Chapter: Nutrition and Diet Therapy: Diet and Clients With Special Needs
Diet and Client Receiving Enteral Nutrition
THE CLIENT RECEIVING
ENTERAL NUTRITION
The term enteral nutrition means the forms of
feeding that bring nutrients directly into the digestive tract (Figure 22-1).
Oral feeding is the usual method and should be used whenever possible. When
clients cannot or will not take food by mouth but their gastrointestinal tract
is working, they will be given a tube feeding (TF). Sometimes this may be
necessary because of uncon-sciousness, surgery, stroke, severe malnutrition, or
extensive burns.
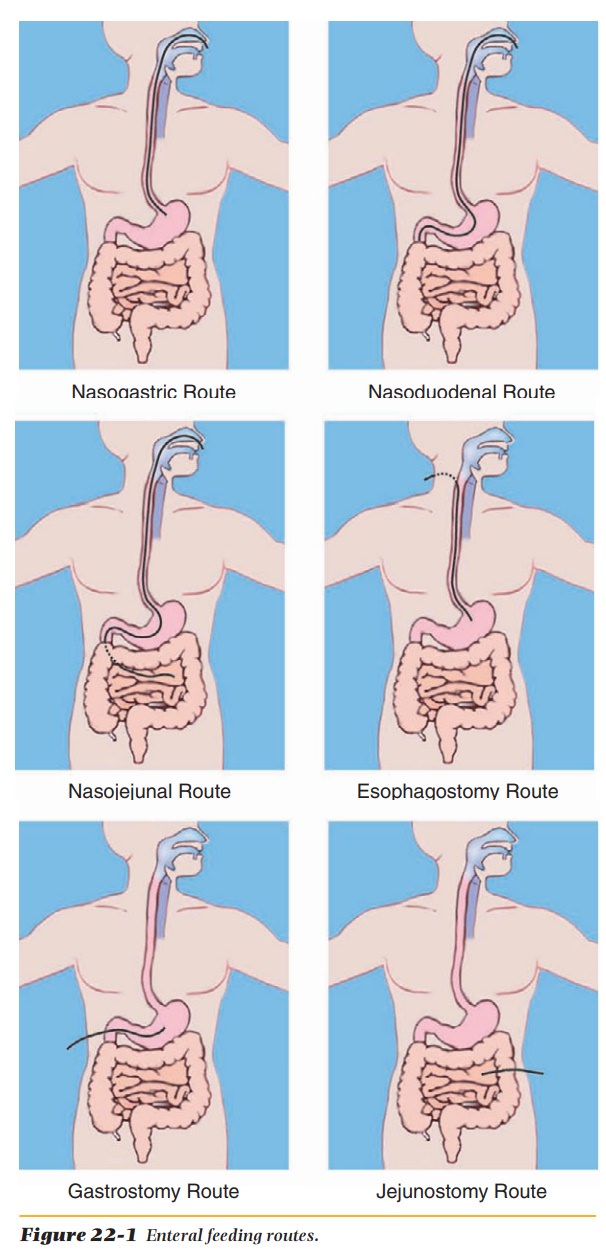
Usually, for periods that do not exceed 6 weeks, tube feeding is adminis-tered through a nasogastric (NG) tube inserted through the nose and into the stomach or small intestine. When the percutaneous endoscopic gastrostomy (PEG) tube cannot be placed in the nose or when tube feedings will be required for more than 6 weeks, an opening called an ostomy is surgically created into the esophagus (an esophagostomy), the stomach (gastrostomy), or the intes-tine (jejunostomy).
The tubes used for
these feedings are soft, flexible, and as small as they can be and still allow
the feeding to pass through. Although some tubes are weighted to keep them in
place in the stomach or intestine, the use of weighted tubes has not been
proved to be better than unweighted.
Numerous commercial
formulas are available, with varying types and amounts of nutrients. Clients
who are able to digest and absorb nutrients can be given polymeric formulas (1–2 calories/ml)
containing intact proteins, carbohydrates, and fats that require digestion.
Clients who have limited ability to digest or absorb nutrients may be given elemental or hydrolyzed formulas (1.0 calories/ml)
that contain the products of digestion of proteins, carbohy-drates, and fats,
and are lactose-free. Modular formulas (3.8–4.0 calories/ml)
can be used as supplements to other formulas or for developing customized
formulas for certain clients (such as those with extensive wound-healing
needs). The use of modular formulas has been decreasing due to the development
of high-protein formulas. Disease-specific formulas have been developed to be
used in the acute setting and for a short period of time. Clients admitted to
the hospital with renal failure, respiratory failure, or liver failure have
been shown to benefit from these specialized formulas.
There are three
methods for administering tube feedings: continuous, intermittent, and bolus.
Intermittent can mean to only administer tube feeding at night, with solid
foods eaten during the day. If there is a food-drug interac-tion, such as with
phenytoin (Dilantin), the TF should be stopped 1 hour before and be restarted 1
hour after administration of the medication via tube.
Daily calorie needs of
the client are usually divided into six servings per day (not to exceed 400 cc
at a time). These feedings are given over a 15-minute time span and followed by
25 to 60 ml of water, hence the term bolus.
This method is usually done when a client has a PEG tube, but it could also be
done with an NG tube.
Usually the feedings
are administered by a pump. This means the feeding is continuous during a 16-
to 24-hour period. Sometimes the formula is given at half strength at a rate of
from 30 to 50 ml per hour. This rate may be increased by about 25 ml every 4
hours until tolerance has been established. Once the client tolerates the
half-strength formula, a full-strength formula is initiated at the appropriate
rate. When clients are ready to return to oral feed-ings, the transfer must be
done gradually.
Possible Complications with Enteral Nutrition
The osmolality of a
liquid substance means the number of particles per kilogram of solution.
Solutions with more particles (high osmolality) exert more pressure than
solutions with fewer particles. Solutions with high osmolality attract water
from nearby fluids that contain lower osmolality. When a formula with high
osmolality reaches the intestine, the body may draw fluid from the blood to
dilute the formula. This process can cause weakness and diarrhea in the client.
However, diarrhea should be attributed to the tube feeding only when all other
causes have been ruled out. Liquid medications containing sorbitol or Clostridium difficile (C-dif) (the
bacterium that causes dysentery) are two possible causes of diarrhea.
Aspiration can occur
(some of the formula enters the lung), causing the client to develop pneumonia.
The tube may become clogged, or the client may pull the tube out. The placement
of the feeding tube should be checked with an X-ray to decrease the possibility
of aspiration. Before beginning the tube feeding, the health care provider must
administer the flush solution according to the physician’s order and raise the
head of the bed. If the feeding is contin-uous, then the head of the bed needs
to remain elevated. Some facilities, to verify correct placement of the NG tube
in the stomach, will check the gastric pH before each use.
Obviously, clients
requiring tube feeding need a great deal of patience and understanding. They
have been deprived of a basic pleasure of life—eating. They may also be
uncomfortable and apprehensive.
Related Topics