Chapter: Medical Immunology: Rheumatoid Arthritis
Clinical and Pathological Aspects of Rheumatoid Arthritis
CLINICAL AND PATHOLOGICAL ASPECTS OF RHEUMATOID ARTHRITIS
A. Localized Disease: Clinical Presentation
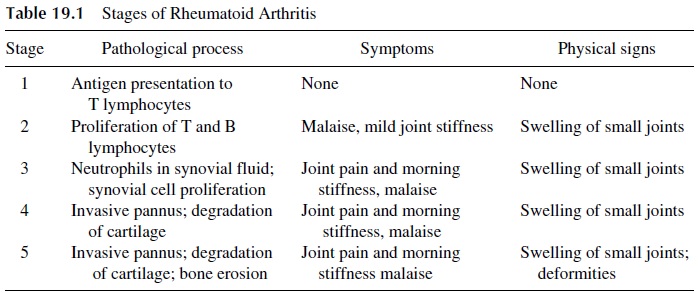
A chronic inflammatory process of the joints that progresses through different stages of increasing severity (Table 19.1) characterizes rheumatoid arthritis. The damage is reversible until cartilage and bones become involved (stages 4 and 5). At that time the changes be-come irreversible and result in severe functional impairment.
The most common clinical presentation of rheumatoid arthritis is the association of pain, swelling, and stiffness of the metacarpophalangeal and wrist joints, often associated with pain in the sole of the foot, indicating metatarso-phalangeal involvement. The disease is initially limited to small distal joints. With time, rheumatoid arthritis progresses from the distal to the proximal joints so that in the late stages, joints such as the ankles, knees, and elbows may become affected.
B. Pathological Manifestations of Localized Disease
In the early stages the inflammatory lesion is limited to the lining of the normal diarthro-dial joint. A thin membrane composed of two types of synoviocytes, the type A synovio
The earliest pathological changes, seen at the time of the initial symptoms, affect the endothelium of the microvasculature, whose permeability is increased, as judged by the de-velopment of edema and of a sparse inflammatory infiltrate of the edematous subsynovial space, in which polymorphonuclear leukocytes predominate. Several weeks later, hyperplasia of the synovial lining cells and perivascular lymphocytic infiltrates can be detected.
In the chronic stage, the size and number of the synovial lining cells increases and the synovial membrane takes a villous appearance. There is also subintimal hypertrophy with massive infiltration by lymphocytes, plasmablasts, and granulation tissue, forming what is known as pannus. This thick pannus behaves like a tumor and in the ensuing months and years continues to grow, protruding into the joint. The synovial space becomes filled by exudative fluid, and this progressive inflammation causes pain and limits motion. With time, the cartilage is eroded and there is progressive destruction of bones and tendons, leading to severe limitation of movement, flexion contractures, and severe mechanical deformities.
C. Systemic Involvement: Clinical Presentation
It is common to observe some signs and symptoms more indicative of a systemic disease, particularly those that are indicative of vasculitis. The most frequent sign is the formation of the rheumatoid nodules over pressure areas, such as the elbows. These nodules are an important clinical feature because, with rare exceptions, they are pathognomonic of RA in patients with chronic synovitis and generally indicate a poor prognosis.
D. Systemic Involvement: Pathological Manifestations
In contrast with the necrotizing vasculitis associated with systemic lupus erythematosus (SLE), due almost exclusively to immune complex deposition, the vasculitis seen in rheumatoid arthritis is associated with granuloma formation. This indicates that cell-medi-ated immune processes are also likely involved. Regardless of the exact pathogenesis of the vasculitic process, rheumatoid patients with vasculitis usually have persistently elevated levels of circulating immune complexes and, generally, a worse prognosis.
Histopathological studies of rheumatoid nodules show fibrinoid necrosis at the cen-ter of the nodule surrounded by histiocytes arranged in a radial palisade. The central necrotic areas are believed to be the seat of immune complex formation or deposition. When the disease has been present for some time, small brown spots may be noticed around the nailbed or associated with nodules. These indicate small areas of endarteritis.
E. The Overlap Syndrome
The overlap syndrome describes a clinical condition in which patients show variable degrees of association of rheumatoid arthritis and systemic lupus erythematosus. The exis-tence of this syndrome suggests that the demarcation between SLE and RA is not absolute, resulting in a clinical continuum between both disorders.
Clinically these patients present features of both diseases. Histopathological studies also show lesions characteristic of the two basic pathological components of RA and SLE (necrotizing vasculitis and granulomatous reactions). Serological studies in patients with the overlap syndrome demonstrate both antibodies characteristically found in SLE (e.g., anti-dsDNA) and antibodies typical of RA (rheumatoid factor, see below).
F. Other Related Diseases
Sjögren’s syndrome can present as an isolated entity or in association with rheumatoid arthritis, SLE, and other collagen diseases. It is characterized by dryness of the oral and ocular membranes (sicca syndrome), and the detection of rheumatoid factor is considered al-most essential for the diagnosis, even for those cases without clinical manifestations suggestive of rheumatoid arthritis.
Felty’s syndrome is an association of rheumatoid arthritis with neutropenia caused by antineutrophil antibodies. The spleen is often enlarged, possibly reflecting its involvement in the elimination of antibody-coated neutrophils.
Related Topics