Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Cardiopulmonary Resuscitation
Cardiopulmonary Resuscitation: Airway
AIRWAY
Although the A of the mnemonic ABC
stands for airway, it shouldalsostand
for theinitial assessment of the
patient. Before CPR is initiated, unresponsive-ness is established and the
emergency response sys-tem is activated. During low blood flow states such as
cardiac arrest, oxygen delivery to the heart and brain is limited by blood flow
rather than by arterial oxygen content; thus, in the new guidelines, greater
emphasis is placed on immediate initiation of chest compressions than on rescuer
breaths.
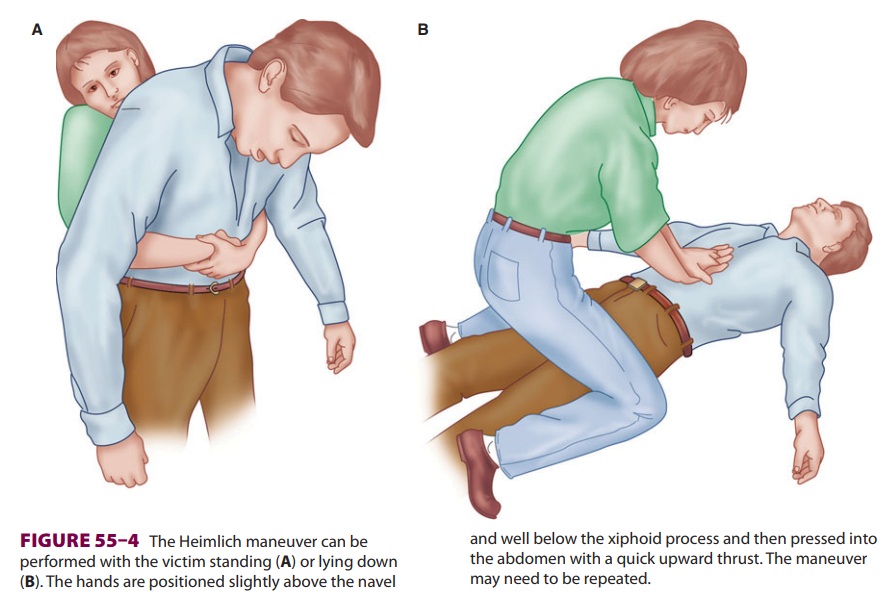
The patient is positioned supine on a firm sur-face. After initiation of
chest compressions, the airway is evaluated. The airway is most commonly
obstructed by posterior displacement of the tongue or epiglottis. If there is
no evidence of cervical spine instability, a head-tilt chin-lift should be
tried first (Figure 55–3 ). One hand (palm) is placed on the
patient’s forehead applying pressure to tilt the head back while lifting the
chin with the forefinger and index finger of the opposite hand. The jaw-thrust
may be more effective in opening the airway and is executed by placing both
hands on either side of the patient’s head, grasping the angles of the jaw, and
lifting.
Any vomitus or foreign body visible in the
mouth of an unconscious patient should be removed. If the patient is conscious
or if the foreign body
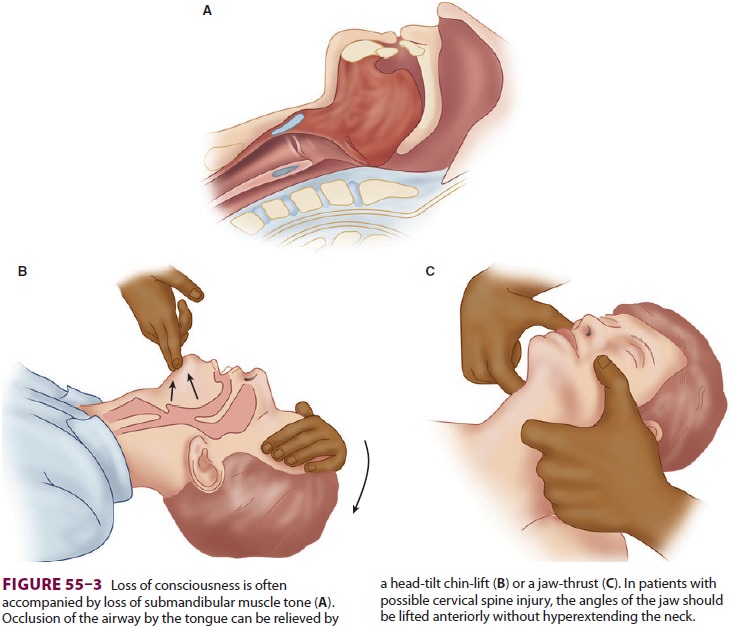
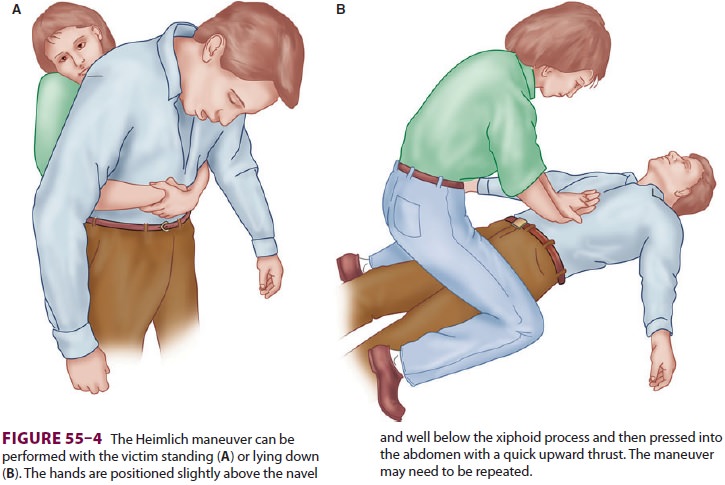
cannot be removed by a finger sweep, the
Heimlich maneuver is recommended. This subdiaphragmatic abdominal thrust
elevates the diaphragm, expelling a blast of air from the lungs that displaces
the foreign body (Figure 55–4).
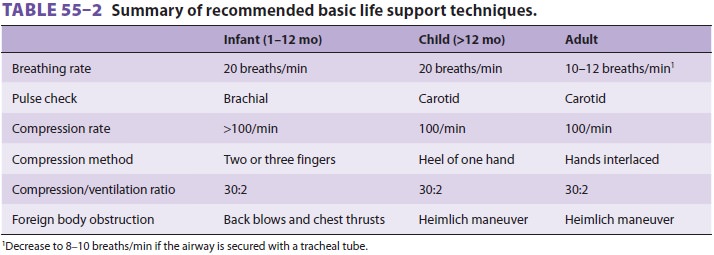
Complications of the Heimlich maneuver include rib fracture, trauma to the
internal viscera, and regurgitation. A combination of back blows and chest
thrusts is recommended to clear foreign body obstruction in infants (Table
55–2).
If after opening the airway there is no evidence of adequate breathing, the rescuer should initiate assisted ventilation, by inflating the victim’s lungs with each breath using mouth-to-mouth, mouth-to-nose, mouth-to-stoma, mouth-to-barrier device, mouth-to-face shield, or mouth-to-mask rescue breathing or by using a bag-mask device . Breaths are delivered slowly (inspiratory time of ½–1 s) with a smaller tidal volume [Vt] (approximately 700–1000 mL, smaller [400–600 mL] if supplemen-tal O2 is used) than was recommended in the past.With positive-pressure ventilation, even with a small Vt, gastric inflation with subsequent regurgi-tation and aspiration are possible. Therefore, as soon as it is feasible, the airway should be secured with a TT, or, if that is not possible, an alternative airway should be inserted. There is inadequate evidence to support the optimal timing of the placement of an artificial airway; however, chest compressions should not be interrupted for more than 10 seconds to place any airway. Alternative airways include the esophageal–tracheal Combitube (ETC), laryngeal mask airway (LMA), pharyngotracheal lumen air-way, King laryngeal tube, and cuffed oropharyngeal airway. The ETC and LMA, along with oral and nasopharyngeal airways, face masks, laryngoscopes,and TTs, are discussed. Of these, the LMA is increasingly preferred for in-hospital arrests. The 2010 CPR-ECC guidelines recommend a TT as the airway adjunct of choice if personnel skilled in placing it are available.
Independent of which airway adjunct is used, the guidelines state that rescuers must confirm TT placement with a Petco2 detector—an indicator,capnograph, or a capnometric device. The best choice for confirmation of TT placement is con-tinuous capnographic waveform analysis. All con-firmation devices are considered adjuncts to clinical conformation techniques (eg, auscultation). Once an artificial airway is successfully placed, it must becarefully secured with a tie or tape (25%ofairwaysare displaced during transportation).
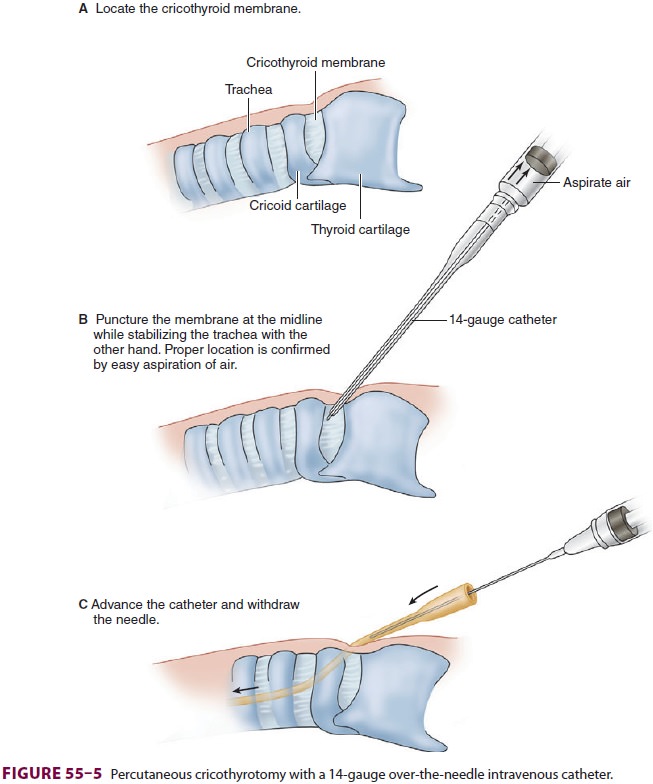
Some causes of airway obstruction may not be relieved
by conventional methods. Furthermore, tracheal intubation may be technically
impos-sible to perform (eg, severe facial trauma), or repeated attempts may be
unwise (eg, cervical spine trauma). In these circumstances, cricothyrotomy or
tracheotomy may be necessary. Cricothyrotomy involves placing a large
intravenous catheter or a commercially available cannula into the trachea
through the midline of the cricothyroid membrane (Figure 55–5). Proper location is confirmed by aspi-ration of air. A 12- or 14-gauge
catheter requires a driving pressure of 50 psi to generate sufficient gas flow
(for transtracheal jet ventilation). The catheter must be adequately secured to
the skin, as the jet ventilation pressure can otherwise easily propel the
catheter out of the trachea.
Various systems are available that connect a high-pressure source of
oxygen (eg, central wall oxygen, tank oxygen, or the anesthesia machine fresh
gas out-let) to the catheter (Figure 55–6). A hand-operated jet injector
or the oxygen flush valve of an anesthesia machine controls ventilation. The
addition of a pres-sure regulator minimizes the risk of barotrauma.
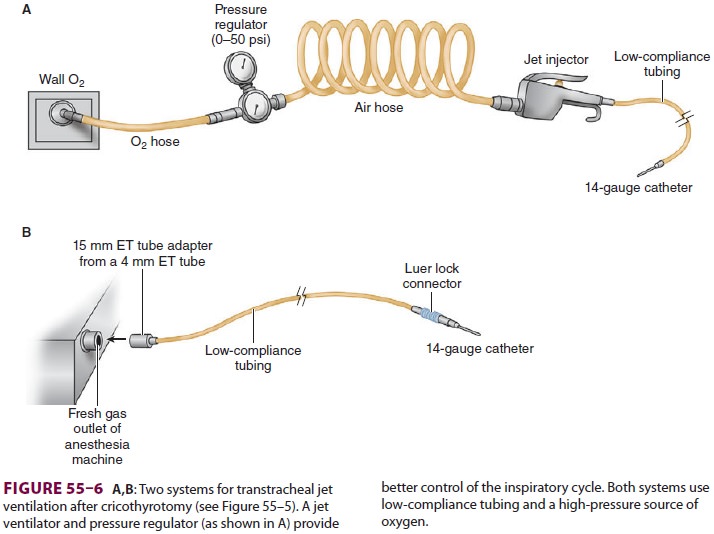
Regardless of which transtracheal jet
ventila-tion system is chosen, it must be readily available,
use low-compliance tubing, and have secure connections. Direct connection of a
12- or 14-gauge intravenous catheter to the anesthesia circle system does not
allow adequate ventilation because of the high compliance of the corrugated
breathing tub-ing and breathing bag. One cannot reliably deliver acceptable
ventilation through a 12- or 14-gauge catheter with a self-inflating
resuscitation bag.
Adequacy of ventilation—particularly
expira-tion—is judged by observation of chest wall move-ment and auscultation
of breath sounds. Acute complications include pneumothorax, subcutaneous
emphysema, mediastinal emphysema, bleeding, esophageal puncture, aspiration,
and respiratory acidosis. Long-term complications include tracheo-malacia,
subglottic stenosis, and vocal cord changes. Cricothyrotomy is not generally
recommended in children younger than 10 years of age.
Tracheotomy can be performed in a more con-trolled environment after
oxygenation has been restored by cricothyrotomy. A detailed description of
tracheotomy, however, is beyond the scope of this text.
Related Topics