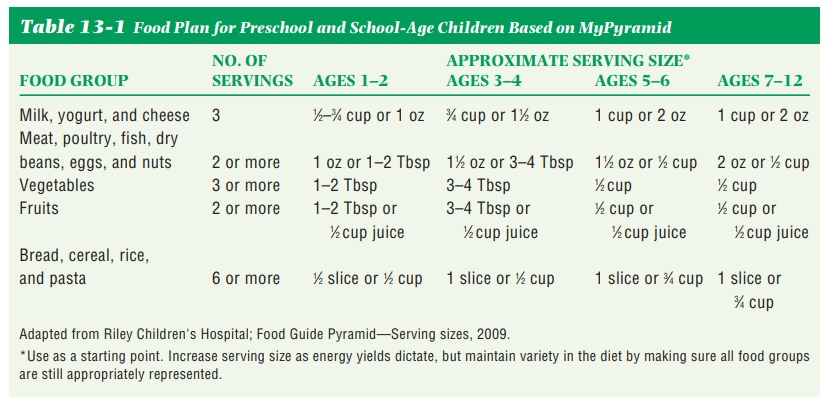
expectations about the amount of food a child needs. A good rule of thumb for
preschool children is 1 tablespoon for each year of age. Table 13-1 details
serving sizes according to age. Calorie needs will depend on rate of growth,
activity level, body size, metabolism, and health.
Children
can have food jags, such as eating only one or two foods, or rituals, such as
not letting foods touch on the plate or using a different spoon for each food
eaten. Choking is prevalent in young children. To prevent choking, do not give
children under 4 years of age peanuts, grapes, hotdogs, raw carrots, hard
candy, or thick peanut butter.
A
child needs a snack every 2 to 3 hours for continued energy. Children often
prefer finger foods for snacks. Snacks should be nutrient-dense and as
nutritious as food served at mealtime. Cheese, Cheerios, fruit, milk, and
unsweetened cereals make good snacks.
Mealtime
should be pleasant, and food should not be forced on the child. The parent’s
primary responsibility is to provide nutritious food in a pleasant setting, and
the child’s responsibility is to decide how much food to eat or whether to eat,
according to child expert Ellyn Satter (1995). When a child is hungry, he or
she will eat. Forcing a child to eat can cause disordered eating and,
ultimately, chronic overeating, anorexia nervosa, or bulimia.
Calorie and Nutrient Needs
The
rate of growth diminishes from the
age of 1 until about 10; thus, the caloric requirement per pound of body weight
also diminishes during this period. For example, at 6 months, a girl needs
about 54 calories per pound of body weight, but by the age of 10, she will
require only 35 calories per pound of body weight.
Nutrient
needs, however, do not diminish. From the age of 6 months to 10 years, nutrient
needs actually increase because of
the increase in body size. Therefore, it is especially important that young
children are given nutritious foods that
they will eat.
MyPyramid
(Figure 13-3) is a good foundation for developing meal plans that, with
adjustments, will suit all family members. A variety of foods should be
offered, and, when possible, the child should be offered some choices of foods.
Such a choice at the table helps the child’s psychosocial development.
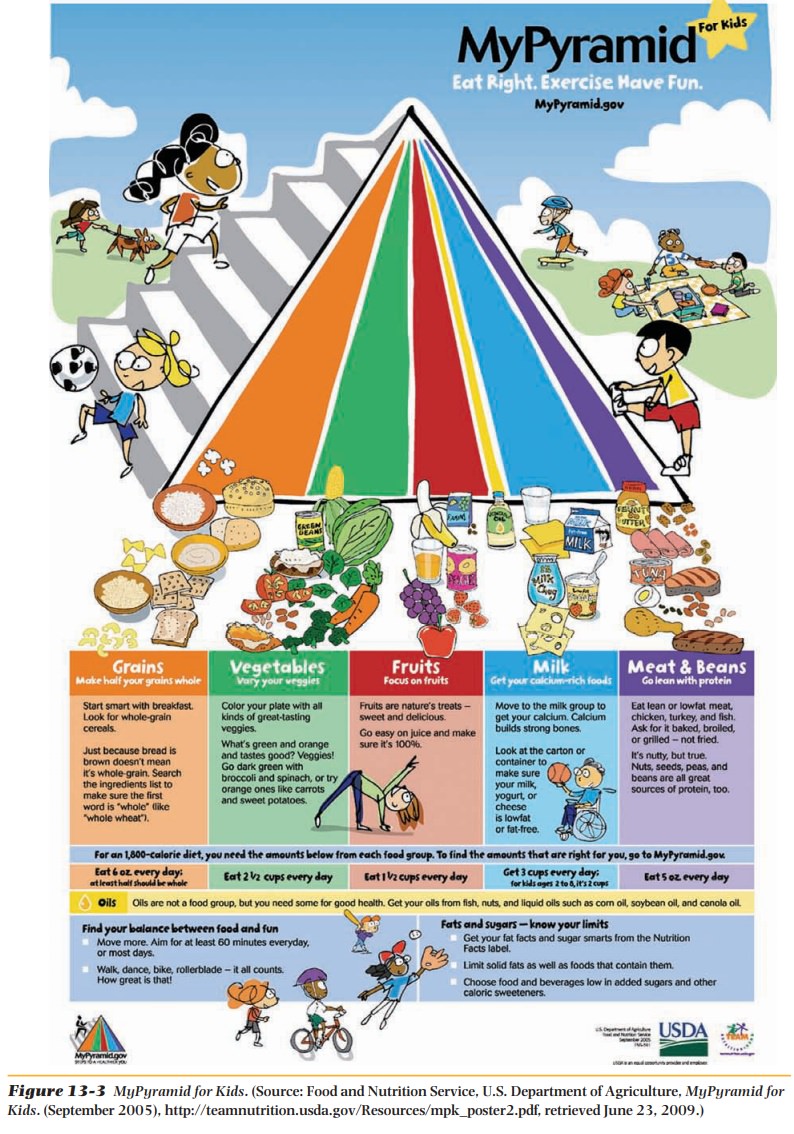
In general, the young child will need 2 to 3 cups of low-fat or fat-free milk each day, or the equivalent in terms of calcium. However, excessive use of milk should be avoided because it can crowd out other iron-rich foods and possibly cause iron deficiency. The selections of the other food groups are the same for adults, but the portions will be smaller. The use of sweets should be minimized because the child is apt to prefer them to nutrient rich foods. Sweet-ened fruit juices, especially, should be limited. Children also need water and fiber in their diets. They need to drink 1 ml of water for each calorie. If food valued at 1,200 calories is eaten, then five 8-ounce glasses of water are needed. Fiber needs are calculated according to age. After age 3, a child’s fiber needs are “age + 5 grams” and no more than “age + 10 grams.” A child who eats more fiber than that might be too full to eat enough other foods to provide all the calories needed for growth and development. Fiber should be added slowly, if not already in the diet, and fluids must also be increased. Childhood is a good time to develop the lifelong good habit of getting enough dietary fiber to prevent constipation and diseases such as colon cancer and diverticulitis.
Childhood Obesity
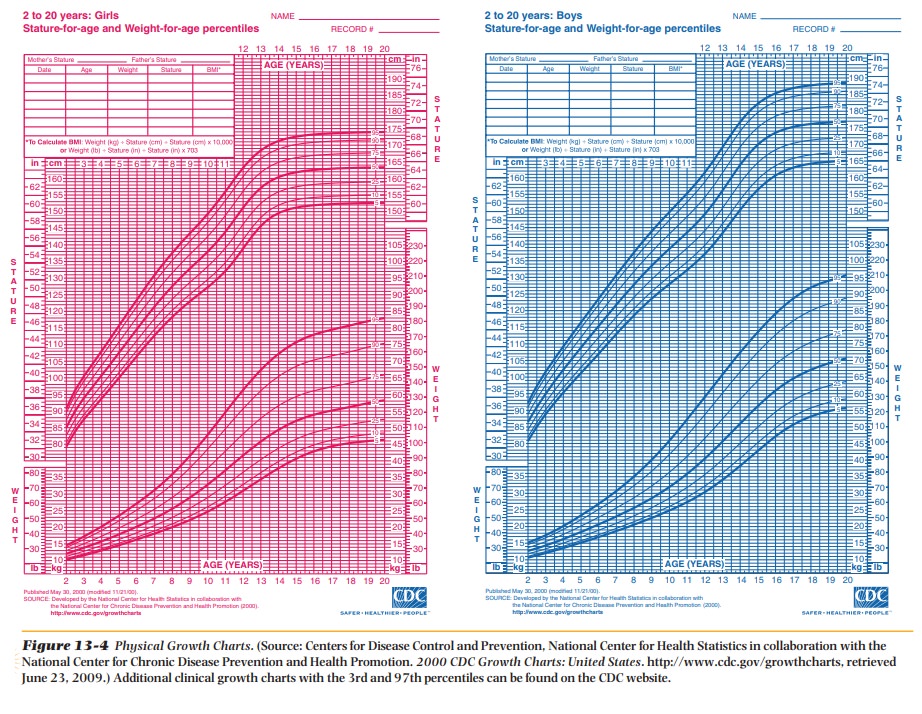
Normal stature and
weight for children can be determined using standardized growth charts (Figure
13-4). Expected growth patterns will fall between the 5th and 95th percentile;
children whose weight falls outside those parameters need special evaluation
and attention. Childhood obesity has become an epidemic. Overweight has doubled
in the last 20 to 30 years, and one in five children is now overweight. The
definition of overweight is a child at or above the 95th percentile of body
mass index (BMI) by sex and age. Children are considered obese when their body
fat exceeds lean muscle mass. Type 2 diabetes mellitus, rarely seen before in
children, is now being diagnosed in children as young as 10; it is related to diet
and weight.

Childhood obesity is
the result of an imbalance between the calories a child consumes as food and
beverages and the calories a child expends for normal growth and development,
metabolism, and physical activity. The bottom line is that calories eaten and
calories expended must be balanced. There is no single factor that causes
childhood obesity. An imbalance can result from the influences and interactions
of a number of factors, including genetic, behavioral, and environmental.
Genetics cannot be
solely to blame for childhood obesity. The genetic factors of the population
have not changed in the past 30 years, but the prevalence of overweight and
obese children has tripled during this time. If one parent is obese, there is a
50% chance that their children will be obese. If both parents are obese, the
risk increases to 80%.
Certain behavioral
factors can contribute to an energy imbalance and therefore obesity. Energy
intake of large portions of food and beverages, eating meals away from home,
frequent snacking on energy-dense foods, and consuming beverages with sugar are
all contributing factors for obesity. Chil-dren drinking sugared beverages may
not compensate for these additional calories at mealtime.
Physical activity is
important for children to help burn excess calories eaten. Obese children and
adults have similar health problems. Physical activity will help increase bone
strength and decrease blood pressure and prevent type 2 diabetes, sleep apnea,
and hyperlipidemia. Many schools have discontinued physical education,
especially for adolescents, but recess still continues for younger children. GET MOVING! Obese children have an 85%
chance of being obese adults if they are obese after the age of 10. Physical
activity can be as easy as walking for 60 minutes per day.
Many children with
working parents are not allowed to leave the house after returning from school.
Sedentary activities, such as watching TV and DVDs, playing computer games and
handheld electronic games, and eating, become the norm. There is a high
correlation between watching TV and obesity. TV can contribute to poor food
choices, excess snacking, and low metabolism.
Environmental factors, including the home, child care, school, and community, can influence a child’s behavior related to food and physical activity. In the home, children will imitate their parents in many ways, including eating habits and physical activity.
Child
care is an important place where healthy eating and physical activity habits
can be developed. Approximately 80% of children with working mothers spend 15
to 40 hours per week at day care. Parents need to check the menu and activity
schedule on a weekly basis.
Children
ages 5 to 17 are enrolled in school, which is a positive envi-ronment in which
to teach healthy eating and the importance of physical activity. Unfortunately,
the government is not helping, and many of the foods served in school
cafeterias are government subsidies. They are generally high-calorie, high-fat
foods that must be deep fried before serving. Butter and cheese sometimes are
included in these subsides. Vending machines are in many schools and, if not
stocked with healthy foods, can contribute to obesity.
Leaders in the
community must create an infrastructure conducive to physical activity like
sidewalks, safe bike and walking trails, parks in neighbor-hoods, and a safe
environment in which to participate.
Snacking and portion
control seem to be big issues with obese children. All foods can be fattening
if eaten beyond needs. Children should not be put on a “diet.” Children
continue to grow, so if weight can be maintained by exercise and portion
control until growth catches up, the problem of obesity will no longer exist.
An obese child, like a
child of normal weight, may need a snack after school. Make that snack a
healthy choice, such as a medium-sized piece of fruit, vegetables (using salsa
or fat-free ranch dressing as a dip), a 100-calorie bag of microwave popcorn,
or a single serving of cereal. Single-serving-size bags or premeasured portion
controlled snacks are ideal because an obese child will be likely to overeat
when eating from a large bag. Help children avoid drinking their daily caloric
needs with pop (soda) or other sweetened drinks. If junk food and sweetened
drinks are not purchased, they cannot be consumed.
What can parents do to
help their children? Talk to a dietitian or a nurse for some ideas like the
following:
• Understand that this is a family problem and that the entire
family will be involved in the solution.
• Help your family balance their calories. One part of balancing
is tosupply adequate nutrition and help everyone develop healthy eating habits.
• Develop healthy eating habits by doing the following:
o Provide plenty of
vegetables, fruits, and whole-grain products.
o Include low-fat or
nonfat dairy products.
o Choose lean meats,
poultry, fish, lentils, and dried beans for protein.
o Serve correct portions
(see Figure 17-3).
o Encourage everyone to
drink lots of water.
o Limit sugar-sweetened
beverages.
o Limit consumption of
sugar and saturated fat.
o Learn to make favorite
dishes healthier. For new ideas about adding fruits and vegetables to your
family’s diet check out the recipe database from http: // www.
FruitsandVeggiesMatter .gov.
o Remove calorie-rich
temptations. Allow your children to eat them “sometimes” so that they will be
truly a treat.
Remember that small changes every day can lead to success.
To continue the
progress made with healthy eating, everyone must participate in one or more
forms of physical activity each day for 60 minutes, such as the following:
• Brisk walking
• Playing tag
• Jumping rope
• Playing soccer
• Basketball
• Swimming
• Riding bicycles
• Dancing
In addition to
encouraging physical activity, help children avoid too much sedentary time.
Quiet time for homework and reading is fine.
Obese children and
adolescents are targets of social discrimination. This begins early in a
child’s school career, and the psychological effect can be devastating, causing
low self-esteem, which in turn may hinder academic and social functioning.
This may seem like a
monumental task for parents, but it is well worth it. Not only will their
children change their eating habits and start a lifelong exercise program, but
so will they.
What Can Parents Do to Help?
• Provide only healthy, nourishing food for meals and snacks. If
it is not available a child cannot eat it.
• Limit TV and computer time. Remove TV sets from your child’s
bedroom.
• Get moving yourself. Exercise benefits everyone.
• Never tell a child he cannot have a food because “he is too
fat.”
• Learn correct portions, even if this means weighing and
measuring (see Table 13-1).
• Remember, there is nothing a child cannot eat; it is just how
oftenand how much will be consumed of a particular food. There are no good or
bad foods.
• Never provide food for comfort or as a reward.
• Eat only at the table and at designated times.
• Give water to drink rather than calorie-laden fruit juice. If a
childwon’t drink water, then a small amount of juice can be mixed with water to
give flavor. Use 1⁄ cup juice to 8–12 ounces of water. This 4 glass of
water-juice will contain about 30 calories versus 120–180 for 100% juice.
• Eat slowly—it takes 20 minutes for the brain to get the message
that the stomach is full. Make it a game—set a timer and see who can make the
meal last for 20 minutes.
• Use the 20-minutes technique if your child wants a
calorie-densesnack such as cookies, chocolate, candy bars, or other
calorie-dense foods. The child must set the timer, sit at the table with a
portion-controlled serving, pay attention to the treat, and make it last for 20
minutes. Holding it in the mouth and rolling it around on the tongue will
satisfy taste buds quicker than swallowing immediately and may contribute to
satiety sooner.
• Learn to determine whether your child is really hungry or
justbored, tired, or lonely. It takes 3 to 4 hours for a stomach to completely
empty after a significant meal, so if that amount of time has elapsed, then
your child is truly hungry.
• Make sure your child gets enough sleep (8–10 hours per night),
as sleep deprivation has been linked to obesity.
• Change any unhealthy habits you may possess. You are your
child’steacher.
Preventing and
reversing childhood obesity will also decrease the incidence of obesity-linked
type 2 diabetes.
Childhood Type 2 Diabetes
As a result of the
increase of childhood obesity, there is a parallel increase in diabetes,
particularly type 2. Type 2 diabetes is normally found only in adults, usually
after the age of 40, and is associated with weight. Most obese children will
develop type 2 diabetes between the ages of 10 and 14.
Children with type 2
diabetes should see a certified diabetes educator to learn what to eat to
control their diabetes. The diabetes educator will also prescribe daily exercise
and attention to fiber intake, both of which help control blood glucose.
Increasing nutrition
and exercise knowledge of parents and children appears to be the only way to
prevent obesity and childhood type 2 diabetes.
Osteoporosis and Cardiovascular Disease
Children and
adolescents live in the moment. This creates problems associated with
osteoporosis and cardiovascular diseases. Adherence to sound nutrition
principles during childhood and adolescence are needed to protect the heart and
bones.
Calcium must be
consumed at the DRI level until the age of 30. Fat intake should follow the
American Heart Association recommendations of 7% saturated fat, 8%
polyunsaturated fat, and 15% monounsaturated fat while keeping total fat to 35%
of daily calories.The typical diet of a teenager contains too much saturated
fat and soda and not enough milk. These habits lead to adult health problems.
Motivating children and teens to change their habits will be a challenge but
needs to be done.
Related Topics