Chapter: Microbiology and Immunology: Mycology, Fungi: Systemic Mycoses
Cryptococcosis
Cryptococcosis
Cryptococcosis, also called European blastomycosis, is an acute to chronic disease caused by an encapsulated yeast, C. neofor-mans. Cryptococcosis is the most common life-threateningfungal disease in patients with AIDS. It is the only systemic mycosis frequently documented from India.
Of the 19 species that comprise the genus Cryptococcus, human disease is associated with only C. neoformans. C. neofor-mans was first described by Busse, a pathologist, in 1984.
Kwon-Chung (1976) have described the perfect (i.e., sexual, teleomorphic) form of C. neoformans, which was named Filobasidiella neoformans. Prior to the identification of F. neoformans, which is mycelial, C. neoformans was consideredmonomorphic yeast.
Morphology
· C. neoformans is a true yeast.
· It is an oval and budding cyst and measures 3–6 mm in diameter. The yeast may be single or may have a single budding daughter cell.
· Within the host and in certain culture media, the yeast is surrounded by a wide polysaccharide capsule. The poly-saccharide capsule is composed of mannose, xylose, and glucuronic acid. This fungus forms a narrow-based bud in contrast to that of B. dermatitidis, which forms a broad-based bud. Rarely, pseudohyphae develop.
C. neoformans on SDA medium forms smooth, convex,cream-colored colonies at 20–37°C. Lactophenol cotton blue (LPCB) wet mount of the colony shows budding yeast cells.
neoformans has two varieties: C. neoformans var neoformans and C. neoformans var gattii. Based on antigenic specificity of the capsular polysaccharide, the species has been classified into four serotypes. These are serotypes A and D (C. neoformans var neoformans) and serotypes B and C (C. neoformans var gattii).
Pathogenesis and Immunity
The immune status of the host is the crucial factor in patho-genesis of cryptococcosis. C. neoformans usually causes most serious infections in patients with impaired CMI. These include:
· patients with AIDS,
· patients undergoing corticosteroid treatment,
· patients undergoing organ transplantation,
· patients with reticuloendothelial malignancy, and
· patients with sarcoidosis.
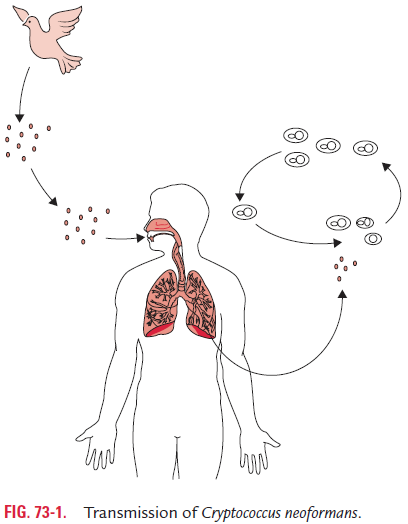
C. neoformans is primarily transmitted by inhalation (Fig. 73-1).Following inhalation, the yeasts are deposited into the pulmo-nary alveoli, in which they survive before they are phagocytosed by alveolar macrophages. Glucosylceramide synthase has been identified as an essential factor in the survival of C. neoformans in pulmonary alveoli.
Cryptococcal polysaccharide capsule has antiphagocytic properties. Hence, unencapsulated yeast are readily phagocy-tosed and destroyed than the encapsulated organisms, which are more resistant to phagocytosis. The antiphagocytic properties of the capsule prevent recognition of the yeast by phagocytes and inhibit leukocyte migration into the area of fungal replication.
◗ Host immunity
The host immunity in cryptococcal infection is mediated by both cellular and humoral responses. CMI is mediated by natural killer cells and T lymphocytes can inhibit or kill cryp-tococci. An increase in helper T-cell activity, skin test conver-sion, and a reduction in the number of viable organisms in the tissues indicates a successful host response against the fungus.
Humoral immunity is mediated by anticryptococcal antibodies and soluble anticryptococcal factors. Both anti-cryptococcal antibodies and the complement play a crucial role in facilitating the macrophage- and lymphocyte-mediated immune response to the organism.
Clinical Syndromes
C. neoformans causes (a) pulmonary cryptococcosis in immuno-competent hosts and in immunocompromised hosts, (b) CNS cryptococcosis, and (c) disseminated nonpulmonary non-CNS cryptococcosis.
◗ Pulmonary cryptococcosis
The clinical manifestations of pulmonary cryptococcosis are widely variable. Pulmonary disease varies from asymptom-atic colonization of the respiratory tract to acute respiratory distress syndrome affecting immunocompromised hosts. It depends on the immune status of the host.
◗ CNS cryptococcosis
Both the brain and meninges are involved in cryptococcal infection of the CNS infections. Meningitis and meningo-encephalitis are the most common manifestations. These are usually subacute or chronic in nature. Without specific therapy, the infection is invariably fatal. The patient dies due to the disease 2 weeks to several years after the symptom onset.
Disseminated nonpulmonary non-CNS cryptococcosis
Disseminated cryptococcosis includes the skin, prostate, and medullary cavity of the bones, next only to the lungs and CNS, and it occurs most commonly in patients with AIDS and other immunosuppressed conditions.
Epidemiology
C. neoformans is distributed worldwide. The incidence ofcryptococcosis is increasing and now it represents a major life-threatening fungal infection in patients with AIDS. Most cases of cryptococcosis are caused by serotypes A and D. C. neoformans var gattii is the most common variety that causes disease in immu-nocompetent patients. C. neoformans var neoformans is the most common variety that causes disease in immunocompromised patients, e.g., AIDS. C. neoformans is primarily transmitted by inha-lation (Fig. 73-1). Human-to-human transmission does not occur.
Laboratory Diagnosis
Laboratory diagnosis of cryptococcal infection is made by demonstration of the yeast in CSF, sputum, pus, and brain biopsy tissue by smear and culture. Methenamine silver or periodic acid-Schiff stains are used to stain the tissue specimens for demonstra-tion of the capsule of C. neoformans. Fixed tissue may also be stained with mucicarmine, which preferentially stains C. neoformans.
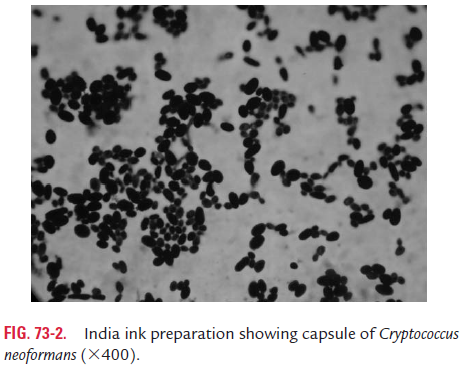
India ink preparation is commonly used to detect budding yeast cells in the CSF (Fig. 73-2). The capsule appears as a clear halo around the yeast cells. By this method, cryptococci can be demonstrated in 25–50% of patients with cryptococcal meningitis.
Gram-stained smear of the CSF shows Gram-positive yeast cells (Color Photo 63).
The culture of centrifuged CSF specimens confirms diagnosis of the condition. This fungus is identified based on its microscopic appearance, biochemical test results, and ability to grow at 37°C (98.6°F).
Latex agglutination test (LAT) is a frequently used serological test to detect cryptococcal polysaccharide antigen in the serum or CSF for diagnosis of meningitis. LAT is an extremely impor-tant adjunct to the diagnosis.
Treatment
Amphotericin B is the drug of choice for initial therapy in men-ingitis or other disseminated infections caused by C. neoformans. Amphotericin B may be used alone or in combination with flucytosine. The therapeutic goal for patients with cryptococcal disease not complicated by HIV infection is to achieve a per-manent cure of the fungal infection. The therapeutic goal for patients with concomitant HIV infection without a CD4 count of greater than 100 cells/mL is to control the acute infection, followed by lifelong suppression of C. neoformans.
Related Topics