Chapter: Basic Radiology : Scope of Diagnostic Imaging
Conventional Radiography
CONVENTIONAL
RADIOGRAPHY
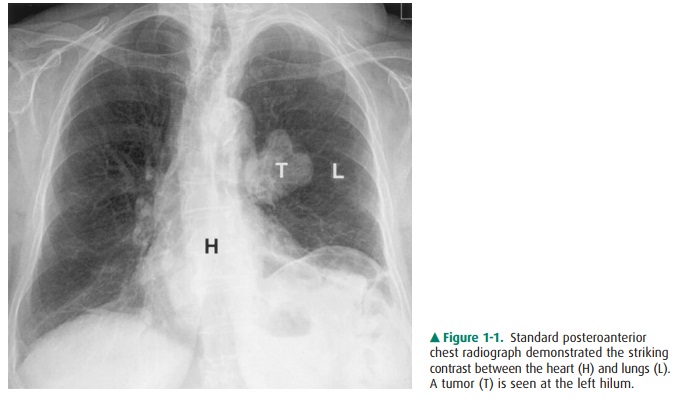
Conventional radiography refers to plain radiographs that are generated when x-ray film is exposed to
ionizing radiation and developed by photochemical process. During develop-ment,
the metallic silver on the x-ray film is precipitated, ren-dering the latent
image black. The amount of blackening on the film is proportional to the amount
of x-ray radiation ex-posure. Plain radiography relies on natural and physical
con-trast based on the density of material through which the x-ray radiation
must pass. Thus, gas, fat, soft tissue, and bone produce black, gray-black,
gray, and white radiographic im-ages, respectively, on film (Figure 1-1).
Although other image modalities
such as CT, ultra-sonography, and MR imaging are being used with increasing
frequency to replace plain radiographs, conventional radiog-raphy remains a
major modality in the evaluation of chest, breast, bone, and abdominal
diseases.
Computed radiography (CR) or
digital radiography is presently replacing conventional screen-film combination
techniques. The most common CR technique, photostimu-lable phosphor computed
radiography (PPCR), uses a phosphor-coated plate to replace the film-screen
combina-tion. When a cassette containing the phosphor-coated plate is exposed
to x-rays, the phosphor stores the absorbed x-ray energy. The exposed cassette
is then placed in a PPCR reader that uses a laser to stimulate release of
electrons, re-sulting in the emission of short-wavelength blue light. The
brightness of the blue light is dependent on the amount of absorbed x-ray
photon energy. This luminescence generates an electrical signal that is
reconstructed into a gray-scale image, which may be displayed on a monitor or
printed as a hard copy. Digital images generated from PPCR are capable of being
transmitted through a picture archiving and com-munications system (PACS),
similar to other digital images acquired from CT or MR facilities. PPCR is
better than plain radiography in linear response to a wide range of x-ray
exposure. However, PPCR provides less spatial resolution than plain
radiography. Another CR technique that is being developed uses an amorphous
selenium-coated plate, which directly converts x-ray photons into electrical
charges.
Fluoroscopy uses a fluorescent
screen instead of radi-ographic film to view real-time images generated when an
x-ray beam penetrates through a certain part of the body. An image intensifier
absorbs x-ray photons and produces a quantity of light on the monitor. The
brightness of the image is proportional to the number of incident photons
received. Fluoroscopy is a major modality used to examine the gas-trointestinal
tract. For example, fluoroscopy can be used to follow the course of contrast
materials through the gastroin-testinal tract, allowing the evaluation of both
structure and function. Spot filming or video recording may be used
syn-chronously with fluoroscopy to optimally demonstrate pathology. Fluoroscopy
is also used to monitor catheter placement during angiography and to guide
interventional procedures. In recent years, digital detectors (such as charge-coupled
devices, CCDs) have begun to replace video cameras on fluoroscopy units.
Conventional tomography produces
an image of one in-tended area by blurring structures superimposed on both
sides of a focus plane. This technique, however, has been largely replaced by
CT.
Mammography uses a film-screen
combination tech-nique to evaluate breast lesions for the early detection of
breast carcinoma. A mammographic unit is installed with a special x-ray tube
and a plastic breast-compression device. A standard mammogram obtains views in
two projections, producing craniocaudal (CC) and mediolateral oblique (MLO)
images of the breast. Additional images of the breast in other projections,
such as mediolateral (ML) views, and using diagnostic techniques such as magnification
and/or spot compression views may also be obtained to further char-acterize
potential pathologic findings. Ultrasonography (US) is also used in breast
imaging as a complementary modality to further characterize breast pathology.
Several image-guided breast interventional procedures, such as preoperative
needle placement for lesion localization and core needle biopsy using
stereotactic ultrasound or MR guidance, are widely available.
Contrast Studies
Contrast materials are used to
examine organs that do not have natural inherent contrast with surrounding
tissues. Contrast media are commonly used to evaluate the gastroin-testinal
tract, the urinary tract, the vascular system, and solid organs. Contrast media
used in MR imaging are described in the MR modality section.
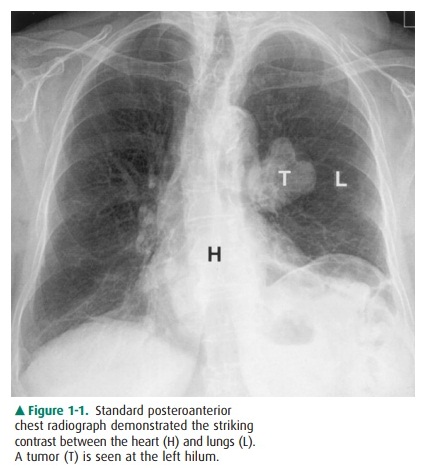
Barium suspension is still used
daily in the examination of the gastrointestinal tract. Barium suspension is a
safe contrast media that provides high imaging density on upper
gastrointestinal (UGI) series, small-bowel studies, and evaluation of the
colon. Both single-contrast and double-contrast techniques may be used to
evaluate the gastroin-testinal tract (Figure 1-2). In the single-contrast
study, barium suspension is administered alone. In the double-contrast study,
both barium and air are introduced to de-lineate the details of the mucosal
surface, which facilitates the identification of superficial lesions in the
bowel lumen. In the UGI double-contrast study, air is introduced into the bowel
lumen by administering oral effervescent agents. For double-contrast evaluation
of the lower GI tract with bar-ium enema, air is introduced into the bowel
lumen via di-rect inflation with a small pump through a rectal catheter.
Small-bowel contrast studies include peroral, enteroclysis, and retrograde
techniques. The peroral small-bowel study is performed by feeding barium
suspension to the patient and recording the progress of contrast through the
small bowel. Enteroclysis is performed by placing a catheter in the proximal
jejunum and infusing barium suspension through the catheter. Enteroclysis is
preferred for evaluat-ing focal small-bowel lesions or the cause of small-bowel
obstructions. Retrograde small-bowel examination is per-formed by retrograde
reflux of barium suspension into the small bowel during barium enema or via
direct injection through an ileostomy.
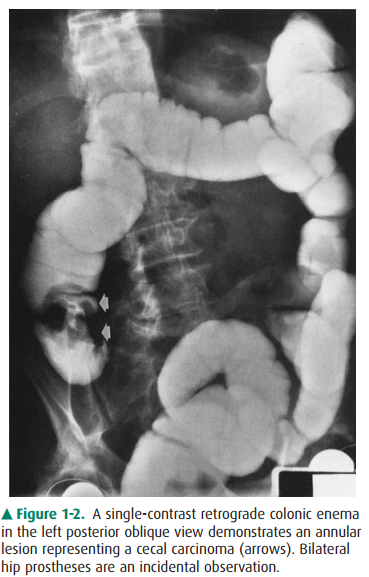
Figure 1-2. A single-contrast retrograde colonic enema in the left posterior oblique view demonstrates an annular lesion representing a cecal carcinoma (arrows). Bilateral hip prostheses are an incidental observation.
Water-soluble contrast media are
commonly used for an-giography, interventional procedures, intravenous
urogra-phy, and enhancement of CT. All water-soluble contrast media are
iodinated agents that are classified as high or low osmolar, ionic or nonionic,
and monomeric or dimeric in chemical nature. The iodine atoms in contrast
medium absorb x-rays in proportion to the concentration in the body when
radiographed. The most common water-soluble contrast media are the high osmolar
ionic contrast agents (diatrizoate and its derivatives). Low osmolar contrast
media include ionic (meglumine ioxaglate) and nonionic (iohexol, iopami-dol,
ioversol, iopromide) monomers, as well as nonionic dimers (iodixanol). Low
osmolar contrast media have an overall lower incidence of adverse reactions,
including nephrotoxicity and mortality, than high osmolar ionic agents;
however, lower osmolar agents are also three to five times more expensive.
The occurrence and severity of
adverse reactions after ad-ministration of iodinated contrast material are
unpre-dictable. These reactions are categorized as mild, moderate, or severe
based on degree of symptoms. Mild adverse reac-tions include nausea, vomiting,
and urticaria that do not re-quire treatment. The incidence of mild adverse
reactions may be less if using a lower osmolality contrast agent. Moderate
reactions include symptomatic urticaria, vasovagal events, mild bronchospasm,
and/or tachycardia that requires treat-ment. Severe and life-threatening
reactions, such as severe bronchospasm, laryngeal edema, seizure, severe
hypotension, and/or cardiac arrest, are unpredictable and require prompt
recognition and immediate treatment.
Contrast-induced nephropathy
(CIN) is characterized by renal dysfunction after intravenous administration of
iodi-nated contrast material. There is no standard definition of CIN. Findings
with CIN include percent increasing serum creatinine from baseline (such as 20%
to 50%) or increasing absolute serum creatinine above baseline (such as 0.5 to
2.0 mg/d) within 24 to 48 hours (or in 3 to 5 days). The inci-dence of CIN is
variable. Patients with renal failure or under-lying renal diseases are several
times more likely to develop CIN than those with normal renal function
following the administration of iodinated contrast material.
Water-soluble contrast agents are
used in the gastroin-testinal tract when barium suspension is contraindicated,
when perforation is suspected, when surgery is likely to fol-low imaging, when
confirmation of percutaneous catheter location is necessary, and when
gastrointestinal opacifica-tion is required during abdominal CT evaluation.
Unlike barium suspension, water-soluble contrast agents are readily absorbed by
the peritoneum if extraluminal extravasation occurs, but provide less image
density. High osmolar water-soluble contrast agents may cause severe pulmonary
edema if aspirated. High osmolar contrast agents may also cause fluid to shift
from the intravascular compartment into the bowel lumen, resulting in
hypovolemia and hypotension, which is less likely to occur with low osmolar
water-soluble contrast media.
Intravenous urography (IVU) uses
ionic or nonionic water-soluble contrast agents to evaluate the urinary tract.
Renal excretion/concentration of intravenously administered iodinated contrast
material opacifies the kidneys, ureters, and bladder approximately 10 minutes
postinjection. Intra-venous urography has been largely replaced over the past
decade by unenhanced helical CT evaluation. IVU, however, remains useful for
the evaluation of subtle uroepithelial neo-plasms and other diseases of the
renal collecting system, and it can provide additional information that
complements data from cross-sectional image modalities. Additional
contrast-enhanced imaging examinations of the genitourinary system include
cystography, voiding cystourethrography, and retro-grade urethrography to
evaluate the bladder and urethra.
Hysterosalpingography is
primarily used to evaluate the patency of fallopian tubes and uterine
abnormalities in pa-tients with infertility. Hysterosalpingography is also used
for postsurgical evaluation and to define anatomy for reanasto-mosis
procedures.
Hysterosalpingography is
performed by inserting a catheter into the uterus and subsequently injecting
water-soluble contrast medium (some institutions prefer oil-based iodine
contrast) to delineate the uterine cavity and the patency of the fallopian
tubes. A fluoroscopic spot image is taken once contrast medium fills the uterus
and fallopian tubes, but before spillage into the peritoneum. A second image is
takenafter fallopian tube spillage appears. A transcervical recanal-ization of
obstructed fallopian tube has been introduced to improve the fertility rate.
Angiography is the study of blood
vessels following intra-arterial or intravenous injection of water-soluble
contrast agents. A series of rapid exposures is made to follow the course of
the contrast medium through the examined blood vessels. Angiographic images are
recorded by standard or dig-ital imaging, and/or stored digitally.
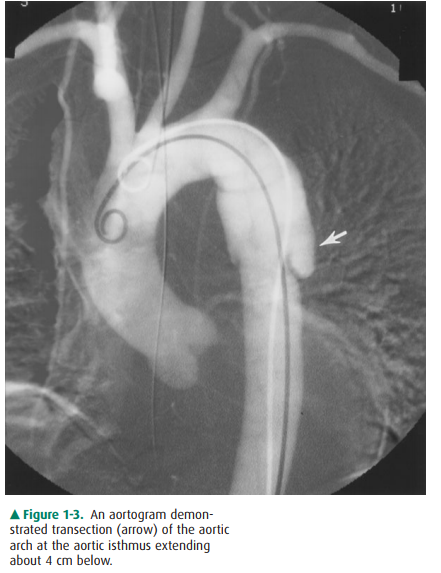
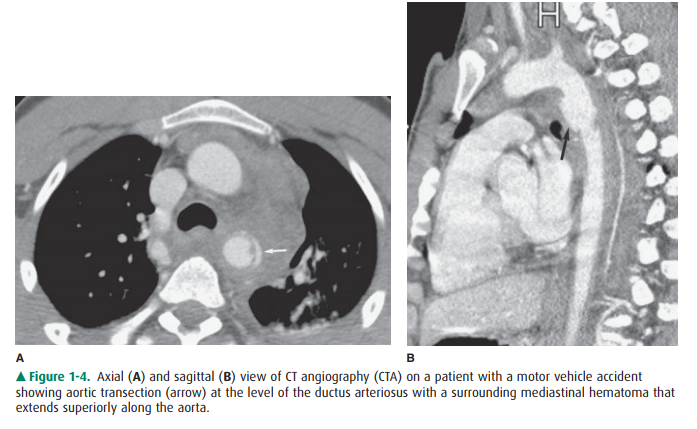
Thoracic aortography is performed
when there is suspi-cion of traumatic aortic injury, dissection (Figure 1-3),
or atherosclerotic aneurysm, and to evaluate cerebral and upper extremity
vascular disease. Multidetector CT has largely re-placed conventional
aortography as the initial modality to evaluate aortic trauma (Figure 1-4). Conventional
aortogra-phy, however, remains important in specific settings, such as planning
endovascular stent graft therapy and assessing small branch vessel injuries in
stable patients. Abdominal aortogra-phy is used to evaluate vessel origins in
vascular occlusive disease or prior to selective catheterization. Abdominal
aortography is also used for vascular mapping prior to aneurysm repair or other
intra-abdominal surgery. Coronary angiography is most commonly performed to
evaluate coro-nary occlusion. Pulmonary angiography is used in patients who are
suspected of having pulmonary embolus, especially in the setting of equivocal
results on ventilation-perfusion imaging. Inferior venacavography is performed
to evaluate for caval occlusion from venous thrombosis, obstruction or
compression by retroperitoneal lymphadenopathy, or fibro-sis. Inferior
venacavography is also performed to evaluate the configuration of the inferior
vena cava before filter place-ment. In recent years, conventional angiography
has been replaced by CT angiography and MR angiography.
Less commonly used contrast
studies include myelogra-phy (evaluating disk herniation and spinal cord
compres-sion), fistulography (sinus tracts for abscesses and cavities),
sialography (evaluating the salivary glands for ductal ob-struction or tumor),
galactography (assessing the breast duc-tal system), and oral cholecystography,
cholangiography (evaluating the biliary tree), and lymphangiography (assess-ing
lymph nodes and lymph channels for malignancies).
Computed Tomography
Computed tomography, an axial
tomographic technique, produces source images that are perpendicular to the
long axis of the body (Figure 1-5). Attenuation values generated by CT reflect
the density and atomic number of various tis-sues and are usually expressed as
relative attenuation coeffi-cients, or Hounsfield units (HUs). By definition,
the HUs of water and air are zero and –1,000, respectively. The HUs of soft
tissues range from 10 to 50, with fat demonstrating negative HU. Bone is at
least 1,000 HU. The contrast resolu-tion of vascular structures, organs, and
pathology, such as hypervascular neoplasms, can be enhanced following
intra-venous infusion of water-soluble contrast media. The type, volume, and
rate of administration as well as the scan delay time vary with specific study
indication and protocol. Addi-tionally, oral contrast material, namely,
water-soluble agents or barium suspensions, can be administered for improved
bowel visualization. Artifacts may be produced by patient motion or
high-density foreign bodies, such as surgical clips.
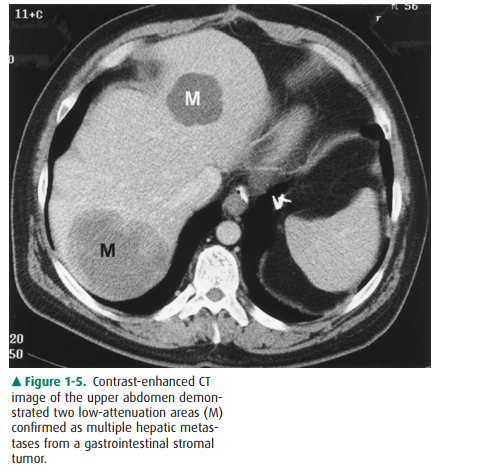
Figure 1-5. Contrast-enhanced CT image of the upper abdomen demon-strated two low-attenuation areas (M) confirmed as multiple hepatic metas-tases from a gastrointestinal stromal tumor.
Variety Scanners
Conventional CT scanners have
traditionally operated in a step-and-shoot mode, defined by data acquisition
and pa-tient positioning phases. During the data acquisition phase, the x-ray
tube rotates around the patient, who is maintained in a stationary position. A
complete set of projections are ac-quired at a prescribed scanning location
prior to the patient positioning phase. During this latter phase, the patient
is transported to the next prescribed scanning location.
The first helical (spiral) CT
scanner was introduced for clinical applications in the early 1990s. Helical CT
is charac-terized by continuous patient transport through the gantry while a
series of x-ray tube rotations simultaneously acquire volumetric data. These
dynamic acquisitions are typically ob-tained during a single breath hold of
about 20 to 30 seconds. Higher spatial resolution can be achieved with narrower
col-limations. The advantages of helical CT technology include reduced scan
times, improved speeds at which the volume of interest can be adequately
imaged, and increased ability to detect small lesions that may otherwise change
position in non-breath-hold studies. In addition, gains in scan speed permit
less contrast material to be administered for the same degree of vessel
opacification.
The evolution of multidetector CT
(MDCT) scanners has resulted from the combination of helical scanning with
multi-slice data acquisition. In this CT system, a multiple-row detec-tor array
is employed. Current state-of-the-art models are capable of acquiring 64, 128,
or 256 channels of helical data simultaneously. For a given length of anatomic
coverage, multidetector CT can reduce scan time, permit imaging with thinner
collimation, or both. The use of thinner collimation (0.4 mm to 2 mm) in
conjunction with high-resolution re-construction algorithms yields images of
higher spatial reso-lution (high-resolution CT), a technique commonly used for
evaluation of diffuse interstitial lung disease or the detection of pulmonary
nodules. Multidetector CT offers additional ad-vantages of decreased contrast
load, reduced respiratory and cardiac motion artifact, and enhanced multiplanar
recon-struction capabilities. These innovations have had a signifi-cant impact
on the development of CT angiography (CTA). Multidetector CT has replaced
conventional angiography as a primary modality in patients with acute aortic
injuries.
CT Angiography
CT angiography protocols combine
high-resolution volu-metric helical CT acquisitions with intravenous bolus
ad-ministration of iodinated contrast material. Using an MDCT scanner, images
are acquired during a single breath hold, en-suring that data acquisition will
commence during times of peak vascular opacification. This has permitted
successful imaging of entire vascular distributions, in addition to mini-mizing
motion artifact and increasing longitudinal spatial resolution, thus
potentially lowering administered contrast doses. The time between the start of
contrast injection and the commencement of scanning can be tailored in response
to a particular clinical question, permitting image acquisition during the
arterial, venous, and/or equilibrium phases. Ex-quisite anatomic detail of both
intraluminal and extralumi-nal structures is revealed using this technique,
including detection of intimal calcification and mural thrombosis. CT
angiography has become an important tool for assessment of the abdominal and
iliac arteries and their branches, the thoracic aorta, pulmonary arteries, and
intracranial and extracranial carotid circulation (Figure 1-6).

CT Colonography
CT colonography (virtual
colonoscopy), introduced in 1994, is a relatively new noninvasive method of
imaging the colon in which thin-section helical CT data are used to generate
two-dimensional or three-dimensional images of the colon. This technology has
been used primarily in the detection and characterization of colonic polyps,
rivaling the traditional colonoscopic approach and conventional barium enema
examinations. These images display the mucosal surface of the colon and
internal density of the detected lesions, as well as directly demonstrating the
bowel wall and extracolonic abdominal/pelvic structures.
Related Topics