Chapter: Medical Surgical Nursing: Assessment of Integumentary Function
Assessment of Integumentary Function
Assessment
HEALTH HISTORY AND CLINICAL MANIFESTATIONS
When
caring for patients with dermatologic disorders, the nurse obtains important
information through the health history and di-rect observations. The nurse’s
skill in physical assessment and an understanding of the anatomy and function
of the skin can en-sure that deviations from normal are recognized, reported,
and documented.
During the health history interview, the nurse asks about any family and personal history of skin allergies, allergic reactions to food, medications, chemicals, previous skin problems, and skin cancer.
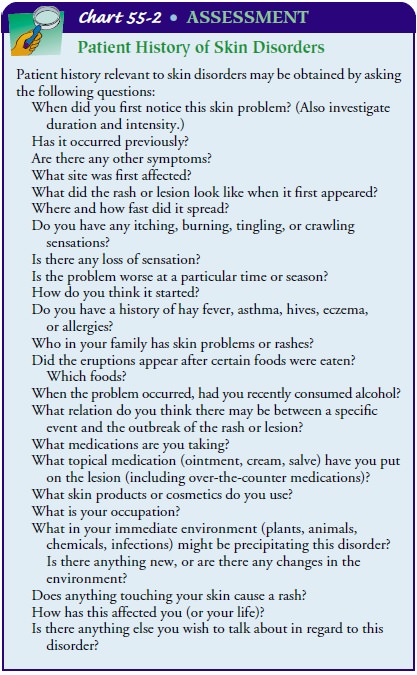
The names of
cosmetics, soaps, shampoos, and other per-sonal hygiene products are obtained
if there have been any recent skin problems noticed with the use of these
products. The health history contains specific information about the onset, signs
and symptoms, location, and duration of any pain, itching, rash, or other
discomfort experienced by the patient. The accompanying as-sessment chart lists
selected questions useful in obtaining appropri-ate information (Chart 55-2).
PHYSICAL ASSESSMENT
Assessment of the skin involves the entire skin area, including the mucous membranes, scalp, hair, and nails. The skin is a reflection of a person’s overall health, and alterations commonly correspond to disease in other organ systems. Inspection and palpation are techniques commonly used in examining the skin. The room must be well lighted and warm. A penlight may be used to highlight lesions. The patient completely disrobes and is adequately draped. Gloves are worn during skin examination if rash or lesions are to be palpated. However, it is important to avoid making the patient feel as if he or she cannot be touched. Touching skin lesions in-dicates a level of acceptance of the patient.
Assessing General Appearance
The
general appearance of the skin is assessed by observing color, temperature,
moisture or dryness, skin texture (rough or smooth), lesions, vascularity,
mobility, and the condition of the hair and nails. Skin turgor, possible edema,
and elasticity are assessed by palpation.
Skin
color varies from person to person and ranges from ivory to deep brown to
almost pure black. The skin of exposed portions of the body, especially in
sunny, warm climates, tends to be more pigmented than the rest of the body. The
vasodilation that occurs with fever, sunburn, and inflammation produces a pink
or reddish hue to the skin. Pallor is an absence of or a decrease in normal
skin color and vascularity and is best observed in the conjunctivae or around
the mouth.
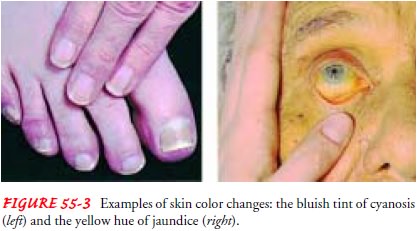
The
bluish hue of cyanosis indicates cellular hypoxia and is easily observed in the
extremities, nail beds, lips, and mucous membranes. Jaundice, a yellowing of
the skin, is directly related to elevations in serum bilirubin and is often
first observed in the sclerae and mucous membranes (Fig. 55-3).
Erythema
Erythema
is redness of the skin
caused by the congestion of cap-illaries. In light-skinned people, it is easily
observed at any loca-tion where it appears. To determine possible inflammation,
the skin is palpated for increased warmth and for smoothness (ie, edema) or
hardness (ie, intracellular infiltration). Because dark skin tends to assume a
purple-gray cast when an inflammatory process is present, it may be difficult
to detect erythema.
Rash
In instances of pruritus (ie, itching), the patient should be asked to indicate which areas of the body are involved. The skin is then stretched gently to decrease the reddish tone and make the rash stand out. Pointing a penlight laterally across the skin may ef-fectively highlight the rash. The differences in skin texture are then assessed by running the tips of the fingers lightly over the skin. The borders of the rash may be palpable. The patient’s mouth and ears are included in the examination. (Sometimes rubeola, or measles, causes a red cast to appear on the tip of the ears.) The patient’s temperature is assessed, and the lymph nodes are palpated.
Cyanosis
Cyanosis
is the bluish discoloration that results from a lack of oxygen in the blood. It
appears with shock or with respiratory or circulatory compromise. In people
with light skin, cyanosis man-ifests as a bluish hue to the lips, fingertips,
and nail beds. Other indications of decreased tissue perfusion include cold,
clammy skin; a rapid, thready pulse; and rapid, shallow respirations. The
conjunctivae of the eyelids are examined for pallor and petechiae (ie, pinpoint red spots that appear on the skin as a
result of blood leakage into the skin).
In
a person with dark skin, the skin usually assumes a grayish cast. To detect
cyanosis, the areas around the mouth and lips and over the cheekbones and
earlobes should be observed.
Color Changes
Almost
every process that occurs on the skin causes some color change. For example, hypopigmentation (ie, decrease in the
melanin of the skin, resulting in a loss of pigmentation) may be caused by a
fungal infection, eczema, or vitiligo
(ie, condition characterized by destruction of the melanocytes in
circum-scribed areas of the skin, resulting in white patches). Hyper-pigmentation (ie, increase in the
melanin of the skin, resultingin increased pigmentation) may occur after
disease or injury to the skin (ie, postinflammatory), after sun injury, or as a
result of aging.
Changes
in skin color in people with dark skin are more no-ticeable and may cause more
concern because the discoloration is more readily visible. Some variation in
skin pigment levels is con-sidered normal. Examples include the pigmented
crease across the bridge of the nose, pigmented streaks in the nails, and
pigmented spots on the sclera of the eye. Many variations of color are
genet-ically determined.
ASSESSING PATIENTS WITH DARK SKIN
The
color gradations that occur in people with dark skin are largely determined by
genetic transmission; they may be described as light, medium, or dark. In
people with dark skin, melanin is produced at a faster rate and in larger
quantities than in people with light skin. Healthy dark skin has a reddish base
or under-tone. The buccal mucosa, tongue, lips, and nails normally are pink.
The degree of pigmentation of the patient’s skin may affect the appearance of a
lesion. Lesions may be black, purple, or gray instead of the tan or red seen in
patients with light skin. Dark pig-ment responds with discoloration after
injury or inflammation, and patients with dark skin more often experience
post-inflammatory hyperpigmentation than those with lighter skin. The
hyperpigmentation eventually fades but may require months to a year to do so.
In
general, people with dark skin suffer the same skin condi-tions as those with
light skin. They are less likely to have skin can-cer but more likely to have
keloid or scar formation and disorders resulting from occlusion or blockage of
hair follicles.
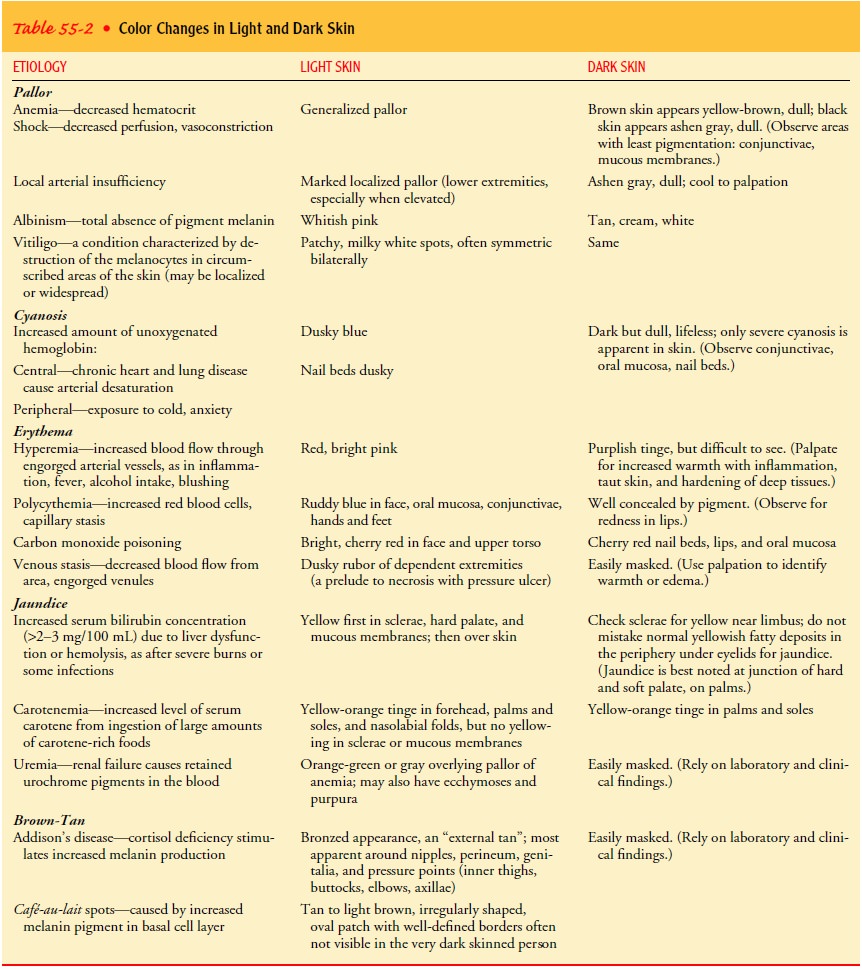
Table
55-2 provides an overview of color changes in light-skinned and dark-skinned
people, and the following section pro-vides specific guidelines for assessing
dark and light skin.
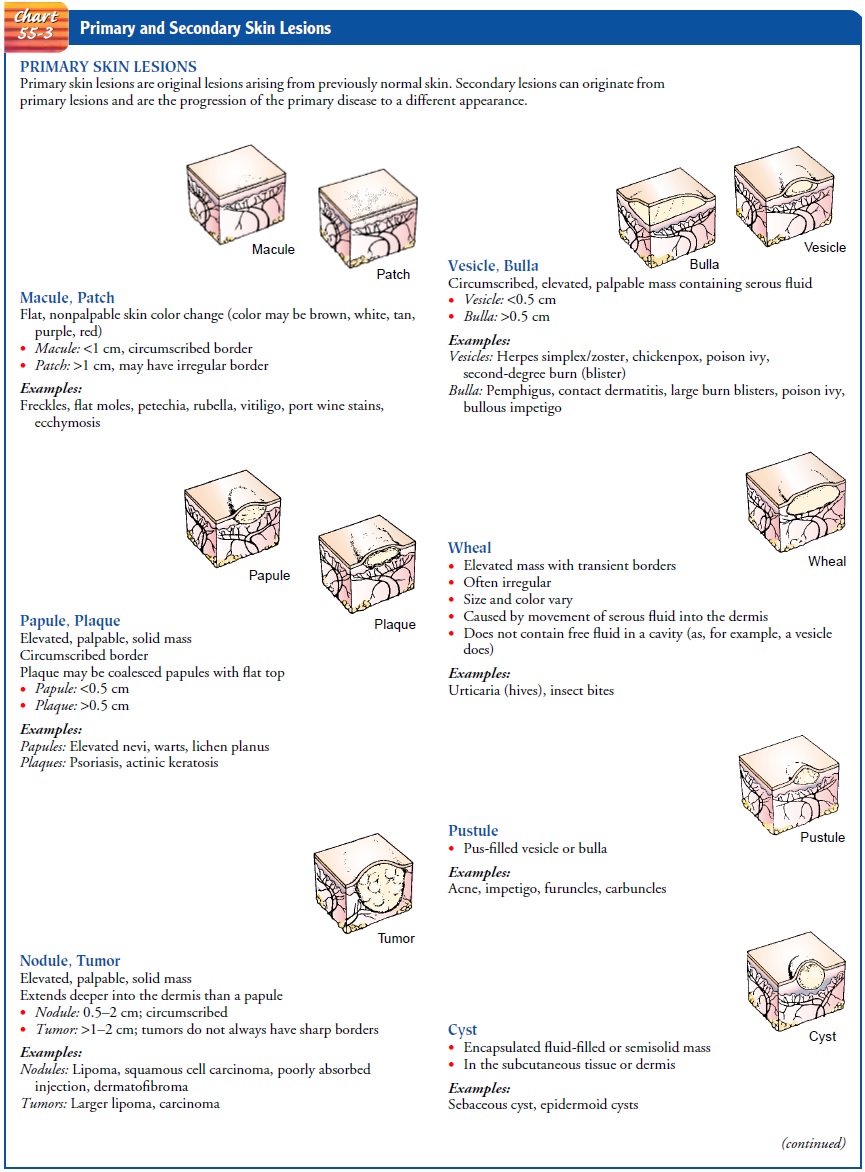
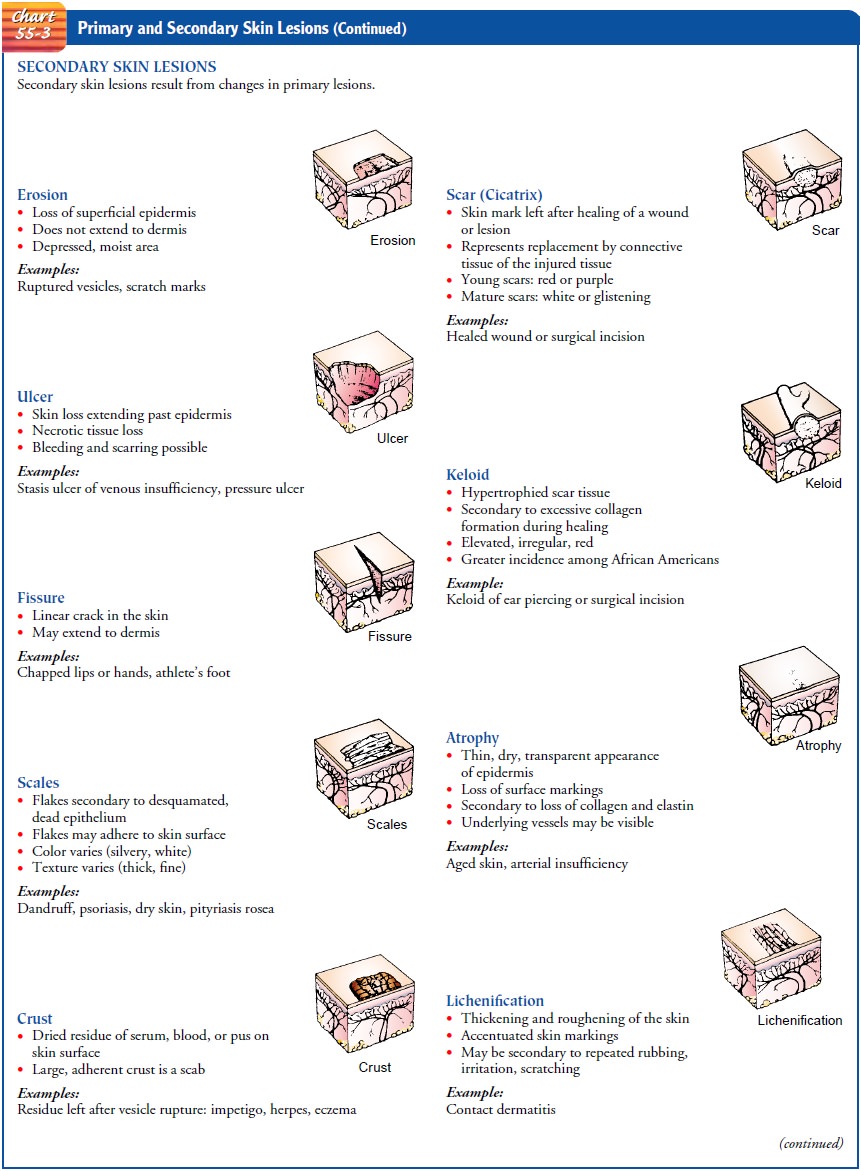
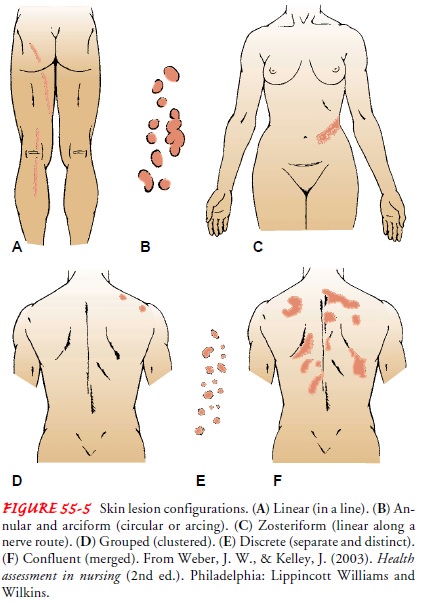
ASSESSING SKIN LESIONS
Skin lesions are the most prominent characteristics
of dermato-logic conditions. They vary in size, shape, and cause and are
clas-sified according to their appearance and origin. Skin lesions canbe
described as primary or secondary. Primary lesions are the ini-tial lesions and
are characteristic of the disease itself. Secondary lesions result from
external causes, such as scratching, trauma, in-fections, or changes caused by
wound healing. Depending on the stage of development, skin lesions are further
categorized accord-ing to type and appearance (Chart 55-3).
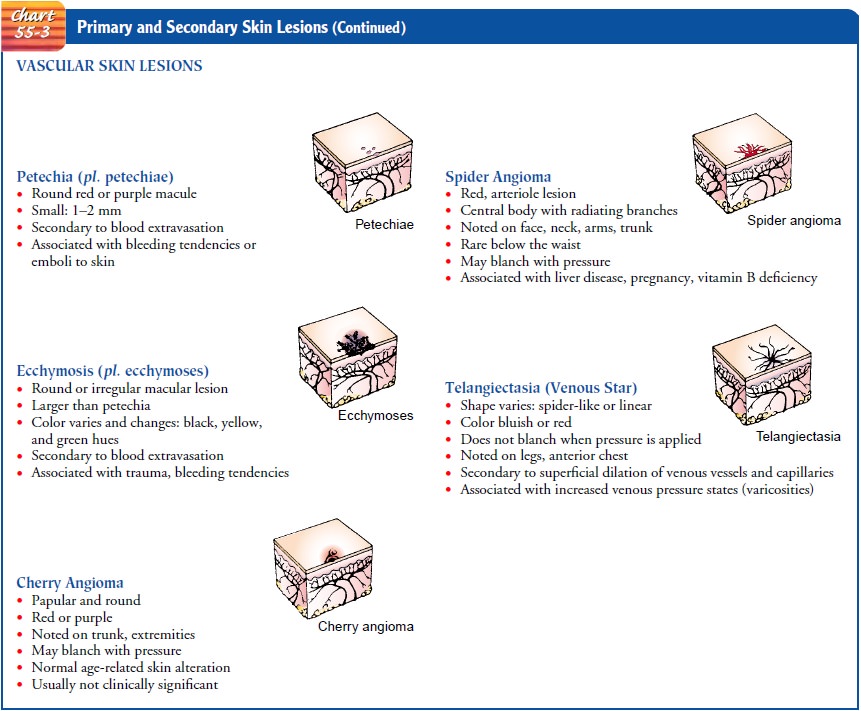
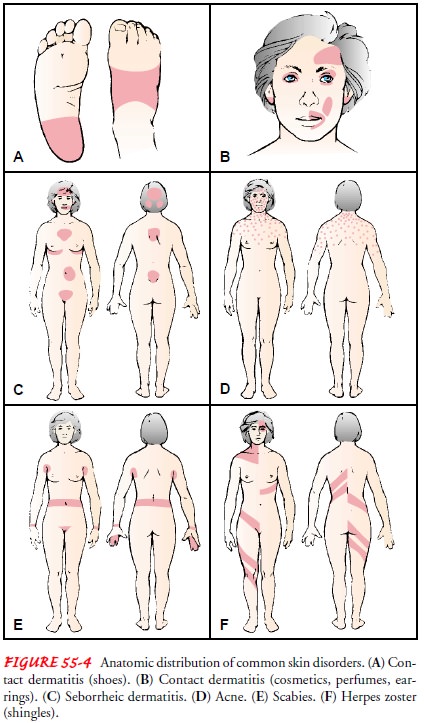
A preliminary assessment of the eruption or lesion
should help to identify the type of dermatosis
(ie, abnormal skin condition) and indicate whether the lesion is primary or
secondary. At the same time, the anatomic distribution of the eruption should
be ob-served, because certain diseases affect certain sites of the body and are
distributed in characteristic patterns and shapes (Figs. 55-4 and 55-5). To
determine the extent of the regional distribution, the left and right sides of
the body should be compared while the color and shape of the lesions are
assessed. After observation, the lesions are palpated to determine their
texture, shape, and border and to see if they are soft and filled with fluid or
hard and fixed to the surrounding tissue.
A
metric ruler is used to measure the size of the lesions so that any further
extension can be compared with this baseline mea-surement. The dermatosis is
documented on the patient’s health record; it should be described clearly and
in detail, using precise terminology.
After
the characteristic distribution of the lesions has been de-termined, the
following information should be obtained and described clearly and in detail:
·
Color of the lesion
·
Any redness, heat, pain, or
swelling
·
Size and location of the
involved area
·
Pattern of eruption (eg,
macular, papular, scaling, oozing, discrete, confluent)
·
Distribution of the lesion
(eg, bilateral, symmetric, linear, circular)
If
acute open wounds or lesions are found on inspection of the skin, a
comprehensive assessment should be made and docu-mented in the patient’s
record. This assessment should address several issues:
·
Wound bed: Inspect for
necrotic and granulation tissue, epithelium, exudate, color, and odor.
·
Wound edges and margins:
Observe for undermining (ie, extension of the wound under the surface skin),
and evalu-ate for condition.
·
Wound size: Measure in
millimeters or centimeters, as ap-propriate, to determine diameter and depth of
the wound and surrounding erythema.
·
Surrounding skin: Assess for
color, suppleness and mois-ture, irritation, and scaling.
Assessing Vascularity and Hydration
After
the color of the skin has been evaluated and lesions have been inspected, an
assessment of vascular changes in the skin is performed. A description of
vascular changes includes location, distribution, color, size, and the presence
of pulsations. Common vascular changes include petechiae, ecchymoses, telangiectases (ie, red marks on the
skin caused by stretching of the superficial blood vessels), angiomas, and
venous stars.
Skin moisture, temperature, and texture are assessed primar-ily by palpation. The elasticity (ie, turgor) of the skin, which de-creases in normal aging, may be a factor in assessing the hydration status of a patient.
Assessing the Nails and Hair
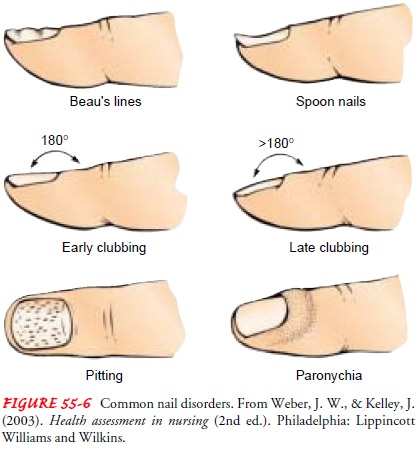
A brief inspection of the nails includes observation of configura-tion, color, and consistency. Many alterations in the nail or nail bed reflect local or systemic abnormalities in progress or resulting from past events (Fig. 55-6). Transverse depressions known as Beau’s lines in the nails may reflect retarded growth of the nail matrix because of severe illness or, more commonly, local trauma. Ridging, hypertrophy, and other changes may also be visible with local trauma. Paronychia, an inflammation of the skin around the nail, is usually accompanied by tenderness and erythema. The angle between the normal nail and its base is 160 degrees. When palpated, the nail base is usually firm. Clubbing is manifested by a straightening of the normal angle (180 degrees or greater) and softening of the nail base. The softened area feels spongelike when palpated.
The hair assessment is carried out by inspecting
and palpating. Gloves are worn, and the examination room should be well
lighted. Separating the hair so that the condition of the skin underneath can
be easily seen, the nurse assesses color, texture, and distribu-tion. Any
abnormal lesions, evidence of itching, inflammation, scaling, or signs of
infestation (ie, lice or mites) are documented.
COLOR AND TEXTURE
Natural
hair color ranges from white to black. Hair color begins to gray with age,
initially appearing during the third decade of life, when the loss of melanin begins
to become apparent. However, it is not unusual for the hair of younger people
to turn gray as a re-sult of hereditary traits. The person with albinism (ie,
partial or complete absence of pigmentation) has a genetic predisposition to
white hair from birth. The natural state of the hair can be altered by using
hair dyes, bleaches, and curling or relaxing products. The types of products
used are identified during the assessment.
The
texture of scalp hair ranges from fine to coarse, silky to brittle, oily to
dry, and shiny to dull, and hair can be straight, curly, or kinky. Dry, brittle
hair may result from overuse of hair dyes, hair dryers, and curling irons or
from endocrine disorders, such as thyroid dysfunction. Oily hair is usually
caused by in-creased secretion from the sebaceous glands close to the scalp. If
the patient reports a recent change in hair texture, the underlying reason is
pursued; the alteration may arise simply from the over-use of commercial hair
products or from changing to a new shampoo.
DISTRIBUTION
Body
hair distribution varies with location. Hair over most of the body is fine,
except in the axillae and pubic areas, where it is coarse. Pubic hair, which
develops at puberty, forms a diamond shape extending up to the umbilicus in boys
and men. Female pubic hair resembles an inverted triangle. If the pattern found
is more characteristic of the opposite gender, it may indicate an en-docrine
problem and further investigation is in order. Racial dif-ferences in hair are
expected, such as straight hair in Asians and curly, coarser hair in people of
African descent.
Men tend to have more body and facial hair than women. Loss of hair, or alopecia, can occur over the entire body or be confined to a specific area. Scalp hair loss may be localized to patchy areas or may range from generalized thinning to total baldness.
When assessing scalp hair loss, it is important to in-vestigate the underlying
cause with the patient. Patchy hair loss may be from habitual hair pulling or
twisting; from excessive traction on the hair (eg, braiding too tightly);
excessive use of dyes, straighteners, and oils; chemotherapeutic agents (eg,
doxo-rubicin, cyclophosphamide); fungal infection; or moles or lesions on the
scalp. Regrowth may be erratic, and distribution may never attain the previous
thickness.
HAIR LOSS
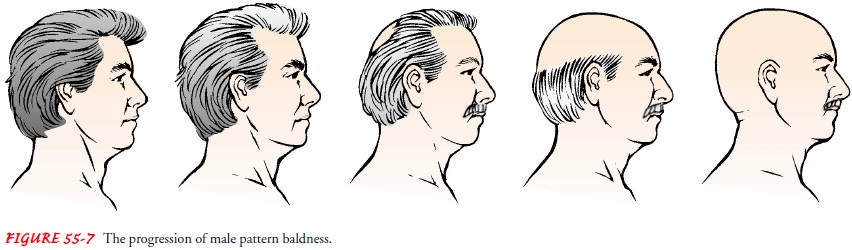
The
most common cause of hair loss is male pattern baldness, which affects more
than one half of the male population and is believed to be related to heredity,
aging, and androgen (male hormone) levels. Androgen is necessary for male
pattern bald-ness to develop. The pattern of hair loss begins with receding of
the hairline in the frontal-temporal area and progresses to gradual thinning
and complete loss of hair over the top of the scalp and crown. Figure 55-7
illustrates the typical male pattern hair loss.
OTHER CHANGES
Male
pattern hair distribution may be seen in some women at the time of menopause,
when the hormone estrogen is no longer pro-duced by the ovaries. In women with
hirsutism, excessive hair may grow on the face, chest, shoulders, and pubic
area. When menopause is ruled out as the underlying cause, hormonal
ab-normalities related to pituitary or adrenal dysfunction must be
investigated.
Because
patients with skin conditions may be viewed nega-tively by others, these
patients may become distraught and avoid interaction with people. Skin
conditions can lead to disfigure-ment, isolation, job loss, and economic
hardship.
Some conditions may subject the patient to a
protracted illness, leading to feelings of depression, frustration,
self-consciousness, poor self-image, and rejection. Itching and skin
irritation, fea-tures of many skin diseases, may be a constant annoyance. The
results of these discomforts may be loss of sleep, anxiety, and de-pression,
all of which reinforce the general distress and fatigue that frequently
accompany skin disorders.
For patients suffering such physical and psychological
dis-comforts, the nurse needs to provide understanding, explanations of the
problem, appropriate instructions related to treatment, nursing support,
patience, and encouragement. It takes time to help patients gain insight into
their problems and resolve their difficulties. It is imperative to overcome any
aversion that may be felt when caring for patients with unattractive skin
disorders. The nurse should show no sign of hesitancy when approaching
pa-tients with skin disorders. Such hesitancy only reinforces the
psy-chological trauma of the disorder.
Related Topics