Chapter: Obstetrics and Gynecology: Dysmenorrhea and Chronic Pelvic Pain
Chronic Pelvic Pain
CHRONIC PELVIC PAIN
Chronic pelvic pain is a common
disorder that repre-sents significant disability and utilization of resources.
Estimates suggest that 15% to 20% of women aged 18 to 50 years have chronic
pelvic pain that lasts longer than 1 year. Although there is no generally
accepted definition of chronic pelvic pain, one
proposed definition is noncyclic painlasting for more than 6 months that
localizes to the anatomic pelvis, anterior abdominal wall at or below the
umbilicus, the lumbosacral back, or the buttocks and is of sufficient severity
to cause functional disability or lead to medical care. Chronicpelvic pain
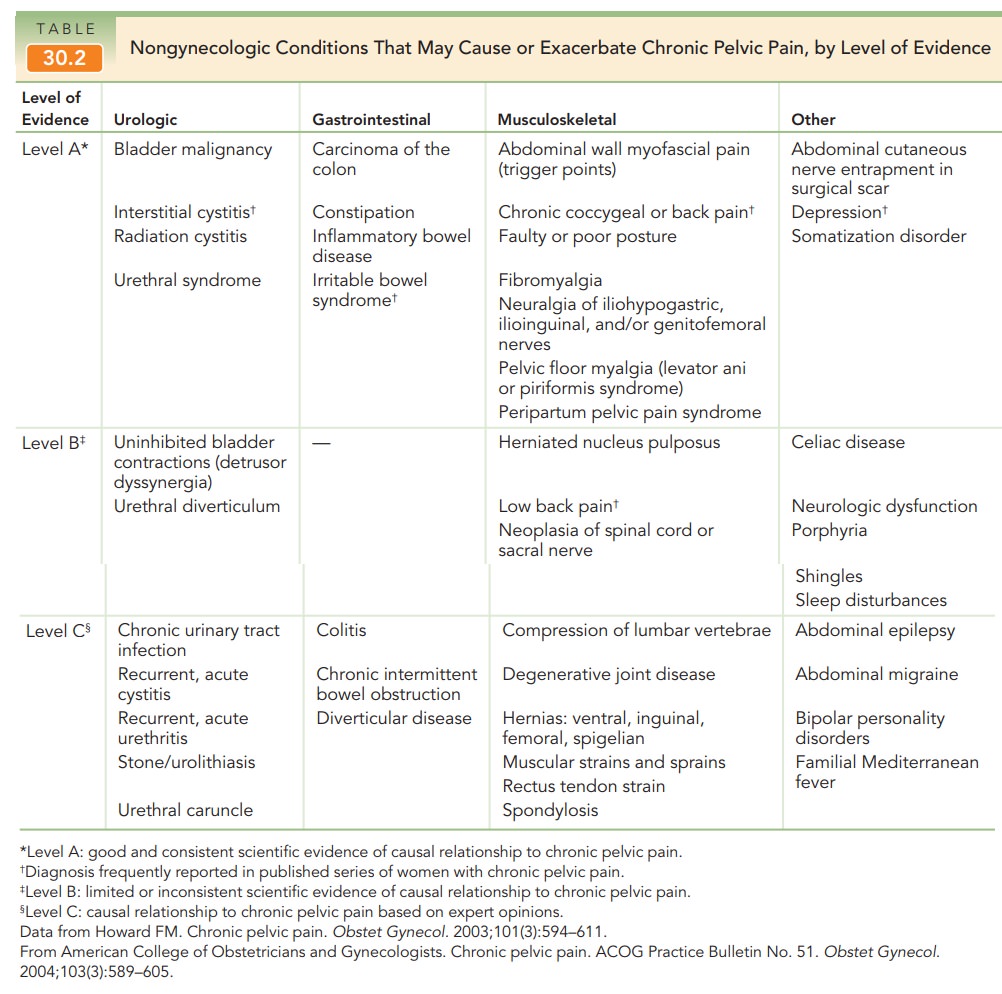
may be caused by diseases of the reproduc-tive, genitourinary, and
gastrointestinal tracts (Box 30.2 and Table 30.2). Other potential somatic
sources of pain include the pelvic bones, ligaments, muscles, and fascia.
Sometimes there is no clear etiology for the pain.
Assessment
The successful evaluation and
treatment of chronic pelvic pain requires time and a patient, caring physician.
The taking of the history and physical examination is a time in which the
physician may both gather information and establish a trusting rapport.
Effective management of this disease is dependent on a good doctor–patient
relation-ship, and the therapeutic effects of the relationship itself should
not be overlooked.
As with the evaluation of any
pain, attention must be paid to the description and timing of the symptoms
in-volved. The history should include a thorough medical, surgical, menstrual,
and sexual history. Inquiries should be made into the patient’s home and work
status, social his-tory, and family history (past and present). The patient
should be questioned about sleep disturbances and other signs of depression, as
well as a past history of physical and
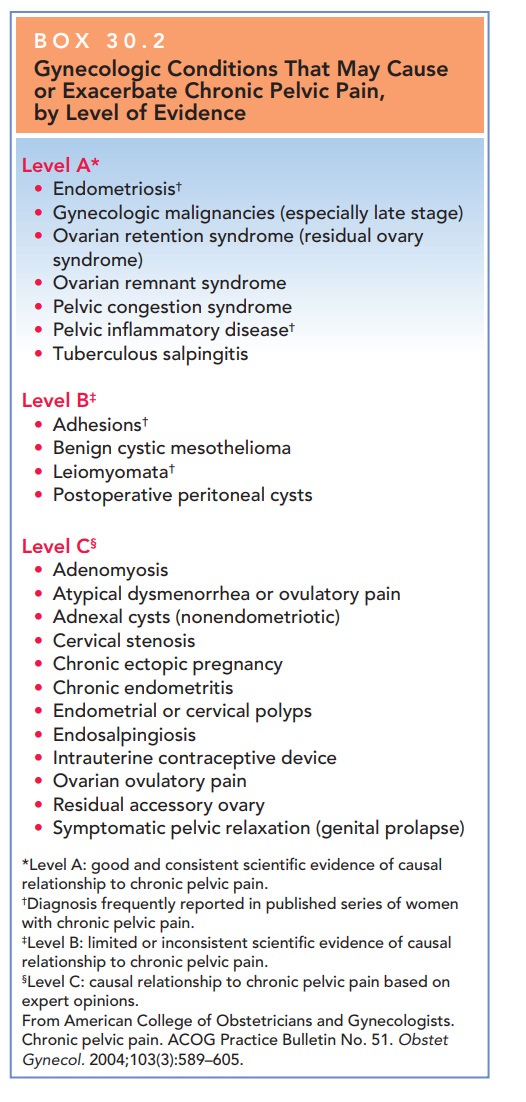
Box 30.2
Gynecologic Conditions That May Cause or Exacerbate Chronic Pelvic Pain, by Level of Evidence
Level A*
·
Endometriosis†
·
Gynecologic
malignancies (especially late stage)
·
Ovarian
retention syndrome (residual ovary syndrome)
·
Ovarian
remnant syndrome
·
Pelvic
congestion syndrome
·
Pelvic
inflammatory disease†
·
Tuberculous
salpingitis
Level B‡
·
Adhesions†
·
Benign
cystic mesothelioma
·
Leiomyomata†
·
Postoperative
peritoneal cysts
Level C§
·
Adenomyosis
·
Atypical
dysmenorrhea or ovulatory pain
·
Adnexal
cysts (nonendometriotic)
·
Cervical
stenosis
·
Chronic
ectopic pregnancy
·
Chronic
endometritis
·
Endometrial
or cervical polyps
·
Endosalpingiosis
·
Intrauterine
contraceptive device
·
Ovarian
ovulatory pain
·
Residual
accessory ovary
·
Symptomatic
pelvic relaxation (genital prolapse)
*Level
A: good and consistent scientific evidence of causal relationship to chronic
pelvic pain.
†Diagnosis frequently reported in published series of women with chronic pelvic pain.
‡Level B: limited or inconsistent scientific evidence of causal relationship to chronic pelvic pain.
§Level C: causal relationship to chronic pelvic pain based on expert opinions.
From
American College of Obstetricians and Gynecologists. Chronic pelvic pain. ACOG
Practice Bulletin No. 51. ObstetGynecol. 2004;103(3):589–605.
Studies have found
a significant correlation between a history of abuse and chronic pain. If a
history of abuse is obtained, the patient should also be screened for any
current physical or sexual abuse.
Physical examination of patients
with chronic pain is directed toward uncovering possible causative pathologies.
The patient should be asked to indicate the location of the pain as a guide to
further evaluation and to provide some indication of the character of the pain.
If the pain is local-ized, the patient will point to a specific location with a
single finger; if the pain is diffuse, the patient will use a sweeping motion
of the whole hand. Maneuvers that du-plicate the patient’s complaint should be
noted, but undue discomfort should be avoided to minimize guarding, which would
limit a thorough examination.
Many of
the same conditions that cause secondary dys-menorrhea may cause chronic pain
states. As in the evaluationof patients with dysmenorrhea,
cervical cultures should be obtained if infection is suspected. For most
patients, a reasonably accurate differential diagnosis can be established
through the history and physical examination. The wide range of differential
diagnoses possible in chronic pelvic pain lends itself to a multidisciplinary
approach, which might include psychiatric evaluation or testing. Consultation
with social workers, physical therapists, gastroenterologists,
anesthesiologists, orthopaedists, and others should be con-sidered. The use of
imaging technologies or laparoscopy may also be required to determine a
diagnosis. However, in approximately one-third of patients with chronic pelvic
pain who undergo laparoscopic evaluation, no identifi-able cause is found.
However, two-thirds of these patients have potential causes identified where
none was apparent before laparoscopy.
The evaluation should begin with
the presumption that there is an organic cause for the pain. Even in patients
with obvious psychosocial stress, organic pathology can and does occur. Only
when other reasonable causes have been ruled out should psychiatric diagnoses
such as som-atization, depression, or sleep and personality disorders be
entertained.
Conditions That Increase the Risk of Chronic Pelvic Pain
Common disorders in women with
chronic pelvic pain are pelvic inflammatory disease, irritable bowel syndrome,
interstitial cystitis, endometriosis, and adhesions. However, it is sometimes
difficult to pinpoint a specific cause of chronic pelvic pain, and many women
with chronic pelvic pain have more than 1 disease that might lead to pain.
Pelvic Inflammatory Disease
Approximately
18% to 35% of women who have had pelvic inflammatory disease will develop
chronic pelvic pain. Theexact mechanism is unknown,
but may involve chronic inflammation, adhesive disease, and the coexistence of
psychosocial factors.
IRRITABLE BOWEL SYNDROME
Irritable bowel syndrome (IBS) occurs in 50% to 80%of women with chronic pelvic pain.
The diagnosis of IBS is defined by the Rome II criteria: abdominopelvic pain
for 12 weeks (not necessarily consecutive) in the preced-ing 12 months that
cannot be explained by known disease, having at least two of the following
features: (1) relieved with defecation, (2) onset associated with a change in
the frequency of bowel movements (diarrhea or constipation), or (3) onset
associated with a change in the form of stool (loose, watery, with mucus, or pellet-like).
IBS is often usefully subcategorized for purposes of treatment depend-ing on
the predominant complaint: pain, diarrhea, con-stipation, or alternating
constipation and diarrhea. The pathophysiology of the syndrome is not clearly
identi-fied, but factors proposed to be involved include altered bowel
motility, visceral hypersensitivity, psychosocial factors (especially stress),
an imbalance of neurotransmit-ters (especially serotonin), and infection (often
indolent or subclinical). A history of childhood sexual or physical abuse is
highly correlated with the severity of symptoms experienced by those with IBS.
INTERSTITIAL CYSTITIS
Interstitial
cystitis is a chronic inflammatory condition ofthe bladder
that is often characterized by pelvic pain, uri-nary urgency and frequency, and
dyspareunia. The pro-posed etiology is a disruption of the glycosaminoglycan layer that normally coats the mucosa of the
bladder. The interstitial cystitis symptom index predicts the diagnosis of
interstitial cystitis and may be used to help determine whether cystoscopy is
indicated. Further evaluation can be done with bladder distention with water or
intravesical potassium sensitivity testing.
Related Topics