Chapter: Clinical Cases in Anesthesia : Gastroschisis and Omphalocele
Describe the fluid and blood product management for this neonate intraoperatively
Describe
the fluid and blood product management for this neonate intraoperatively.
Intraoperative fluid requirements can be
divided into three basic areas: maintenance fluid, preoperative fluid deficit
replacement, and replacement of third-space and blood losses.
Maintenance Fluid
Maintenance fluid volume is determined based on
weight as shown in Table 65.2.
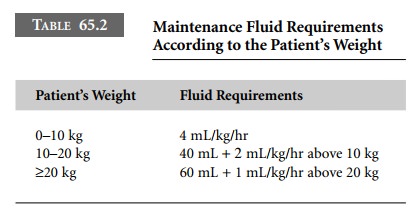
Maintenance requirements for water,
electrolytes, and glucose have been standardized using metabolic rates. This
has led to D5 0.2% NS being used as standard maintenance fluid.
Several factors including increased temperature and increased metabolic rate
can increase maintenance fluid requirements. Balanced salt solutions are
standard replace-ment fluids used in the operating room and in the older infant
are used for maintenance also. Glucose-free fluids are generally used in the
operating room for several reasons. Most notably, intraoperative hypoglycemia
is very rare in older infants and children. Hyperglycemia, on the other hand,
is associated with adverse outcomes related to the brain, heart, and intestines
during ischemic events. However, neonates and specifically preterm infants are
at risk for hypoglycemia and may require glucose infusions during the
intraoperative period. In these situations, only
the maintenance fluids should contain glucose.
Fluid Deficit Replacement
This patient presenting to the operating room
would not have a fluid deficit, as it would have already been cor-rected during
the preoperative preparation. Typically, the fluid deficit results from
prolonged fasting times. This deficit is determined by multiplying the hourly
maintenance fluid requirement by the number of hours that the patient has been
fasting. The deficit is replaced with a balanced salt solution over a 3-hour
period: 50% infused in the first hour and 25% infused the second and third
hours.
Third-Space Losses
The magnitude of third-space losses depends on
the site and extent of surgical manipulation. The guidelines for third-space
loss replacement recommend 8–15 mL/kg/hr during extensive intra-abdominal
surgery. A neonate with gastroschisis could potentially require 5–10 times this
amount for third-space replacement. Third-space loss should be replaced with a
balanced salt solution without glucose. The state of hydration needs to be continually
assessed.
Blood Losses
Prior to any procedure where blood loss is
expected, the anesthesiologist should determine the approximate blood volume
and estimate the allowable blood loss (ABL). It is important to remember that
the ABL is an estimate, as many variables are considered when determining the
level of anemia that each patient will tolerate. ABL is calculated as follows:
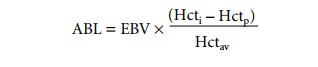
where
EBV = estimated blood volume (see Table 65.3)
Hcti = initial hematocrit
Hctp = allowable perioperative
hematocrit
Hctav = average of Hcti
and Hctp (Hcti + Hctp/2).
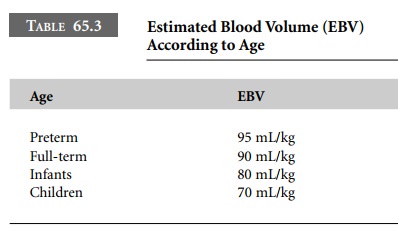
When determining the estimated allowable
periopera-tive hematocrit, the affinity for oxygen of hemoglobin F must be
considered. In the neonate with high levels of hemoglobin F, oxygen delivery at
the tissue level is low despite potentially high hemoglobin levels (P50
approxi-mately 19 mmHg.)
Replacement of blood and fluid is critical in
small neonates since their total blood volume is so small. Blood loss needs to
be replaced as it occurs to maintain normovolemia. It can be replaced with
crystalloid (3 times the amount of blood loss) or with colloid or blood in
equal volumes.
Once a decision is made to transfuse, every
effort should be made to limit exposures to multiple donors. In pediatric
patients, this means dividing a single donor unit into a “pedi pack” (1 unit
divided into multiple 50–100 mL parts) so that the same donor unit can be
administered at differ-ent times. A general rule is that the increase in hematocrit
with red blood cell administration will be approximately the same as the
milliliters per kilogram infused.
Related Topics