Chapter: Essentials of Psychiatry: Neurosurgery for Treatment Refractory Psychiatric Disorders
Characteristics of Patients Undergoing Neurosurgery for Treatment-refractory OCD and MDD
Characteristics
of Patients Undergoing Neurosurgery for Treatment-refractory OCD and MDD
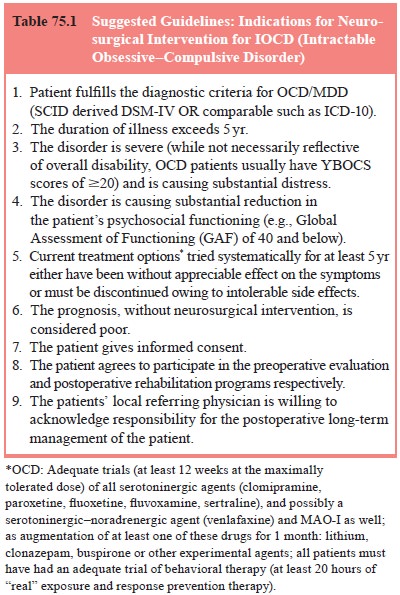
Though
selection criteria have not been standardized across cent-ers, a review of most
reported studies from several countries sug-gests that only a small number of
OCD or MDD patients who have not responded to a variety of exhaustive
treatments are considered for palliative neurosurgery. Treatments include
multiple adequate medication trials, an adequate trial of behavioral
treatment/psycho-therapy and electroconvulsive therapy (ECT) for MDD –
encom-passing patients who remain severely disabled for several years de-spite
these efforts (Table 75.1). In addition to the essential informed consent of
the patient, a panel of specialists, usually constituted at the institutional
level, carefully reviews all aspects of the patient’s condition before making a
consensus decision on surgery.
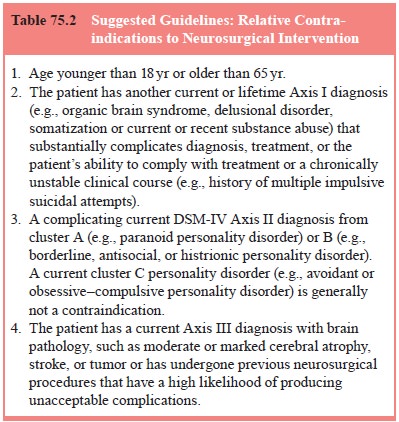
Severe,
chronic OCD and MDD referrals commonly present with comorbidities including
depression, obsessive–compulsive “psychosis”, substance abuse, history of
harmful behavior and personality disorders. The decision to offer surgery must
be eval-uated on a case-by-case basis, carefully considering the benefits and
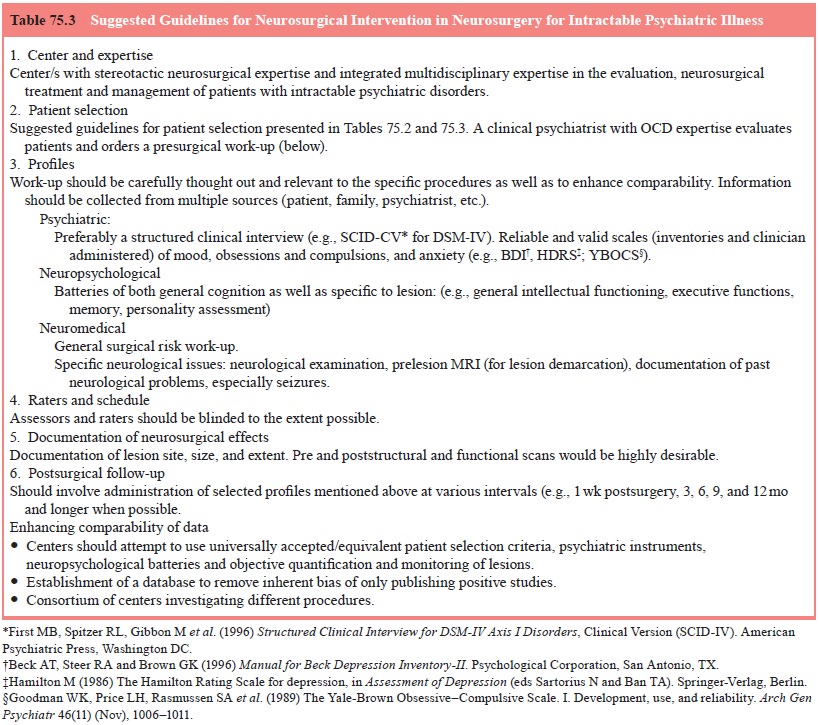
risks of intervention, alongside those of nonintervention. Tables 75.2 and 75.3
contain guidelines for indications and rela-tive contraindications for these
procedures evolved in the con-text of 25 years of experience with the
stereotactic cingulotomy procedure for intractable psychiatric disorder at one
center. (Massachusetts General Hospital (MGH): OCD Clinic and Cingulotomy
Program, Boston, MA, USA).
Related Topics