Chapter: Medical Surgical Nursing: Assessment of Integumentary Function
Anatomy of the Skin, Hair, Nails, and Glands of the Skin
Anatomic and Physiologic
Overview
The largest organ system of the body, the skin is
indispensable for human life. Skin forms a barrier between the internal organs
and the external environment and participates in many vital body func-tions.
The skin is contiguous with the mucous membrane at the ex-ternal openings of
the digestive, respiratory, and urogenital systems. Because skin disorders are
readily visible, dermatologic complaints are commonly the primary reason for a
patient to seek health care.
ANATOMY OF THE SKIN, HAIR, NAILS, AND GLANDS OF THE SKIN
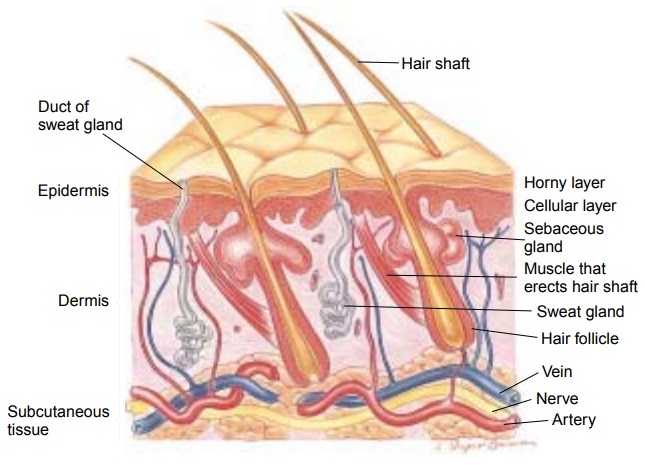
The
skin is composed of three layers: epidermis, dermis, and sub-cutaneous tissue
(Fig. 55-1). The epidermis is an outermost layer of stratified epithelial cells
and composed predominantly of kera-tinocytes. It ranges in thickness from about
0.1 mm on the eye-lids to about 1 mm on the palms of the hands and soles of the
feet. Four distinct layers compose the epidermis, from innermost to outermost:
stratum germinativum, stratum granulosum, stra-tum lucidum, and stratum
corneum. Each layer becomes more differentiated (ie, mature and with more
specific functions) as it rises from the basal stratum germinativum layer to
the outermost stratum corneum layer.
Epidermis
The epidermis, which is contiguous with the mucous
membranes and the lining of the ear canals, consists of live, continuously
di-viding cells covered on the surface by dead cells that were originally
deeper in the dermis but were pushed upward by the newly developing, more
differentiated cells underneath. This external layer is almost completely
replaced every 3 to 4 weeks. The dead cells contain large amounts of keratin, an insoluble, fibrous pro-tein
that forms the outer barrier of the skin and has the capacity to repel
pathogens and prevent excessive fluid loss from the body. Keratin is the
principal hardening ingredient of the hair and nails.
Melanocytes
are the special cells of
the epidermis that are pri-marily involved in producing the pigment melanin, which col-ors the skin and
hair. The more melanin in the tissue, the darker is the color. Most of the skin
of dark-skinned people and the darker areas of the skin on light-skinned people
(eg, the nipple) contain larger amounts of this pigment. Normal skin color
de-pends on race and varies from pale; almost ivory, to deep brown, almost pure
black. Systemic disease affects skin color as well. For example, the skin
appears bluish when there is insufficient oxy-genation of the blood,
yellow-green in people with jaundice, or red or flushed when there is
inflammation or fever (Table 55-1).
Production
of melanin is controlled by a hormone secreted from the hypothalamus of the
brain called melanocyte-stimulatinghormone.
It is believed that melanin can absorb ultraviolet lightin sunlight.
Two
other cells are common to the epidermis: Merkel and Langerhans cells. Merkel cells are receptors that
transmit stimuli to the axon through a chemical synapse. Langerhans cells are
be-lieved to play a significant role in cutaneous immune system re-actions.
These accessory cells of the afferent immune system process invading antigens
and transport the antigens to the lymph system to activate the T lymphocytes.
The
epidermis is modified in different areas of the body. It is thickest over the
palms of the hands and soles of the feet and con-tains increased amounts of
keratin. The thickness of the epider-mis can increase with use and can result
in calluses forming on the hands or corns forming on the feet.
The junction of the epidermis and dermis is an area of many undulations and furrows called rete ridges. This junction an-chors the epidermis to the dermis and permits the free exchange of essential nutrients between the two layers. This interlocking between the dermis and epidermis produces ripples on the sur-face of the skin. On the fingertips, these ripples are called finger-prints. They are a person’s most individual characteristic, andthey rarely change
Dermis
The dermis makes up the largest portion of the
skin, providing strength and structure. It is composed of two layers: papillary
and reticular. The papillary dermis lies directly beneath the epidermis and is
composed primarily of fibroblast cells capable of produc-ing one form of
collagen, a component of connective tissue. The reticular layer lies beneath
the papillary layer and also produces collagen and elastic bundles. The dermis
is also made up of blood and lymph vessels, nerves, sweat and sebaceous glands,
and hair roots. The dermis is often referred to as the “true skin.”
Subcutaneous Tissue
The
subcutaneous tissue, or hypodermis, is the innermost layer of the skin. It is
primarily adipose tissue, which provides a cush-ion between the skin layers,
muscles, and bones. It promotes skin mobility, molds body contours, and
insulates the body. Fat is de-posited and distributed according to the person’s
gender and in part accounts for the difference in body shape between men and
women. Overeating results in increased deposition of fat beneath the skin. The
subcutaneous tissues and amount of fat deposited are important factors in body
temperature regulation.
Hair
An outgrowth of the skin, hair is present over the
entire body ex-cept for the palms and soles. The hair consists of a root formed
in the dermis and a hair shaft that projects beyond the skin. It grows in a
cavity called a hair follicle.
Proliferation of cells in the bulb of the hair causes the hair to form (see
Fig. 55-1).
Hair follicles undergo cycles of growth and rest.
The rate of growth varies; beard growth is the most rapid, followed by hair on
the scalp, axillae, thighs, and eyebrows. The growth or anagenphase may last up to 6 years for scalp hair, whereas the
telogen orresting phase lasts for approximately 4 months. During telogen, hair
sheds from the body. The hair follicle recycles into the grow-ing phase
spontaneously, or it can be induced by plucking out hairs. Growing and resting
hair can be found side by side on all parts of the body. About 90% of the
100,000 hair follicles on a normal scalp are in the
growing phase at any one time, and 50 to 100 scalp hairs are shed each day.
There
is a small bulge on the side of the hair follicle that houses the stem cells
that migrate down to the follicle root and begin the cycle of reproducing the
hair shaft. It was discovered that these bulges also contain the stem cells
that migrate upward to reproduce skin (Jaworski & Gilliam, 1999). The
location of these cells on the side of the hair shaft rather than at the base
is a fac-tor in hair loss. In conditions in which inflammation causes dam-age
to the root of the hair, regrowth is possible. However, if inflammation causes
damage to the bulge on the side, stem cells are destroyed and hair does not
grow.
In
certain locations on the body, hair growth is controlled by sex hormones. The
most vivid example is the growth of hair on the face (ie, beard and mustache),
chest, and back, which is con-trolled by the male hormones known as androgens.
Some women with higher levels of testosterone have hair in the areas generally
thought of as masculine, such as the face, chest, and lower ab-domen. This is
often a normal genetic variation; if it appears along with irregular menses and
weight changes it may indicate a hormonal imbalance.
Hair
in different parts of the body serves different functions. The hairs of the
eyes (ie, eyebrows and lashes), nose, and ears filter out dust, bugs, and
airborne debris. The hair of the skin provides thermal insulation in lower
animals. This function is en-hanced during cold or fright by piloerection (ie,
hairs standing on end), caused by contraction of the tiny erector muscles
attached to the hair follicle. The piloerector response that occurs in humans
is probably vestigial (ie, rudimentary).
Hair
color is supplied by various amounts of melanin within the hair shaft. Gray or
white hair reflects the loss of pigment. Hair quantity and distribution can be
affected by endocrine conditions. For example, Cushing’s syndrome causes hirsutism (ie, excessive hair growth,
especially in women), and hypothyroid-ism (ie, underactive thyroid) causes
changes in hair texture. In many cases, chemotherapy and radiation therapy
cause hair thin-ning or weakening of the hair shaft, resulting in partial or
com-plete alopecia (ie, hair loss)
from the scalp and other parts of the body.
Nails
On
the dorsal surface of the fingers and toes, a hard, transparent plate of
keratin, called the nail, overlies
the skin. The nail grows from its root, which lies under a thin fold of skin
called the cuti-cle. The nail protects the fingers and toes by preserving their
highly developed sensory functions, such as for picking up small objects.
Nail
growth is continuous throughout life, with an average growth of 0.1 mm daily.
Growth is faster in fingernails than toe-nails and tends to slow with aging.
Complete renewal of a fin-gernail takes about 170 days, whereas toenail renewal
takes 12 to 18 months.
Glands of the Skin
There are two types of skin glands: sebaceous
glands and sweat glands (see Fig. 55-1). The sebaceous glands are associated with hair follicles. The ducts of
the sebaceous glands empty sebum
(ie, oily secretion) onto the space between the hair follicle and the hair
shaft. For each hair there is a sebaceous gland, the secretions of which
lubricate the hair and render the skin soft and pliable.
Sweat glands are found in the skin over most of the
body sur-face. They are heavily concentrated in the palms of the hands and
soles of the feet. Only the glans penis, the margins of the lips, the external
ear, and the nail bed are devoid of sweat glands. Sweat glands are
subclassified into two categories: eccrine and apocrine.
The
eccrine sweat glands are found in all areas of the skin. Their ducts open
directly onto the skin surface. The thin, watery secretion called sweat is produced in the basal coiled
portion of the eccrine gland and is released into its narrow duct. Sweat is
composed of predominantly water and contains about one half of the salt content
of the blood plasma. Sweat is released from ec-crine glands in response to
elevated ambient temperature and el-evated body temperature. The rate of sweat
secretion is under the control of the sympathetic nervous system. Excessive
sweating of the palms and soles, axillae, forehead, and other areas may occur
in response to pain and stress.
The
apocrine sweat glands are larger, and unlike eccrine glands, their secretion
contains parts of the secretory cells. They are lo-cated in the axillae, anal
region, scrotum, and labia majora. Their ducts generally open onto hair follicles.
The apocrine glands be-come active at puberty. In women, they enlarge and
recede with each menstrual cycle. Apocrine glands produce a milky sweat that is
sometimes broken down by bacteria to produce the characteris-tic underarm odor.
Specialized apocrine glands called ceruminousglands
are found in the external ear, where they produce cerumen(ie, wax).
Related Topics