Chapter: Psychiatric Mental Health Nursing : Assessment
Content of the Assessment
CONTENT OF THE ASSESSMENT
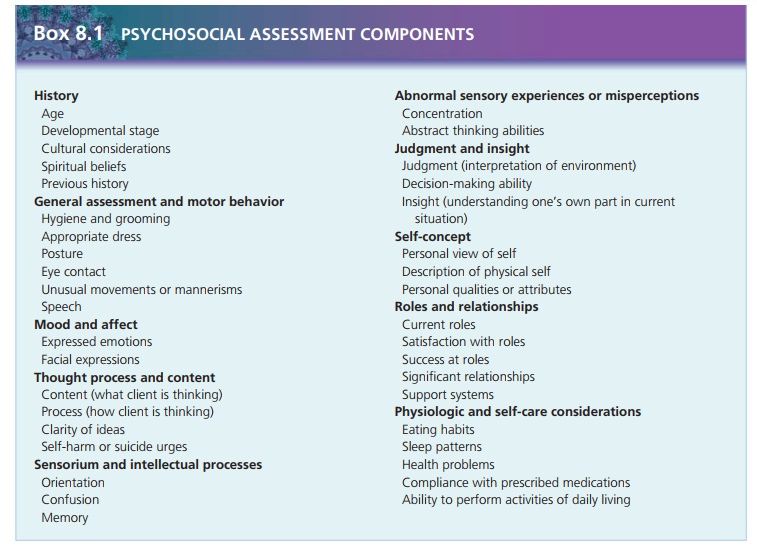
The information gathered in a psychosocial assessment can be
organized in many different ways. Most assessment tools or conceptual
frameworks contain similar categories with some variety in arrangement or
order. The nurse should use some kind of organizing framework so that he or she
can assess the client in a thorough and systematic way that lends itself to
analysis and serves as a basis for the client’s care. The framework for
psychosocial assessment discussed here and used throughout this textbook
contains the following components:
·
History
·
General appearance and motor behavior
·
Mood and affect
·
Thought process and content
·
Sensorium and intellectual processes
·
Judgment and insight
·
Self-concept
·
Roles and relationships
·
Physiologic and self-care concerns
History
Background assessments include the client’s history, age and
developmental stage, cultural and spiritual beliefs, and beliefs about health
and illness. The history of the cli-ent, as well as his or her family, may
provide some insight into the client’s current situation. For example, has the
cli-ent experienced similar difficulties in the past? Has theclient been
admitted to the hospital, and if so, what was that experience like? A family
history that is positive for alcoholism, bipolar disorder, or suicide is
significant because it increases the client’s risk for these problems.
The client’s chronological age and developmental stage are
important factors in the psychosocial assessment. The nurse evaluates the
client’s age and developmental level for congruence with expected norms. For
example, a client may be struggling with personal identity and attempting to
achieve independence from his or her parents. If the cli-ent is 17 years old,
these struggles are normal and antici-pated because these are two of the
primary developmental tasks for the adolescent. If the client is 35 years old
and still struggling with these issues of self-identity and inde-pendence, the
nurse will need to explore the situation. The client’s age and developmental
level also may be incongru-ent with expected norms if the client has a
developmental delay or mental retardation.
The nurse must be sensitive to the client’s cultural and spiritual
beliefs to avoid making inaccurate assumptions about his or her psychosocial
functioning (Schultz & Videbeck, 2009). Many cultures have beliefs and
values about a person’s role in society or acceptable social or personal
behavior that may differ from those of the nurse. Western cultures generally
expect that as a person reaches adulthood, he or she becomes financially
independent, leaves home, and makes his or her own life decisions. In contrast,
in some Eastern cultures, three generations may live in one household, and
elders of the family make major life decisions for all. Another example is the
assessment of eye contact. Western cultures consider good eye contact to be a
positive characteristic indicating self-esteem and pay-ing attention. People from
other cultures, such as Japan, consider such eye contact to be a sign of
disrespect.
The nurse must not stereotype clients. Just because a person’s
physical characteristics are consistent with a par-ticular race, he or she may
not have the attitudes, beliefs, and behaviors traditionally attributed to that
group. For example, many people of Asian ancestry have beliefs and values that
are more consistent with Western beliefs and values than with those typically
associated with Asian countries. To avoid making inaccurate assumptions, the
nurse must ask clients about the beliefs or health practices that are important
to them or how they view themselves in the context of society or relationships.
The nurse also must consider the client’s beliefs about health and
illness when assessing the client’s psychosocial functioning. Some people view
emotional or mental prob-lems as family concerns to be handled only among
family members. They may view seeking outside or professional help as a sign of
individual weakness. Others may believe that their problems can be solved only
with the right medi-cation, and they will not accept other forms of therapy.
Another common problem is the misconception that one should take medication
only when feeling sick. Many men-tal disorders, like some medical conditions,
may require clients to take medications on a long-term basis, perhaps even for
a lifetime. Just like people with diabetes must take insulin and people with
hypertension need antihyperten-sive medications, people with recurrent
depression may need to take antidepressants on a long-term basis.
General Appearance and Motor Behavior
The nurse assesses the client’s overall appearance, including
dress, hygiene, and grooming. Is the client appropriately dressed for his or
her age and the weather? Is the client unkempt or disheveled? Does the client
appear to be his or her stated age? The nurse also observes the client’s
posture, eye contact, facial expression, and any unusual tics or trem-ors. He
or she documents observations and examples of behaviors to avoid personal
judgment or misinterpretation. Specific terms used in making assessments of
general appearance and motor behavior include the following:
·
Automatisms: repeated purposeless
behaviors often in-dicative of anxiety, such as drumming fingers, twisting
locks of hair, or tapping the foot
·
Psychomotor retardation: overall slowed movements
·
Waxy flexibility: maintenance of posture or
position over time even when it is
awkward or uncomfortable
The nurse assesses the client’s speech for quantity, qual-ity, and
any abnormalities. Does the client talk nonstop? Does the client perseverate
(seem to be stuck on one topic and unable to move to another idea)? Are
responses a min-imal “yes” or “no” without elaboration? Is the content of the
client’s speech relevant to the question being asked? Is the rate of speech
fast or slow? Is the tone audible or loud? Does the client speak in a rhyming
manner? Does the cli-ent use neologisms
(invented words that have meaning only for the client)? The nurse notes any
speech difficul-ties such as stuttering or lisping.
Mood and Affect
Mood refers to the client’s
pervasive and enduring emo-tional state. Affect
is the outward expression of the client’s emotional state. The client may make
statements about feelings, such as “I’m depressed” or “I’m elated,” or the
nurse may infer the client’s mood from data such as pos-ture, gestures, tone of
voice, and facial expression. Thenurse also assesses for consistency among the
client’s mood, affect, and situation. For instance, the client may have an
angry facial expression but deny feeling angry or upset in any way. Or the
client may be talking about the recent loss of a family member while laughing
and smil-ing. The nurse must note such inconsistencies.
![]()
![]()
Common terms used in assessing affect include the following:
·
Blunted affect: showing little or a
slow-to-respond fa-cial expression
·
Broad affect: displaying a full range of
emotional expressions
·
Flat affect: showing no facial
expression
·
Inappropriate affect: displaying a facial
expression that is incongruent with
mood or situation; often silly or giddy regardless of circumstances
·
Restricted affect: displaying one type of
expression, usually serious or
somber.
The client’s mood may be described as happy, sad, depressed,
euphoric, anxious, or angry. When the client exhibits unpredictable and rapid
mood swings from depressed and crying to euphoria with no apparent stim-uli,
the mood is called labile (rapidly
changing).
The nurse may find it helpful to ask the client to esti-mate the
intensity of his or her mood. The nurse can do so by asking the client to rate
his or her mood on a scale of 1 to 10. For example, if the client reports being
depressed, the nurse might ask, “On a scale of 1 to 10, with 1 being least
depressed and 10 being most depressed, where would you place yourself right
now?”
Thought Process and Content
Thought process refers to how the client
thinks. The nurse can infer a
client’s thought process from speech and speech patterns. Thought content is what the client actually says. The nurse
assesses whether or not the client’s verbalizations make sense; that is, if
ideas are related and flow logically from one to the next. The nurse also must
determine whether the client seems preoccupied, as if talking or pay-ing
attention to someone or something else. When the nurse encounters clients with
marked difficulties in thought pro-cess and content, he or she may find it
helpful to ask focused questions requiring short answers. Common terms related
to the assessment of thought process and content include the following
(American Psychiatric Association, 2000):
·
Circumstantial thinking: a client eventually answers
a question but only after giving
excessive unnecessary detail
·
Delusion: a fixed false belief not
based in reality
·
Flight of ideas: excessive amount and rate
of speech composed of fragmented or
unrelated ideas
o Ideas of reference: client’s inaccurate interpretation that general events are personally
directed to him or![]()
![]() her, such as hearing a speech on the news and
believing the message had personal meaning
her, such as hearing a speech on the news and
believing the message had personal meaning
·
Loose associations: disorganized thinking that
jumps from one idea to another with
little or no evident rela-tion between the thoughts
·
Tangential thinking: wandering off the topic and
never providing the information
requested
·
Thought blocking: stopping abruptly in the
middle of a sentence or train of
thought; sometimes unable to con-tinue the idea
·
Thought broadcasting: a delusional belief that
others can hear or know what the
client is thinking
·
Thought insertion: a delusional belief that
others are putting ideas or thoughts
into the client’s head—that is, the ideas are not those of the client
·
Thought withdrawal: a delusional belief that
others are taking the client’s
thoughts away and the client is pow-erless to stop it
·
Word salad: flow of unconnected words
that convey no meaning to the
listener.
Related Topics