Chapter: Modern Medical Toxicology: Cardiovascular Poisons: Cardiac Drugs and Lipid Lowering Agents
Cardiac Glycosides - Cardiovascular Poisons
CARDIAC GLYCOSIDES
The
history of cardiac glycosides in relation to the treatment of congestive heart
failure begins with the classic 1785
monograph by William Withering, who
wrote about the therapeutic and toxic properties of Digitalis purpurea. The common name of this plant is foxglove, and it grows well in the hilly
regions of Darjeeling, Nilgiris, and Kashmir. It is a biennial or perennial
herb belonging to family Scrophulariaceae, growing upto 1 to 1.5 metres in
height (Fig 23.1). Leaves are hairy,
ovate, toothed, and grey-green in colour, while the flowers are tubular and
pink or white in colour (Fig 23.2).
There is a related species, Digitalis
lanata, which is also rich in cardiac glycosides. Leavesconstitute the main
source of glycosides in both plants.

The following discussion will be mainly with reference to the digitalis glycosides digoxin and digitoxin, which are the most widely used cardiac glycosides. Other less commonly used glycosides include gitoxin, gitalin, digitonin, digitin (all from D.purpurea), lanatoside C, and deslanoside (both from D.lanata).
Uses
·
Treatment of mild to moderate heart failure
·
Control of ventricular response rate in patients with
chronic atrial fibrillation.
·
Digoxin increases left ventricular ejection fraction
resulting in improvement of heart failure symptoms. Digoxin is often used in
conjunction with a diuretic and an angiotensin-converting enzyme inhibitor for
the treatment of heart failure
Toxicokinetics
■■ Both digoxin and digitoxin are well absorbed
orally, but while the former is only moderately protein bound (25%), and has a
large apparent volume of distribution (adults
: 7 to 8 L/kg, neonates : 10 L/kg, infants : 16 L/kg), digitoxin is highly
protein bound (97%), and has a low apparent volume of distribution.
■■ Peak
serum concentrations of digoxin occur within 1.5 to 6 hours after an oral dose.
For digitoxin and digitalis leaf, the peak of cardiac toxicity is 4 to 12
hours.
■■ Digoxin
is metabolised to a very minor extent (about 16%) via hydrolysis, oxidation,
and conjugation. Metabolism is not dependant on the cytochrome P450 system.
■■ After
a single dose, digoxin is the major serum and urine metabolite of digitoxin. 60
to 80% of digoxin is excreted unchanged in the urine and the terminal half-life
is about 36 hours. Digitoxin has a much longer elimination half-life (about 100
hours).
■■ Most
of an administered dose of digoxin is distributed to skeletal muscle after
absorption (about 65%). The myocar-dium : plasma ratio is about 30 : 1.
Mode of Action
■■Digitalis glycosides inhibit active transport of Na+ and K+ across cell membranes by binding onto a specific site on the extracytoplasmic face of the alpha subunit of Na+-K+-ATPase. The force of contraction of the heart (positive inotropic effect) is increased due to increase in cytosolic Ca++ during systole. Both Na+ and Ca++ enter the myocar-dial cells during each cycle of depolarisation, contraction, and repolarisation. During repolarisation and relaxation, Ca++ is pumped back into the sarcoplasmic reticulum by Ca++-ATPase and is removed intracellularly by a Na+Ca++ exchanger, and a sarcolemmal Ca++-ATPase.
■■ Massive
acute cardiac glycoside overdose differs signifi-cantly from chronic toxicity.
In acute overdose, the sodium-potassium pump is poisoned, producing a fall in intracellular
potassium and a rise in extracellular potas-sium, which may be marked. The
normal membrane resting potential is reduced, and electrical conduction is
slowed, with eventual complete loss of myocardial electrical func-tion.
Clinically this results in high grade heart block, and eventually in asystole,
which may not respond to electrical pacing.
Adverse Effects
·
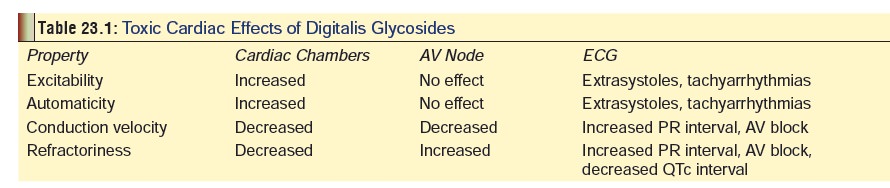
CVS: Arrhythmias are induced, the
more common types comprising non-paroxysmal atrial tachycardia, premature
ventricular extrasystoles, premature atrial and junctional extrasystoles, and
all grades of A-V block. The most serious arrhythmias are ventricular
tachycardia and ventricular fibrillation. The toxic cardiac effects of
digitalis glycosides are summarised in Table
23.1.
·
GIT: Anorexia, nausea, vomiting,
weakness.
·
CNS: Confusion, disorientation,
headache, and hallucina-tions (digitalis delirium).
·
Eye: Transient amblyopia, blurred
vision, scotomata, photo-phobia, and chromatopsia.
·
Miscellaneous: Gynaecomastia,
restlessness, diarrhoea in elderly.
Drug Interactions
·
Toxicity is increased by diuretics
(except potassium- sparing) and corticosteroids, because of hypokalaemia.
Common drugs that may reduce the elimination of cardiac glycosides and result
in digitalis intoxication include: amiodarone, propafenone, quinidine, and
verapamil.
·
Blood levels increased by Calcium
channel blockers, spironolactone, quinidine and Calcium salts.
·
Effectiveness reduced by phenytoin,
neomycin, sulfasala-zine, kaolin, pectin, and some antacids.
·
Metoclopramide interferes with
absorption.
·
Erythromycin, tetracycline, and
omeprazole increase absorption.
Clinical (Toxic) Features
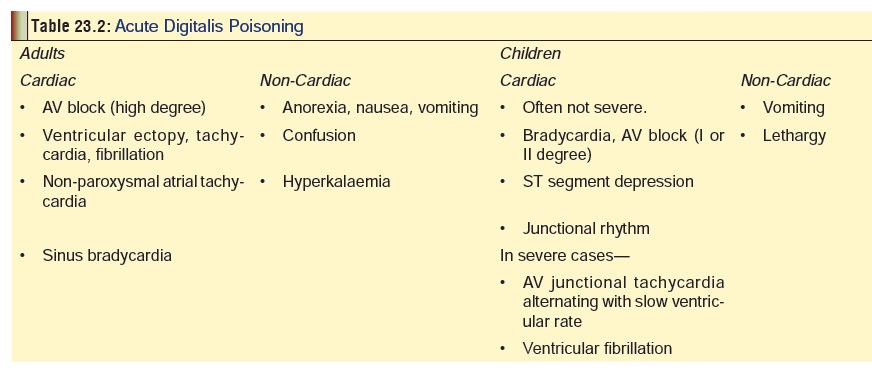
· Manifestations of digitalis overdose
are mentioned sepa-rately for adults and children in Table 23.2.
· Poisoning may be acute or chronic.
o In an acute ingestion, nausea and vomiting are promi-nent as well as evidence of cardiotoxicity.
o
In chronic poisoning, non-specific symptoms, such as malaise
and weakness predominate, as well as the classic, but rare, visual
disturbances.
· Lethargy, drowsiness, weakness,
paraesthesias, and headache may occur with digoxin toxicity. Signs of toxic
psychosis, including hallucinations, paranoia, agitation, confusion, and
delirium, may also occur. Often, CNS signs will be the only presentation of
digitalis toxicity, before cardiac or gastrointestinal symptoms.
· In many patients, though, the sole
evidence for digi-talis toxicity is the appearance of a cardiac arrhythmia.
Nonparoxysmal nodal tachycardia, atrial tachycardia with AV dissociation and
bidirectional ventricular tachycardia are common. Poor prognosis is associated
with old age, plasma digoxin level exceeding 15 ng/ml, and presence of AV block
(high degree), hyperkalaemia, or ventricular tachycardia.
· The hallmark of digitalis poisoning
is increased automa-ticity coupled with concomitant conduction delay. Every
known type of arrhythmia has been associated with digitalis intoxication,
including bradycardia, all degrees of heart block, PAT with block, bundle
branch block, nodal tachy-cardia with AV dissociation, atrial and ventricular
ectopy, and ventricular tachycardia and fibrillation; any or all may occur in
the same patient. Although no single arrhythmia is always present, commonly
appearing aberrations include frequent premature ventricular beats,
bradyarrhythmias, paroxysmal atrial tachycardia with block, junctional
tachy-cardia, and bidirectional ventricular tachycardia.
· Nausea, vomiting and abdominal pain
are early manifes-tations of acute and chronic toxicity. The most common
presenting symptoms in a paediatric patient are gastroin-testinal complaints,
sinus bradycardia, or first-degree AV block.
·
Hypotension and cardiac arrest may occur. Peak cardiac
effects generally occur 3 to 6 hours following digoxin over-dosage and may
persist for the ensuing 24 hours or longer. Profound hyperkalaemia after acute
ingestion is common.
· Non-occlusive mesenteric infarction
and refractory shock resulting in death have been reported following digoxin
toxicity.
·
Photophobia, amblyopia, miosis, and aberrations of colour
(predominance of yellow-green), are associated primarily with chronic toxicity.
Cones are 50-fold more sensitive than rods. Inhibition of light response by
photoreceptors is concentration-dependant and reversible.
Usual Fatal Dose
■■ Digitalis
leaf: 2 grams
■■ Gitalin:
15 mg
■■ Digoxin:
10 mg
■■ Digitoxin:
3 mg.
Acute digoxin ingestion of greater than 10 mg in a
previ-ously healthy adult, or 4 mg in a child may produce serious toxicity,
including cardiac arrest.
Therapeutic plasma concentration of digoxin should not
exceed 2 ng/ml. Concentrations exceeding 15 ng/ml are poten-tially fatal. Usual
therapeutic range: 0.5 to 2 ng/ml (0.64 to 2.56 nmol/L). Paediatric patients
appear to be more resistant to the cardiotoxic effects of digoxin than adults
at comparable serum levels. Children excrete digoxin more rapidly than older
patients. In overdose, the distribution phase may be prolonged, therefore,
serum digoxin levels may not be meaningful until approximately 6 hours
post-ingestion. Due to digoxin pharma-cokinetics, serum samples should not be
drawn within 6 hours of the previous dose, unless toxicity or overdose is
strongly suspected.
Treatment
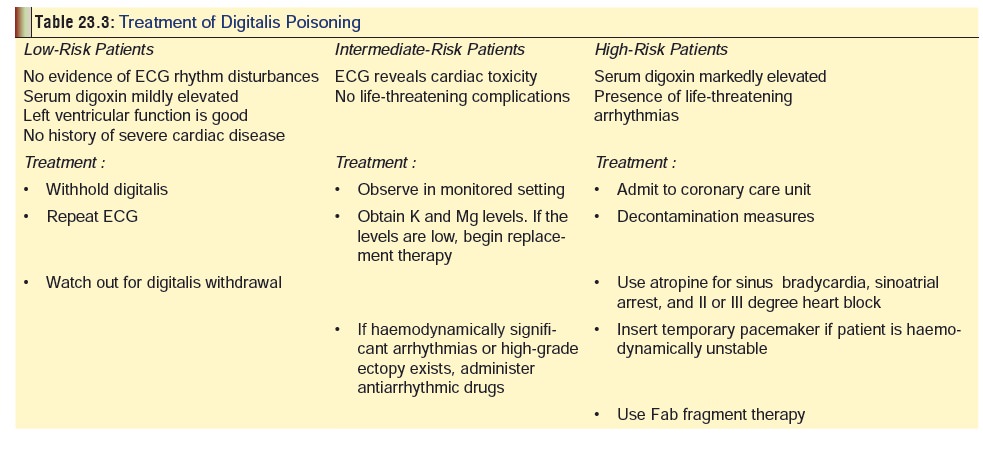
A
summary of the important treatment measures is given in Table 23.3.
1.
Initial Treatment
· Decontamination: Emesis, lavage, activated charcoal,* cathartic (as applicable). Emesis and stomach wash may enhance vagal stimulation and exacerbate bradycardia or heart block.
While digoxin immune Fab fragments are the preferred treatment for
severe or life-threatening cardiac glycoside intoxication, multiple dose
activated charcoal may be useful in situations in which Fab frag-ments are not
available. Whole bowel irrigation may be useful after large ingestions.
·
Forced diuresis, haemodialysis and haemoperfusion are
generally ineffective.
·
Monitor serum glycoside and potassium levels frequently.
Hyper- or hypokalaemia may occur.
·
All patients with a history of cardiac glycoside inges-tion
should have a baseline electrocardiogram, and serial serum levels and
electrolytes. Patients who remain asymptomatic with normal (or unchanged from
previous) baseline and follow-up electrocardiogram, declining serum levels, and
normal electrolytes, may be discharged after 6 hours of observation, following
psychiatric consultation if indicated.
2.
Advanced Treatment:
·
Antidote:Digoxin-specific
antibody fragments (Fab) -Fab therapy is of proven efficacy in not only
digitalis overdose, but also in oleander poisoning. Fab fragments are
administered intravenously. They bind intravascular free digoxin and then
diffuse into the interstitial space and bind free digoxin there. Digoxin and
potassium levels should be followed; continuous ECG monitoring is also
indicated. Therapy should be guided by the occurrence of life-threatening
arrhythmia, significant cardiac compromise or severe hyperkalaemia rather than
by digoxin concentration alone. In the absence of major clinical
signs/symptoms, an absolute digoxin concentration of greater than 10 nmol/L (6
hours after last dose) is an indication for the use of digoxin Fab fragments.
–– Indications for antidotal treatment include—
--
Ingestion of greater than 10 mg digoxin by an adult (4 mg by a child).
--
Potassium concentration exceeding 5 mEq/L. -- Serum digoxin level of more than
15 ng/ml. -- Progressive bradyarrhythmias or severe ventric-ular arrhythmias.
--Rapidly
progressing clinical symptomatology.
––
Dose—Each vial (Digibind) contains
38 mg of Fab fragments.
-- Dose depends on total body load (TBL) of
digoxin which can be calculated in 3 ways:
»» Estimate amount of digoxin ingested andasume 80%
bioavailability, i.e., x mg ingested
× 0.8 = TBL. (For digitoxin, bioavailability is taken as 100%).
»» Estimate serum
digoxin (or digitoxin) leveland use the following formula - Serum level (ng/ml)
x volume of distribution (Vd)weight (kg), where Vd is 5.6 L/kg
for digoxin, and 0.56 L/kg for digitoxin.
»»Use an empiric dose based on average requirements for an
acute or chronic over-dose in an adult or child: Adult = 10 to 20 vials (acute poisoning), 3 to 6 vials (chronicpoisoning); Child = 10 to 20
vials (acute poisoning), ¼ to ½ vial
(chronic poisoning).
–– Mode of Administration—Intravenous, over 30
minutes, via a 0.22 micron membrane filter.
Reconstitute
each vial with 4 ml of sterile water and use immediately (or within 4 hours if
refrigerated).
–– Adverse Effects—Allergic reactions (rare).
––
Disadvantages—Not yet available in India. Can be procured from abroad, but is
extremely expensive. A full course of antidotal therapy with Fab fragments can
cost several thousand dollars.
·
In the absence of Fab fragments,
ventricular irrita-bility can be treated with phenytoin or lignocaine.
Antiarrhythmics that may be useful include atropine, phenytoin and lignocaine.
Dose
-
––
Phenytoin: 50 mg/min, slow IV (maximum 1000 mg in adult, 15 to 20
mg/kg in child). Maintenance oral dose : 300 to 400 mg/day in adult, 6 to 10
mg/ kg/day in child.
–– Lignocaine: 1 mg/kg IV bolus, followed
by contin-uous infusion at 1 to 4 mg/min in adult, or 20 to 50 mcg/kg/min in
child. 15 minutes after initial bolus, an additional 1 mg/kg IV bolus should be
adminis-tered (both adult and child).
·
Atropine is useful in the management
of bradycardia, and varying degrees of heart block due to the digitalis-induced
effects of enhanced vagal tone on SA node rhythmicity and on conduction through
the AV node. In patients with severe supraventricular bradyarrhythmias, or high
degrees of AV block, 0.5 mg of atropine is given 0.1 mg). This dose can be
repeated every 5 minutes as necessary.
·
Magnesium (20 ml of 20% solution
over 20 minutes by slow infusion) has been reported to reverse digoxin induced
arrhythmias. It should be used extremely cautiously if at all in the presence
of renal failure.
·
External or transvenous pacemaker:
Pacemaker use should be considered in severe bradycardia and/or slow
ventricular rate due to second or high-degree AV block that fails to respond to
atropine and/or phenytoin when Percutaneous cardiopulmonary bypass has been
used for therapy resistant cardiac arrest due to digoxin over-for therapy
resistant cardiac arrest due to digoxin over-dose. Catecholamines may be needed
during bypass to maintain arterial pressure. This method may
providehaemodynamic support and sufficient tissue perfu-sion to allow
neutralisation by digoxin immune FAB in patients with cardiac arrest due to
massive cardiac glycoside overdoses.
·
Haemodialysis is ineffective in
removing cardiac glycosides but may assist in restoring serum potassium to
normal levels. Plain, charcoal, and immobilised antidigoxin antibody
haemoperfusion have all been used in digoxin and digitoxin overdose. None of
these techniques have proven utility in these ingestions. Treatment of
hypo-/hyperkalaemia, and hypomagne- saemia, as follows—
––
Hypokalaemia: IV potassium chloride in 0.9 or 0.45 % sodium
chloride, at a rate of 0.5 to 1.0 mEq/min (1 mEq/kg/hour in a child).
––
Hyperkalaemia: IV insulin, dextrose, sodium bicarbonate, and oral
ion-exchange resins (sodium polystyrene sulfonate). Digoxin immune Fab is
first-line treatment. Fab fragments and bicarbonate/ insulin/glucose should not
be used simultaneously because severe hypokalaemia may result. Do not administer calcium salts.
Calcium increases cardiac effects of glycosides, and may precipitate
arrhythmias. Hyperkalaemia is caused by poisoning of Na-K pump by glycoside, so
that intracellular potassium becomes extracellular; there is not increased
total body potassium.
![]() –– Hypermagnesaemia: 2 grams magnesium
sulfate (10%) IV over 20 minutes (25 mg/kg/dose in a child). Maintenance : 1 to
2 gm/hr (adult), 25 to 50 mg/kg/hr (child).
–– Hypermagnesaemia: 2 grams magnesium
sulfate (10%) IV over 20 minutes (25 mg/kg/dose in a child). Maintenance : 1 to
2 gm/hr (adult), 25 to 50 mg/kg/hr (child).
Related Topics