Chapter: Clinical Cases in Anesthesia : The Difficult Airway
Describe the management options for a patient who, after induction of anesthesia
Describe the management options for a patient who, after induction
of anesthesia, unexpectedly cannot be intubated with a Macintosh blade. This
patient has a good mask airway.
Having induced general anesthesia in a patient
and then discovered a difficult intubation, it is imperative to maintain
oxygenation and ventilation. This is generally accom-plished with a facemask
and 100% oxygen. Successful oxygenation during controlled ventilation and
desaturation during intubation attempts are monitored with pulse oximetry.
During traditional laryngoscopy, external posterior and/or lateral displacement
of the larynx may bring it into view. Improved sniffing position may be
helpful.
A multitude of retraction blades exist and vary
in length and shape. They are used to displace the base of the tongue and
epiglottis anterior to the line of vision. The most familiar types are the
Macintosh and Miller blades. Difficulty with the Macintosh blade often arises
when its tip fails to elevate the hyoid bone, which indirectly raises the
epiglottis. Often, a straight blade elevates a floppy epiglottis when curved
blades fail to do so. Difficulty with the straight blade frequently comes from
impacting on teeth. The Siker blade was developed to view the “anterior larynx”
but is extremely difficult to use because the laryngo-scopist must learn to
work with a mirror image. The Bellscope, a bent straight blade, offers the
advantages of the Macintosh and Miller blades, as well as improved anterior
vision by employing angulation and a prism, rather than a mirror. The Bullard
and Wu laryngoscopes incorporate a fiberoptic viewing system and a broad
retraction blade. Consequently, sniffing position is not as important when
using these laryngoscopes. They may be of greatest potential benefit for those
whose head must remain flat on the bed, such as the patient with cervical spine
fractures. A working channel is provided for suctioning, administra-tion of
local anesthetics, or insufflation of oxygen. Both the Bullard and Wu
laryngoscopes require a mouth opening sufficiently wide to accommodate the
broad retraction blade and endotracheal tube. Blood and secretions in the
airway tend to impair the view through fiberoptic systems. Upper airway edema
or adipose tissue may sometimes encroach on the view of traditional retraction
laryngoscopes, which are open on the right side. A two-piece tubular
laryn-goscope such as the Wu scope can overcome this problem.
Various stylets may be used. The hollow stylet,
gummed elastic bougie, or similar devices should be available in all
anesthetizing locations. High-technology variations, such as illuminating
stylets, work well in the average adult but are associated with false-positives
and false-negatives in the very thin and obese. Illuminating stylets function
on the principle of transillumination. As the light bulb enters the trachea,
transilluminated light remains bright and circumscribed. If the stylet enters
the esophagus, the light becomes more diffuse. Factors impairing its usefulness
include anterior cervical scars, obesity, neck tumors, blood, or secretions.
Macintosh first described this technique in 1957. Over the ensuing five
decades, it has not gained popularity.
If a flexible fiberoptic laryngoscopy is not
planned, then blind spontaneously breathing nasal tracheal intubation is an
alternative offering a good chance of success. Vasoconstriction of the nasal
mucosa, selection of a small nasal tracheal tube (6 mm), and generous
lubrication of the tube’s distal portion are highly recommended. If flexi-ble
fiberoptic intubation is planned, then the risk of epi-staxis may dissuade one
from the nasal approach. Epistaxis might seriously impair mask ventilation and
visualization by all means of laryngoscopy.
Retrograde guided techniques are highly
successful but have not gained popularity. The cricothyroid membrane is pierced
by a 16-gauge needle at a 30° angle pointing cepha-lad. Confirmation of proper
placement is achieved by aspi-rating air into a syringe. The needle remains in
situ, and a thin wire is passed through the needle until it exits the mouth or
nose. The wire is clamped outside the neck to anchor its distal end. The
endotracheal tube is advanced over the guidewire and into the trachea. Several
predictable problems occur with this technique. After the wire is threaded
retrograde through the airway, it may not exit the mouth or nose. Laryngoscopy
and retrieval with a clamp may be necessary. Advancement of the endotracheal
tube along the wire may be blocked by the arytenoids. To over-come this
problem, the endotracheal tube is retracted 1–2 cm and rotated 90°
counterclockwise. Progression beyond the vocal cords and into the trachea may
be prevented by the guidewire as it exits the neck and tethers the endotracheal
tube at a distance of 1–2 cm into the trachea.
Alternatively, the portion of the guidewire
that exits the mouth or nose can be threaded through the working channel of a
flexible fiberoptic laryngoscope. The scope is then advanced over the wire,
under direct vision, through the vocal cords. In this way passage through the
vocal cords and into the trachea is confirmed visually. Once positioned
properly in the trachea, the endotracheal tube can be advanced over the
fiberscope, and its proper location above the carina confirmed.
Compared with various retraction blades and
stylets, flexible fiberoptic laryngoscopy has established a long and impressive
success record with difficult intubations. Flexible fiberoptic laryngoscopy is
applicable to the anes-thetized and awake patient. In the anesthetized patient,
it can be performed with interrupted controlled ventilation by facemask, such
as with traditional rigid laryngoscopy. Alternatively, it can be accomplished
using simultaneous controlled ventilation via anesthesia facemasks equipped
with a self-sealing diaphragm.
Flexible fiberoptic intubation in the paralyzed
patient is generally more difficult than in the spontaneously breathing patient
because the anterior pharyngeal wall tends to collapse onto the posterior
pharyngeal wall, thereby obstructing the view. Also, the larynx assumes a more
anterior position, hindering its identification. Copious blood and/or
secretions seriously impair vision through a flexible fiberoptic laryngo-scope
(FFL). FFLs contain suction channels, but unlike suction channels in the pulmonologist’s
bronchoscope, the FFL’s channel is an inefficient one. Consequently, blood and
secretions are aspirated better with a standard large-bore suc-tion device,
such as the one normally used for traditional rigid laryngoscopy. Passing
oxygen through the FFL’s work-ing channel tends to push blood and secretions
out of the way, prevents fogging, and enhances the patient’s effective FIO2.
The sniffing position allows for further posterior dis-placement of the
epiglottis, which could also obstruct the view. Consequently, cervical
extension with the head flat on the bed is preferable for flexible fiberoptic
laryngoscopy.
Various aids to FFL insertion exist. Care must
be taken to seat oral airways exactly in the midline to prevent lateral
displacement of the fiberscope, which adds to the difficulty of intubation. In
cases for which it is especially important to do so, none of the presently
available oral intubation air-ways adequately elevate the base of the tongue.
Insertion of the nasal tracheal tube before the fiberoptic scope risks
epistaxis before passage of the insertion tube. Furthermore, placing nasal
tracheal tubes too far eliminates adequate space for manipulating the scope
between the nasal tracheal tube and larynx. Difficulty threading endotracheal
tubes into the larynx may arise if the endotracheal tube’s tip abuts the right
arytenoid. To overcome this obstacle, the endotracheal tube should be retracted
1–2 cm and rotated 90° counterclockwise. This maneuver brings the tip
ante-riorly, away from the right arytenoid.
After exhausting one’s personal repertoire of
techniques, simply repeating methods that have already failed seems to have
little chance of success. Additional instrumentation will lead to laryngeal and
pharyngeal edema predisposing the patient to airway obstruction. The remaining
options include continuing anesthesia by facemask; performing regional
anesthesia; for urgent cases, awakening the patient and intubating with
spontaneous breathing that day; awak-ening the patient and intubating with
spontaneous respira-tions several days later to allow for resorption of airway
edema; performing tracheostomy; and performing cricothy-roidotomy. Initial
tracheostomy is indicated for laryngeal fractures and for abscesses impinging
on the airway.
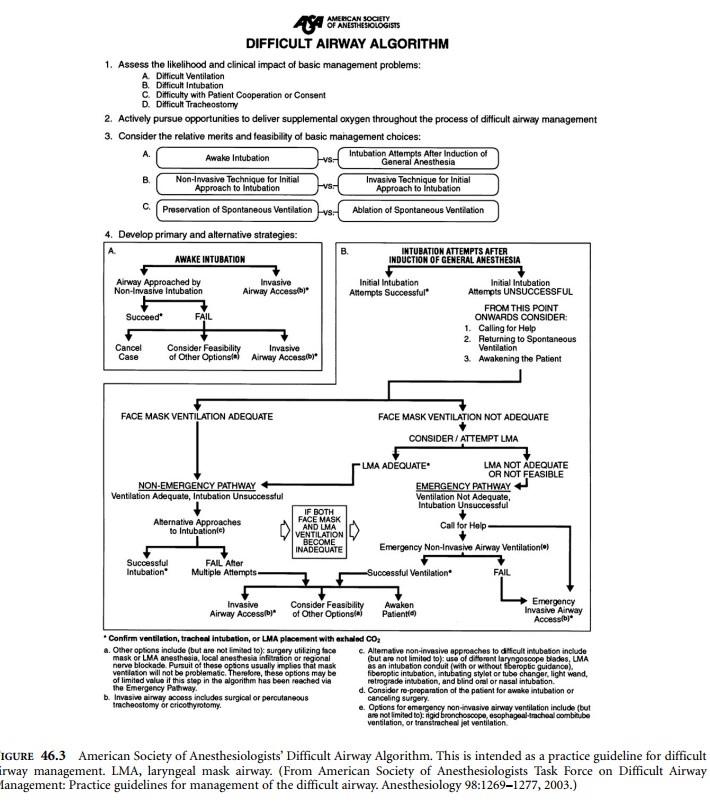
The ASA’s Difficult Airway Algorithm serves as
a useful guideline (Figure 46.3).
Related Topics