Chapter: Clinical Cases in Anesthesia : Depolarizing Neuromuscular Blockade
Describe other recognized side-effects of succinyl-choline
Describe
other recognized side-effects of succinyl-choline.
Succinylcholine administration is associated
with a number of complications, ranging from benign to lethal. They include
prolonged blockade (discussed above), myal-gias, increased intraocular,
intragastric, and intracranial pressures, dysrhythmias, masseter muscle spasm,
anaphy-lactic and anaphylactoid reactions, and hyperkalemia.
Myalgias have been reported postoperatively in
5–83% of patients receiving succinylcholine. This complication is more common
in ambulatory patients. It can be attenuated by pretreatment with a small dose
of a nondepolarizing muscle relaxant or lidocaine. The mechanism of
succinyl-choline-induced myalgias is thought to be a result of a shift of
calcium intracellularly, leading to damage of cellular structures via
activation of phospholipase A2. Patients who develop myalgias are
reported to have a fall in serum calcium after succinylcholine. Alternatively,
muscle spindle damage from asynchronous muscle contractions that is due to high
intracellular calcium concentration has been proposed as a mechanism of
myalgias following succinyl-choline.
Succinylcholine causes a sustained increase in
intraocu-lar pressure of 5–15 mmHg for 10 minutes. This was attrib-uted to
extraocular muscle fasciculations. However, Kelly et al. (1993) demonstrated a
rise in intraocular pressure after removal of extraocular muscles. Although it
has been sug-gested that succinylcholine may aggravate open eye injuries, a
1985 report did not show worsening of eye injuries following succinylcholine
administration. The use of suc-cinylcholine in open eye injuries remains
controversial.
Intragastric pressure is also reported to
increase follow-ing succinylcholine. The increase is related to visible
fasci-culations and may be attenuated by a small dose of a nondepolarizing
muscle relaxant before succinylcholine.
Intracranial pressure increases after
succinylcholine administration to laboratory animals. The issue is more
complicated in humans because it is difficult to separate succinylcholine’s
effect from those of other actions per-formed at the same period of time.
Different views are expressed by different experts regarding the safety of
succinylcholine in patients with raised intracranial pres-sure. Potential risks
of brain stem herniation must be weighed against those of airway compromise
from pro-longed onset of profound muscle relaxation achieved in other ways.
Dysrhythmias are associated with
succinylcholine administration. Tachydysrhythmias may occur but are less
problematic than bradycardias. Bradycardia is more com-mon in children but may
occur in adults particularly after a second dose of succinylcholine. This problem
can be attenuated by pretreatment with a vagolytic agent. Metabolic breakdown
products of succinylcholine do not seem to play a part in causing dysrhythmias,
because infu-sions of succinylcholine do not cause this problem.
Masseter muscle spasm (MMS) following
succinyl-choline presents a complicated problem. It has been sug-gested that
MMS following succinylcholine is a harbinger of malignant hyperthermia (MH).
Many of the patients who have demonstrated MMS have had positive muscle
biopsies for MH susceptibility. Because succinylcholine is a triggering agent
for MH, some authors have recommended aborting surgery and monitoring for MH.
In a large retro-spective series published by Littleford et al. (1991),
patients who had MMS were allowed to continue with their anes-thetic (often
including inhaled agents) and surgery. None of their patients developed MH;
however, some showed biochemical abnormalities associated with MH. VanDerSpeck
et al. (1988) demonstrated in children that masseter muscle tone increases following
succinylcholine while limb muscles are relaxed. This may represent a variant of
the normal relaxant response to succinylcholine. However, it does not preclude
the development of MH. Clinical management following succinylcholine-induced
MMS is controversial.
Sustained generalized muscle contracture is
associated with MH and must be considered in a different light from isolated
MMS. Sustained muscle contracture may also occur in patients with myotonia and
dermatomyositis. In these latter circumstances, laryngoscopy may prove
diffi-cult, but metabolic disturbances are unlikely.
Anaphylactic and anaphylactoid reactions may
occur to many drugs used in anesthesia. Muscle relaxants are most often
implicated (80% of cases), and succinylcholine is the most frequent relaxant
responsible (54%).
Hyperkalemia is a serious complication of
succinyl-choline. Under certain conditions, upregulation (prolifera-tion) of
nicotinic receptors occurs. This increase in receptors is associated with the
appearance of extrajunctional recep-tors. When exposed to succinylcholine,
these receptors allow a massive egress of intracellular K+, leading
to hyper-kalemia. Normal increases in serum K+ following
succinyl-choline are 0.5–1.0 mEq/L. This rise usually lasts 10–15 minutes. The
pathologic response may be far greater.
Increases of 7.0 mEq/L have been measured.
Acute hyper-kalemia may cause peaked T-waves, cardiac conduction block,
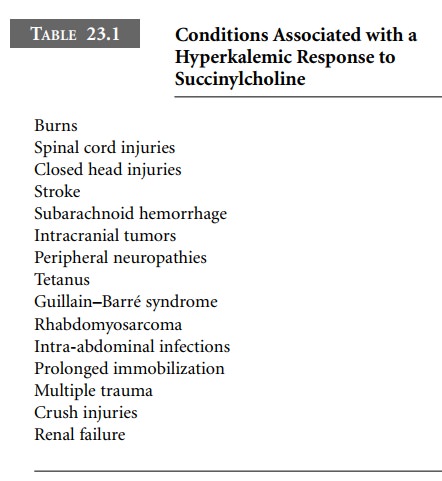
ventricular dysrhythmias, or sine-wave cardiac arrest. Conditions associated
with a hyperkalemic response to succinylcholine are listed in Table 23.1.
Many authors suggest that a safe period exists
several months after injury. This is not well documented in the lit-erature.
The potential risk of hyperkalemia must be weighed against the benefits of succinylcholine
administration.
The use of succinylcholine in renal failure is
controver-sial. The increase in serum K+ in these patients is no
greater than in normal patients. Renal failure patients frequently have a
higher initial K+ level, and some authors suggest that even the
small increase normally associated with succinyl-choline may put these patients
at risk for dysrhythmias. Obviously, the starting K+ level is
critical to the decision regarding succinylcholine’s safety in these patients.
Hyperkalemic dysrhythmias following
succinylcholine must be rapidly diagnosed and treated. Hyperkalemia may respond
to induced alkalosis, which forces K+ back into the cell. This may
be accomplished by hyperventilation and bicarbonate administration. Calcium
chloride, 15 mg/kg intravenously, antagonizes the cardiac conduction effects of
hyperkalemia and may restore sinus rhythm. Insulin and glucose (10 U of regular
insulin in 25 mL of 50% dextrose) also drive K+ intracellularly.
Related Topics