Chapter: Psychiatric Mental Health Nursing : Assessment
Assessment of Suicide or Harm Toward Others
ASSESSMENT OF SUICIDE OR HARM
TOWARD OTHERS
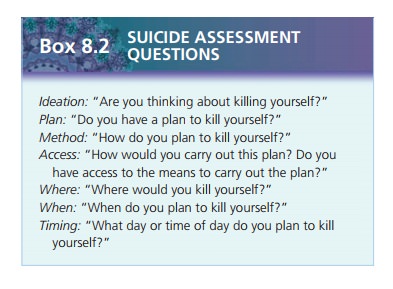
The nurse must determine whether the depressed or hope-less client
has suicidal ideation or a lethal plan. The nurse does so by asking the client
directly, “Do you have thoughts of suicide?” or “What thoughts of suicide have
you had?”
Likewise, if the client is angry, hostile, or making threat-ening
remarks about a family member, spouse, or anyone else, the nurse must ask if
the client has thoughts or plans about hurting that person. The nurse does so
by question-ing the client directly:
·
What thoughts have you had about hurting (person’s name)?
·
What is your plan?
·
What do you want to do to (person’s name)?
When a client makes specific threats or has a plan to harm another
person, health-care providers are legally obligated to warn the person who is
the target of the threats or plan. The legal term for this is duty to warn. This is one situation in
which the nurse must breach the client’s con-fidentiality to protect the
threatened person.
Sensorium and Intellectual Processes
Orientation
Orientation refers to the client’s recognition of person, place,
and time—that is, knowing who and where he or she is and the correct day, date,
and year. This is often documented as “oriented 3 3.” Occasionally, a fourth sphere, situation,
is added (whether or not the client accurately perceives his or her current
circumstances). Absence of correct information about person, place, and time is
referred to as disorienta-tion, or “oriented 3 1” (person only) or “oriented 3 2” (person and place). The
order of person, place, and time is significant. When a person is disoriented,
he or she first loses track of time, then place, and finally person.
Orienta-tion returns in the reverse order: first, the person knows who he or
she is, then realizes place, and finally time.
Disorientation is not synonymous with confusion. A confused person
cannot make sense of his or her sur-roundings or figure things out even though
he or she may be fully oriented.
Memory
The nurse directly assesses memory, both recent and remote, by
asking questions with verifiable answers. For example, if the nurse asks, “Do
you have any memory problems?” the client may inaccurately respond “no,” and
the nurse cannot verify that. Similarly, if the nurse asks, “What did you do
yesterday?” the nurse may be unable to verify the accuracy of the client’s
responses. Hence, questions to assess memory generally include the following:
·
What is the name of the current president?
·
Who was the president before that?
·
In what county do you live?
·
What is the capital of this state?
·
What is your social security number?
Ability to Concentrate
The nurse assesses the client’s ability to concentrate by asking
the client to perform certain tasks:
·
Spell the word world
backward.
·
Begin with the number 100, subtract 7, subtract 7 again, and so on.
This is called “serial sevens.”
·
Repeat the days of the week backward.
·
Perform a three-part task, such as “Take a piece of paper in your
right hand, fold it in half, and put it on the floor.” (The nurse should give
the instructions at one time.)
Abstract Thinking and Intellectual Abilities
When assessing intellectual functioning, the nurse must consider
the client’s level of formal education. Lack of for-mal education could hinder
performance in many tasks in this section of the assessment.
The nurse assesses the client’s ability to use abstract think-ing, which is to make associations or
interpretations about a situation or
comment. The nurse usually can do so by asking the client to interpret a common
proverb such as “a stitch in time saves nine.” If the client can explain the
proverb cor-rectly, his or her abstract thinking abilities are intact. If the
client provides a literal explanation of the proverb and can-not interpret its
meaning, abstract thinking abilities are lack-ing. When the client continually
gives literal translations, this is evidence of concrete thinking. For instance,
·
Proverb: A stitch in time saves nine.
Abstract meaning: If you take the time to fix
something now, you’ll avoid bigger
problems in the future.
Literal translation: Don’t forget to sew up holes
in your clothes (concrete thinking).
·
Proverb: People who live in glass
houses shouldn’t throw stones.
Abstract meaning: Don’t criticize others for
things you also may be guilty of
doing.
Literal translation: If you throw a stone at a
glass house, the glass will break
(concrete thinking).
The nurse also may assess the client’s intellectual func-tioning by
asking him or her to identify the similarities between pairs of objects, for
example, “What is similar about an apple and an orange?” or “What do the
newspa-per and the television have in common?”
Sensory-Perceptual Alterations
Some clients experience hallucinations (false sensory perceptions or perceptual experiences that do not really exist). Hallucinations can involve the five senses and bodily sensations. Auditory hallucinations (hearing voices) are the most common; visual hallucinations (see-ing things that don’t really exist) are the second most common. Initially, clients perceive hallucinations as real experiences, but later in the illness, they may recognize them as hallucinations.
Judgment and Insight
Judgment refers to the ability to
interpret one’s environ ment and situation correctly and to adapt one’s
behavior and decisions accordingly. Problems with judgment may be evidenced as
the client describes recent behavior and activ- ities that reflect a lack of
reasonable care for self or others. The nurse also may assess a client’s
judgment by asking the client hypo-thetical questions, such as “If you found a
stamped addressed envelope on the ground, what would you do?”
![]()
![]()
Insight is the ability to understand the true nature of one’s situation and accept some personal responsibility for that situation. The nurse frequently can infer insight from the client’s ability to describe realistically the strengths and weaknesses of his or her behavior. An example of poor insight would be a client who places all blame on others for his own behavior, saying, “It’s my wife’s fault that I drink and get into fights, because she nags me all the time.” This client is not accepting respon-sibility for his drinking and fighting. Another example of poor insight would be the client who expects all problems to be solved with little or no personal effort: “The prob-lem is my medication. As soon as the doctor gets the med-ication right, I’ll be just fine.”
Self-Concept
Self-concept is the way one views oneself
in terms of per-sonal worth and dignity. To assess a client’s self-concept, the
nurse can ask the client to describe himself or herself and what characteristics
he or she likes and what he or she would change. The client’s description of
self in terms of physical characteristics gives the nurse information about the
client’s body image, which is also part of self-concept.
![]()
![]() Also included in an assessment of self-concept
are the emotions that the client frequently experiences, such as sadness or
anger, and whether or not the client is comfort-able with those emotions. The
nurse also must assess the client’s coping strategies. He or she can do so by
asking, “What do you do when you have a problem? How do you solve it? What
usually works to deal with anger or disappointment?”
Also included in an assessment of self-concept
are the emotions that the client frequently experiences, such as sadness or
anger, and whether or not the client is comfort-able with those emotions. The
nurse also must assess the client’s coping strategies. He or she can do so by
asking, “What do you do when you have a problem? How do you solve it? What
usually works to deal with anger or disappointment?”
Roles and Relationships
People function in their community through various roles such as
mother, wife, son, daughter, teacher, secretary, or volunteer. The nurse
assesses the roles the client occupies, client satisfaction with those roles,
and whether the client believes he or she is fulfilling the roles adequately.
The number and type of roles may vary, but they usually include family, occupation,
and hobbies or activities. Family roles include son or daughter, sibling,
parent, child, and spouse or partner. Occupation roles can be related to a
career or school or both. The ability to fulfill a role or the lack of a
desired role is often central to the client’s psychosocial functioning. Changes
in roles also may be part of the cli-ent’s difficulty.
Relationships with other people are important to one’s social and
emotional health. Relationships vary in terms of significance, level of
intimacy or closeness, and intensity. The inability to sustain satisfying
relationships can result from mental health problems or can contribute to the
worsening of some problems. The nurse must assess the relationships in the
client’s life, the client’s satisfaction with those relationships, or any loss
of relationships. Com-mon questions include the following:
·
Do you feel close to your family?
·
Do you have or want a relationship with a significant other?
·
Are your relationships meeting your needs for compan-ionship or
intimacy?
·
Can you meet your sexual needs satisfactorily?
·
Have you been involved in any abusive relationships?
If the client’s family relationships seem to be a signifi-cant
source of stress or if the client is closely involved with his or her family, a
more in-depth assessment of this area may be useful.

Physiologic and Self-Care Considerations
When doing a psychosocial assessment, the nurse must include
physiologic functioning. Although a full physical health assessment may not be
indicated, emotional prob-lems often affect some areas of physiologic function.
Emotional problems can greatly affect eating and sleeping patterns: Under
stress, people may eat excessively or not atall and may sleep up to 20 hours a
day or may be unable to sleep more than 2 or 3 hours a night. Clients with
bipolar disorder may not eat or sleep for days. Clients with major depression
may not be able to get out of bed. Therefore, the nurse must assess the client’s
usual patterns of eating and sleeping and then determine how those patterns
have changed.
The nurse also asks the client if he or she has any major or
chronic health problems and if he or she takes pre-scribed medications as
ordered and follows dietary recom-mendations. The nurse also explores the
client’s use of alcohol and over-the-counter or illicit drugs. Such ques-tions
require nonjudgmental phrasing; the nurse must reassure the client that
truthful information is crucial in determining the client’s plan of care.
Noncompliance with prescribed medications is an important area. If
the client has stopped taking medication or is taking medication other than as
prescribed, the nurse must help the client feel comfortable enough to reveal
this information. The nurse also explores the barriers to com-pliance. Is the
client choosing noncompliance because of undesirable side effects? Has the
medication failed to pro-duce the desired results? Does the client have
difficulty obtaining the medication? Is the medication too expensive for the
client?
Related Topics