Chapter: Surgical Pathology Dissection : Common Uncomplicated Specimens
Common Uncomplicated Specimens : Surgical Pathology Dissection
Common Uncomplicated Specimens
The
dissection of tonsils, adenoids, hernia sacs, intervertebral discs, and
amputations for gan-grene are fairly straightforward, yet a brief discussion of
the appropriate handling of these specimens is important for two reasons.
First, because these specimens are so frequently en-countered, even small
mistakes in technique can be magnified over the course of handling numer-ous
specimens. By getting it right the first time, you can avoid developing bad
habits that are perpetuated with subsequent dissections. Second, mundane
specimens are particularly suscepti-ble to cursory and inattentive
examinations. As is true for novel and complex specimens, the pro-sector should
carefully examine the specimen and tailor a dissection that is attuned to the
clini-cal context.
Tonsils and Adenoids
The term
tonsils usually refers to the
palatine ton-sils. These are located laterally on each side of the oral cavity
as it communicates with the oro-pharynx. The term adenoids refers to the pharyn-geal tonsils. These are located along
the roof of the nasal cavity as it communicates with the naso-pharynx. Even
when these two structures are re-ceived together in the same specimen
container, they can easily be distinguished by their gross appearance. The
palatine tonsils are oval-shaped nodules of tissue. They are longer vertically
than they are horizontally. Their attached (i.e., lateral) surface is covered
by a thick fibrous capsule with adherent soft tissues, while their free (i.e.,
medial) surface is covered by a tan, glistening mucosa and is somewhat
cerebriform, which is due toa longitudinal cleft and stellate crypt openings.
The adenoids, on the other hand, tend to be flat and are frequently fragmented
when removed. Their free (mucosal) surfaces are disrupted by deep longitudinal
clefts that extend into the un-derlying lymphoid tissue.
The
palatine tonsils are usually removed from both sides of the oropharynx. Subtle
changes in the size, shape, and consistency of the ton-sils can be appreciated
by comparing the two tonsils. For example, enlargement that is due to an
infiltrative process may best be appre-ciated when the enlarged tonsil is
compared to the normal tonsil from the opposite side. After the tonsils and
adenoids are identified, they should be separately measured and de-scribed.
Look for exophytic masses, ulcerations, bulky enlargement, and any other gross
abnor-malities. Bivalve the tonsils and adenoids along the long axis of each,
and carefully inspect the cut surface for masses, abscess formation, or other
lesions.
Tonsils
and adenoids do not always need to be submitted for histologic evaluation. The
deci-sion to sample these specimens depends on the patient’s clinical history
and the gross findings. From our own experience, we have found that these
specimens should be sampled for
histologic evaluation if they meet any of the criteria listed below:
1. The age
of the patient is greater than 10 or less than 3 years.
2. The
tonsils or adenoids are grossly ab-normal.
3. The
tonsils or adenoids are greater than 3 cm.
4. There is
a size disparity between the two tonsils.
5. Histologic
evaluation is requested by the clini-cian or is indicated by the patient’s
clinical history.
If any
one of the above criteria is met, the tonsils and adenoids should be
appropriately sampled for histologic evaluation. One or two represen-tative
sections of the tonsils and adenoids are generally sufficient, but certain
conditions may require special processing or more extensive sec-tioning. For
example, diffusely enlarged tonsils or adenoids with architectural effacement
may suggest involvement by a lymphoproliferative disorder, and these should be
processed like a lymph node involved by a lymphoma (see Chap-ter 41). Sometimes
the tonsils are removed in an attempt to find an ‘‘occult’’ primary neoplasm in
a patient presenting with metastatic carcinoma to cervical lymph nodes. In this
situation, the tonsils should be serially sectioned and submit-ted in their
entirety for histologic evaluation. If the tonsils or adenoids do not meet any
of the above criteria, they do not need to be sampled for histologic
evaluation. After completing your gross description, place the specimen in
formalin and store it for at least 2 weeks.
Hernia Sacs
Hernia
sacs are pouches of peritoneum enclosing a hernia. Grossly and microscopically,
these are unimpressive specimens. They consist of vari-able amounts of fat,
fibroconnective tissue, and a mesothelium-lined peritoneum. Nonetheless, even
hernia sacs attest to the dictum that unex-pected but important pathologic
findings can be discovered in the most mundane of specimens. Indeed, a wide
range of pathologic findings have been documented in routinely resected hernia
sacs, ranging from endometriosis to malignant mesothelioma.
Measure
and describe the sac, taking note of any areas that appear hemorrhagic or
discolored. Palpate the specimen, and document the contents of the hernia sac
and whether any nodules are present. Small specimens do not require addi-tional
sectioning. Larger tissue fragments should be serially sectioned. Document the
gross appear-ance of the cut sections. Standards for submitting grossly normal
hernia sacs for histologic exami-nation vary from institution to institution.
In the current era of cost containment, some centershave eliminated the routine
histologic examina-tion of grossly normal pediatric hernia sacs. Nonetheless, all
grossly abnormal hernia sacs, all hernia sacs excised from adults, and all
hernia sacs from patients whose clinical history indicates a possible
histology-based diagnosis should be submitted for histologic evaluation. Most
hernia sacs can be entirely submitted in a single tissue cassette for
histologic evaluation. For larger speci-mens, a single cassette with sections
representing all components of the specimen is generally suf-ficient. More
extensive sampling may be neces-sary when focal lesions are identified or when
indicated by the patient’s clinical history.
Intervertebral Disk Material
Intervertebral
disks typically consist of multiple irregular fragments of fibrous tissue,
cartilage, and bone in variable proportions. These frag-ments are small and generally
do not require sectioning. Nonetheless, the prosector’s role in handling these
is not inconsequential. The appro-priate sampling and processing of these
speci-mens largely depends on the prosector’s skill at recognizing the various
components that are present.
Begin by
measuring the specimen. This can be done most efficiently by measuring the
aggre-gate dimensions of the specimen (not the dimen-sions of each individual
piece). Describe the type and appearance of the tissue received. Separate the
bone from the soft tissue fragments, and decalcify the pieces of bone so that
they can be sectioned by the histology laboratory (see Chap-ter 2). Keep in
mind that these small bone frag-ments do not require nearly as much time to
decalcify as sections from large bone resections. As is true for tonsils,
adenoids, and hernia sacs, some centers have eliminated histologic exami-nation
of disk tissue specimens after routine cervical and lumbar decompression.
Nonethe-less, routine disk tissue is submitted for histolo-gic examination at
most centers, and the tissues must be submitted when clinically indicated.
After the bone has been separated, submit the soft tissues for histologic
evaluation. Again, if all of the tissue does not easily fit into a single
tissue cassette, submit fragments that are rep-resentative of the specimen as a
whole. Some-times the patient’s clinical history may indicatemore extensive
sampling, as when metastatic car-cinoma is suspected clinically.
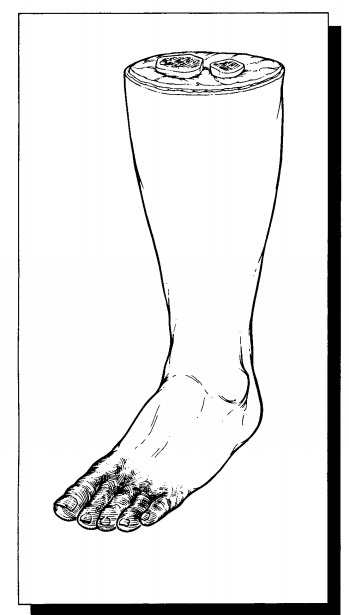
Amputations for Gangrene
Admittedly,
most amputation specimens are nei-ther small nor anatomically simple. On the
other hand, the dissection of amputations for gangrene is straightforward and
need not entail an inordi-nate amount of time and effort. The dissection of
these specimens, whether a resection of a digit or an entire limb, should focus
on two key questions: What are the nature and extent of the lesion (e.g.,
ulceration and gangrene)? What is the underly-ing pathologic process (e.g.,
vascular occlusion)? As for all specimens, the patient’s clinical history
should be clarified before the dissection of an amputation specimen is begun.
Clinical and ra-diographic findings may direct the dissection to the most
relevant areas of the specimen.
First,
measure the overall dimensions of the specimen. Make liberal use of anatomic
land-marks (e.g., tibial tubercle, lateral tibial malleo-lus) when measuring
the specimen and describing the location of any lesions. Next, examine the four
components of the specimen—the skin, soft tissues, bone, and vasculature. Begin
with the skin. Look for loss of hair, skin discoloration, and frank ulceration.
Note the location of these findings. Next, evaluate the soft tissues. Section
through any ulcers to determine the depth of the ulcer. Do the surrounding soft
tissuesappear necrotic? Also note whether the soft tis-sues at the surgical
margin appear viable. The bone underlying areas of ulceration and necrosis is
most likely to reveal pertinent pathology. Spe-cifically, section through the
deepest area of any ulcer, and determine if the underlying bone is grossly
involved by the inflammatory process. Fi-nally, evaluate the vasculature. For
amputations of the lower limbs, occlusive vascular disease can usually be
documented by performing a limited dissection of the anterior and posterior
tibial ar-teries. These can be located by sectioning deeply into the anterior
and posterior compartments of the calf. A deep transverse incision at midcalf
can usually accomplish this. When a complete dissec-tion of a particular
vascular tree is indicated, an anatomy text outlining the distribution of the
blood supply should be consulted.![]()
Sections
should be taken to demonstrate is-chemic changes in the skin, necrosis of the
soft tissue, inflammation in the underlying bone, oc-clusive disease of the
vascular tree, and viability of the soft tissues at the surgical margin. When
sampling the ulcer, include the adjacent epider-mis and the underlying
subcutaneous tissues. If the zone of ulceration and necrosis appears to extend
to the bone, submit a section of the bone immediately underlying the ulcer.
Submit cross sections of the major arteries, selectively sam-pling those
regions where the lumen is most stenotic. Finally, submit a transverse section
of the neurovascular bundle at the resection margin, along with some skin and
soft tissue from this region.
Related Topics