Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Deliriants
Cannabis - Deliriant Neurotoxic Poisons
Cannabis
Cannabis is among the earliest mind-altering drugs known to
man and has been around for at least 4000 years. Today, it is the world’s most
commonly used illicit drug, with more than 300 million regular users. In terms
of popularity ratings, it stands 4th among psychoactive drugs (after caffeine,
nicotine, and alcohol).
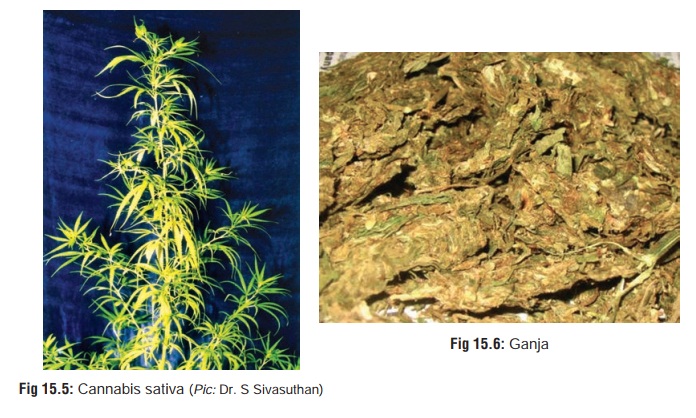
Source
Cannabis preparations (vide
infra) are derived from Indian hemp plant (Cannabis sativa) (Fig 15.5),
which is a hardy, aromatic annual herb that grows wild under most climatic
conditions. The plant grows to a height of 5 to 15 feet, and is characterised
by an odd number of leaflets on each leaf (varying from 5 to 9), all having
serrated or saw-tooth edges. The male and female flowers are borne on separate
plants. After pollination, the male plants die back.
Toxic Principles
The
main active principle is d9 (delta-9) tetrahydrocannabinol
(THC) which is a cannabinoid found in both the male and female plants. The
concentration of THC is highest in the bracts, flowers, and leaves, while it is
practically non-existent in the stem, root, and seeds. The THC content of the
plant varies greatly, and is probably controlled more by the type of seed than
by the soil or climatic conditions. Apart from THC, Cannabissativa contains a number of other cannabinoids,
includingcannabidiol, cannabinol, cannabidolic acid, cannabicyclol, and
cannabigerol. So far, more than 60 of these cannabinoids have been identified.
Uses
· The durable fibres of the woody trunk of cannabis, referred to collectively as Indian hemp, has been used for centuries to produce rope and twine, as well as fine or rough cloth. The cannabis plant is possibly the most efficient source of paper pulp, producing up to 5 times as much cellulose per acre per year, as trees.
![]()
· Cannabis seeds are used as food by
man, poultry, and other birds, as well as furnishing hemp-seed oil for paint
and soap.
· Therapeutic uses:
1.
THC in the form of a synthetic oral cannabinoid
(“dron-abinol”) has been shown to be effective in controlling the nausea and
diarrhoea associated with AIDS, as well as the nausea and vomiting caused by
chemotherapy for cancer or AIDS. It also increases appetite and produces weight
gain in both AIDS and cancer patients.
2.
Since smoked cannabis lowers intraocular pressure, it has
been suggested that this effect though short-lived (3 to 4 hours), can be
utilised for treating glaucoma.
3.
Some studies suggest a possible role for cannabis in the
treatment of multiple sclerosis, epilepsy, and dystonic states, though
convincing scientific evidence is lacking.
4.
THC possesses analgesic properties and has been tried in the
treatment of pain due to cancer.
Mode of Poisoning
Toxic
effects arise mainly from the abuse of various cannabis preparations for their
mind-altering properties.
· Marijuana: The term “marijuana” refers to any part of theplant or its
extract that is used to induce psychotomimetic or therapeutic effects. Synonyms
include Mary Jane, MJ, maconha, pot, weed, grass, puff and dagga.
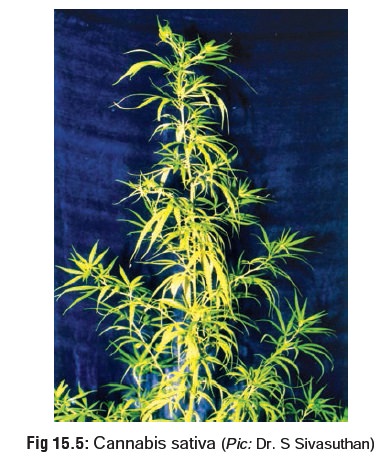
· Ganja: Although some texts refer to ganja as beingsynonymous with
marijuana, while others consider it to be a resinous mass composed of leaves
and bracts, in India (where the term actually originated), it is used to refer
to crushed leaves and inflorescences of female plants (Fig15.6). It is usually smoked in a pipe (“chillum”) or in theform
of cigarettes (“reefer” or “joint”). Ganja is said to contain 1 to 2% THC.
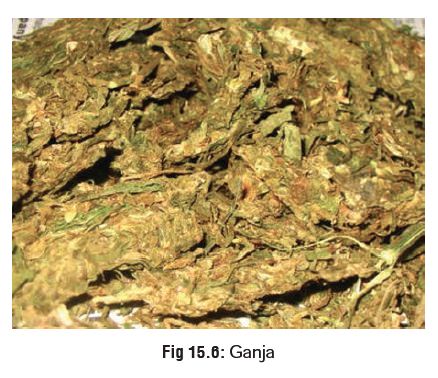
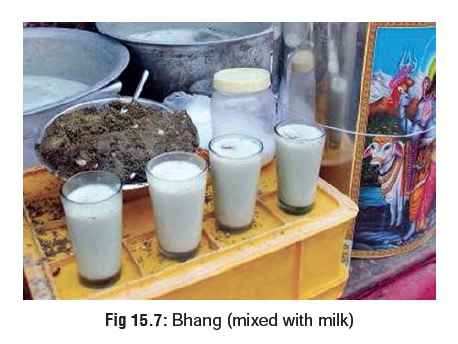
· Bhang: Bhang consists of dried mature leaves and flowerstems that are ground with water and mixed with milk (Fig15.7) or fruit juice. It is consumed by Hindus in India duringfestivals such as Holi and Shiv Ratri.
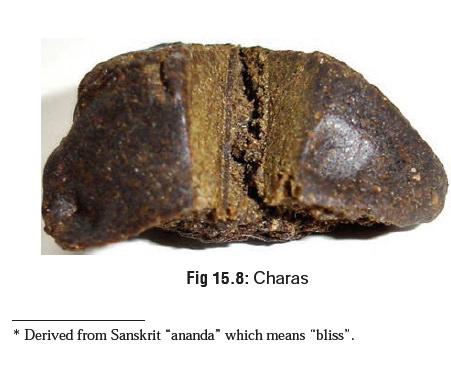
·
Hashish
(Charas): This preparation is made out of driedresin collected from
flower tops, and contains varying concentrations of THC up to 10% (Fig 15.8). It is popular in the Middle
East and North Africa. Hashish oil or “liquid hashish” is an alcohol or petrol
extract which occurs as a dark green viscous liquid with the consistency of
tar. It is the most potent of all cannabis preparations and contains 20 to 30%
(or more) THC.
·
Sinsemilla:
It is the most popular form of cannabis in theUSA, and refers to seedless
(unpollinated female) plant which averages 5% of THC.
·
Marijuana
“Blunts”: This is nothing but cheap cigarssliced open, packed with
cannabis, and resealed. The harsh stench of the cigar masks the characteristic
sweet smell of cannabis. Blunts are very popular among the youth in some parts
of the USA.
Mode of Action
·
Recently a receptor site has been
identified in rat brain that binds reversibly and selectively with
cannabinoids. Receptor binding was also found in the peripheral B
lymphocyte-rich areas such as the marginal zone of the spleen, nodular corona
of Peyer’s patches, and cortex of lymph nodes.
· Another recent development has been the isolation of an endogenous cannabinoid-like ligand within the brain, named “anandamide”.*
·
A cannabinoid antagonist was also
discovered that antago- nises cannabinoid-induced inhibition of adenylcyclase
and smooth muscle contraction.
·
All this suggests the presence of a
cannabinoid neuro- chemical pathway.
o It
appears that cannabinoids exert many of their actions by influencing several
neurotransmitter systems and their modulators. These include GABA, dopamine,
acetylcholine, histamine, serotonin, noradrenaline, and prostaglandins.
o Cannabinoid
receptor location and density in animal models has correlated well with
clinical effects in humans. The highest density of receptors occurs in the
basal ganglia and molecular layer of cerebellum, which correlates with its
interference in motor coordination. Intermediate levels of binding were found
in the hippocampus, dentate gyrus, and layers I and IV of cortex, consistent with
effects on short-term memory and cognition. Low receptor density is noted in
the brainstem areas controlling cardiovascular and respiratory functions, which
correlates with the cannabinoids’ known lack of lethality.
o After
binding to receptors, cannabinoids also produce effects through
second-messenger systems including inhibition of adenylcyclase and calcium
channels, and also probably by enhancing potassium channels activity.
Toxicokinetics
Smoking cannabis generally produces immediate effects, while
ingestion results in slow and unpredictable effects due to the instability
induced by the acidic environment of the stomach. The most important factor in
determining the bioavailability of THC happens to be the smoking dynamics
(manner in which the cannabis is smoked). It takes about 15 seconds for the
lungs to absorb the THC and transport it to the brain. Peak effects are seen in
10 to 30 minutes and may last for 1 to 4 hours. The mean terminal half-life of
THC in plasma of frequent cannabis smokers is 4.3 days (range: 2.6–12.6 days).
Drug Interactions
·
Concomitant use of cannabis and
ethanol produces additive effects on psychomotor performance.
·
Concomitant use of cannabis and
cocaine can greatly increase the heart rate.
·
Concomitant use of cannabis and phencyclidine
(“super- grass” or “superweed”) produces an intensely vivid hallu- cinogenic
experience.
Clinical (Toxic) Features
Acute Poisoning:
·
Euphoria with increased garrulity and hilarity, espe-cially
when smoked in a social group setting.
·
Temporal and spatial disorientation with intensification of
sensation (colours become brighter, sounds become more distinct, music is heard
with heightened fidelity) and increased clarity of perception.
·
At high doses, the user experiences hallucinations,
sedation, and sometimes dysphoria characterised by unpleasant sensations, fear,
and panic.
·
Sometimes an acute toxic psychosis is precipitated with
suicidal ideation, anxiety, and paranoia. Occasionally, schizophrenic symptoms
occur. Flashback phenomena have been reported.
·
Tachycardia, palpitations, hypotension (high doses).
·
Stimulation of appetite.
·
Bloodshot eyes due to conjunctival congestion.
·
Pupils are usually not affected.
Chronic Poisoning:
Chronic users of cannabis demonstrate tolerance to most of
the physical effects, while this is not very apparent in the case of mood and
behavioural changes.
·
Amotivational Syndrome: Chronic
indulgence is said to induce an amotivational syndrome characterised by apathy,
poor concentration, social withdrawal, and lack of motivation to study or work.
However, the actual existence of such a syndrome is being questioned by had not
attempted to adequately distinguish between the effects of cannabis and
pre-existing psychological status. In other words, it is difficult to determine
which came first, the drug or the amotivation.
·
Heavy cannabis users demonstrate an
increased tendency to develop manic, schizophreniform, and confusional
psychoses over a period of time. The development of acute psychosis after
chronic use is controversial because of questions about the contribu- tion of
premorbid personalities and multiple-drug use.
·
Medical Complications:
–– Chronic lung disease and carcinogenesis.
Experiments have revealed that cannabis smoking can cause a five-fold increase
in blood CoHb level and three-fold increase in the amount of tar inhaled when
compared with tobacco.
–– Cancers of mouth and larynx.
–– Aspergillosis: Studies have shown that
cannabis is often contaminated with
–– Aspergillus spores which can cause
aspergillosis in immunocompromised individuals.
–– Digital clubbing has been reported in chronic
hashish users.
Usual Fatal Dose
There
are no authentically documented cases of lethality from cannabis intoxication
alone. The few cases of fatality that have been reported have not adequately
ruled out the possibility of multiple-drug intoxication. In spite of such lack
of documented fatalities, some authors have suggested that the fatal dose for
IV cannabis is about 1 to 2 grams, while it is 700 grams for ingestion (of
bhang).
Diagnosis
Clinical:
·
Symptomatology
·
Characteristic ‘burnt rope’ odour in the breath of a recent
smoker.
Identification of suspected specimen: Suspend leaf orstem fragments in
several drops of chloral hydrate (10%) on a microscope slide and examine under
low power for characteristic “cystolith hairs”. These hairs look like bear
claws or elephant tusks. At the base of these claws is a wart-like cluster
composed of calcium carbonate deposit. Add a drop of 20% HCl and note the
gentle effervescent release of carbon dioxide gas in tiny bubbles.
Urine levels of cannabinoids:
·
THC is hydrophobic and accumulates in adipose tissue.
Screening tests may be positive for up to 70 or more days, depending on the
cut-off levels used and the individual’s lipid stores of THC. Some
investigators state that after using three or more joints per day, an
individual who then stops smoking cannabis completely and adopts an excessive
fitness programme mobilising body fat, will test positive for urinary THC (at
50 to 100 ng/ml) for more than 2 months. An individual who smokes an occasional
joint will test positive (at 500 to 1000 ng/ml) f3 to 4 days.
·
False positive results may occur with therapeutic use of
ibuprofen, fenoprofen, and naproxen. False negatives may result from dilution,
diuretic use, common salt, or other contaminants. Concomitant testing of urine
specific gravity, pH, temperature, and creatinine could help in eliminating
these confounders.
Treatment
Acute Poisoning:
·
Decontamination measures in cases of ingestion.
·
Acute psychotic reactions respond to benzodiazepines.
·
Supportive measures.
Chronic Poisoning:
·
Psychosocial therapy consisting of attempts to promote
realistic and rewarding alternatives to the drug and associated life styles,
along with a commitment to abstinence from self-administered or unprescribed
psychotropic drugs. A combination of interventions is recommended, including
urine testing, participation in multi-step programmes, education about drug
effects, drug counselling, psychotherapy, and family therapy.
·
Drug-focussed group therapy comprising strategies such as
social pressure to reinforce abstinence, teaching socialisation and problem
solving skills, reducing stress and the sense of isolation common with drug
abuse, relapse prevention exercises, and varying degrees of confrontation.
· Short-term use of anxiolytic agents such as benzodiaz-epines may be necessary in some cases when anxiety symptoms are severe.
·
Short-term use of antipsychotic medication may be required
if there are persistent delusional ideas or frightening
flash backs.
Medicosocial and Forensic Issue
·
Cannabis has been around for
thousands of years, initially touted for its “medical” uses, and later
condemned for its abuse potential. The first reference to the medical use of
cannabis is in a pharmacy book written about 2737 BC by the Chinese Emperor
Shen Nung, who recommended it for “absent-mindedness, female weakness, gout,
rheu- matism, malaria, beri beri, and constipation”.
·
The mind-altering properties of
cannabis probably did not receive wide attention until about 1000 BC when it
became an integral part of Hindu culture in India. After AD 500, cannabis began
creeping westward, and references to it began appearing in Persian and Arabic
literature.
·
Cannabis was brought to Europe by
Napoleon’s soldiers returning from Egypt in the early part of 19th century. It
made its entry into the USA at about 1920 when Mexican labourers smuggled the
weed across the border into Texas. Its popularity spread quickly, and by 1937
most of the American states had enacted laws prohibiting the use or possession
of marijuana. Today, inspite of all efforts at minimising the abuse of
cannabis, the drug is the most commonly used illicit substance in the USA.
·
The use of cannabis among youth
reached its peak in the 1960s when the drug became associated with social
protest. The hippie generation (“flower people”) was particularly fond of
cannabis, to whom it was a “gateway drug” opening the doors to more potent
“hard drugs” such as opiates and hallucinogens.
·
Recent reports of medical uses of
cannabis have led to the resurgence of “pot culture” beginning with the 1990s.
Consumption of cannabis in various forms has always been popular in India.
Sanyasis and temple poojaris use it to induce a trance-like state for the
purpose of religious meditation. There are several festivals such as Holi and
Shiva Ratri when widespread consumption occurs even among the general populace.
·
While long-term cannabis use can
cause serious health problems (vide supra),
acute intoxication sometimes leads to medicolegal complications. The danger
lies in the capacity of cannabis to interfere with motor skills and judgement.
Operating a motor vehicle or other machinery under the influence of the drug
could lead to potential loss of life or limb.
·
Occasional acute psychotic reactions
precipitated by long- term heavy cannabis use can cause the user to “run amok”
in homicidal frenzy. This became well known during the Vietnam war when several
American soldiers began suffering from acute toxic psychosis arising out of heavy
abuse. Cannabis is also known to induce suicidal ideation brought on by anxiety
and paranoia.
·
While cannabis does not appear to
have teratogenic effects on the foetus, some studies have indicated that
infants whose mothers had used the drug during pregnancy exhib- ited impaired
foetal growth.
Related Topics