Chapter: Essentials of Psychiatry: Behavior and Adaptive Functioning
Assessing Behavior and Adaptive Functioning in the Clinical Interview
Assessing Behavior and Adaptive
Functioning in the Clinical Interview
Finding out about a patient’s personality style, level of adaptive functioning and usual patterns of behavior is one of the major tasks of the psychiatric interview. A psychiatrist gains important infor-mation from what a patient and those people close to the patient say about her or his behavior. However, a psychiatrist also gains invaluable information by closely observing the person during the interview itself. Whether the psychiatrist is quickly sizing up an agitated patient during a psychiatric emergency or carefully noticing how a patient shifts in the chair during a psychotherapy session, the ability to observe a patient’s behavior is one of a psy-chiatrist’s most important tools. A patient’s appearance, attitude and motor behaviors during an interaction with the psychiatrist provide important clues to personality, capacity for interpersonal interactions and potentially problematic behavior patterns
Appearance
Observing a patient’s appearance includes making a judgment about the overall physical impression of the person reflected by grooming, clothing, poise and posture. The ability to appear well-kempt is impaired in many psychiatric disorders, ranging from the psychotic patient who appears disheveled after being up for several nights to the depressed patient dressed in dark, som-ber tones and slumped in the chair. Clothing often reveals aspectsof personality; patients with extroverted, histrionic, or dramatic personalities often wear brightly colored, unusual clothes and are often garishly made up. Problems with appearance can suggest the possibility of other functional impairments as well. The mo-tivation and degree of volitional control over appearance must usually be inferred. At times, appearance may provide an impor-tant clue of an inconsistency in a patient’s verbal presentation and suggest a serious behavior problem.
Attitude and Cooperation
The interviewer can also detect a patient’s
attitude and willing-ness to cooperate during an examination. Attitude and
coopera-tion are related but not identical concepts; a paranoid patient may
have a suspicious attitude but may cooperate by answer-ing the interviewer’s
questions nonetheless. Often, however, a person’s attitude and ability to
cooperate are both affected by psychiatric illness. Patients may be friendly or
hostile, seduc-tive, defensive, or apathetic. During the psychiatric interview,
they may seem attentive or disinterested and be frank or eva-sive and guarded.
Again, each of these attitudes and the degree of cooperation a patient exhibits
can depend on the underlying psychiatric state or can reflect a conscious
manipulation on the part of the patient for the sake of achieving a desired
goal. At-titude and degree of cooperativeness with an interviewer yield data
about a patient’s capacity to establish rapport and relate to others, thereby
suggesting the person’s general level of interper-sonal functioning.
Motor Behavior
The astute examiner can also observe motor
behaviors that pro-vide clues to a patient’s internal state. First, the overall
level of ac-tivity should be noted. Behavioral activity is often quantitatively
increased in patients with mania or anxiety disorders, whereas it may be
decreased in those with depression or intoxication. In addition, impulsivity
can sometimes be revealed by motor behav-iors, as when a person pounds on a
wall or hurls an object. Mo-tor behavior can also provide clues to personality;
the dramatic patient often gesticulates freely during conversation, whereas the
obsessive patient often conveys a sense of constricted facial movements and
gestures. The types of behaviors associated with overactivity may include
restlessness, pacing, handwringing, or other forms of agitation. In contrast,
psychomotor retardation is a slowing of the usual body movements. A depressed
patient with psychomotor slowing may be observed sitting perfectly still,
staring into space. Similarly, patients with underlying neurologi-cal disorders
such as Parkinson’s disease or those who are taking medicines that produce
parkinsonism may exhibit motor slowing in the form of lack of facial
expressiveness and loss of the body movements and gestures that often accompany
speech.
Another clinically relevant way of approaching the
task of assessing a patient’s behavior was suggested by Halleck (1994). He
suggested that in addition to focusing on appearance, atti-tude and cooperation
in the clinical evaluation, the interviewer can assess 1) the patient’s
physical and emotional attractiveness; 2) his or her means of seeking control
and whether control is a central issue; and 3) the degree to which the patient
is dependent, passive, aggressive, attention seeking, private, or exploitative
in his or her behaviors. Although patients with different styles have different
motives for and various ways of expressing these types of behaviors, examining
their behavior in each of these catego-ries is likely to provide a productive
additional approach to evalu-ating behavior and adaptive functioning.
Problematic Patterns of Behavior
Problematic patterns of behavior, such as
impulsivity, compulsiv-ity and avoidance, cut across diagnostic groups; looking
for these patterns can be a fruitful way of characterizing aspects of
mal-adaptive functioning. Each of these three patterns can arise from a wide
array of psychiatric problems. For example, intoxicated people are often
disinhibited and impulsive, acting in ways that they would not act if they were
sober. However, a manic patient may also be impulsive, often spending money
freely or engaging in sexual activity without considering the consequences of
these actions. Labeling each of these patterns of behavior impulsive is an
important first step in reaching a diagnosis. In addition, finding one type of
impulsive behavior should prompt the psy-chiatrist to look for others and to
predict that the patient may act impulsively in the future.
Impulsive Behaviors
Impulsive behaviors are actions that arise without
much delay between the formation of an idea or desire and its gratification in
action. Not all impulsive behavior is pathological; in a muted and
well-modulated form, impulsivity is closer to spontaneity. Certain personality
styles, such as dramatic characters, are more likely to be spontaneous or
impulsive than others. In contrast, a person with a conscientious style might
decide to think about the purchase for a few days, then return to buy the
necklace only to find it gone.
However, in its more extreme forms, impulsivity is
often pathological. A number of behaviors that seem dissimilar may have
impulsivity as the common and uniting thread. Another advantage of thinking
about impulsivity as a distinct pattern of
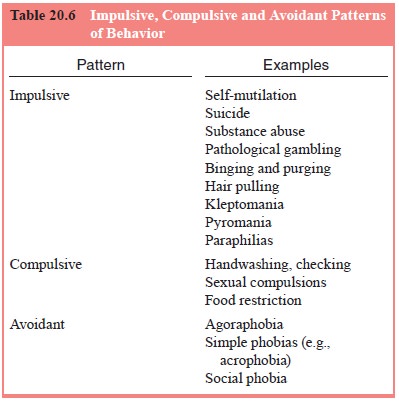
problem behavior is that impulsivity in one sphere
is often ac-companied by impulsive behaviors in other arenas.
Behaviors that are frequently impulsive in nature
include self-mutilation and suicide, substance abuse, pathological gam-bling,
binging and purging eating behaviors, and hair pulling. In addition, urges to
steal (kleptomania), to set fires (pyromania), or to engage in sexually
perverse or unusual behaviors (paraphilias) also result in impulsive behaviors
(Table 20.6).
Different types of impulsive behaviors are often
experi-enced in similar ways by patients. One hallmark of impulsive acts is
that they are often preceded by a growing internal sense of tension and
discomfort that is reduced by the impulsive act itself. Whether the act is hair
pulling (trichotillomania) that results in baldness, or pathological gambling
that has severe financial consequences, the person is likely to feel that she
or he can no longer tolerate the internal tension and that giving in to the
impulse will provide relief to an uncomfortable internal state
A second characteristic of impulsive acts is that
they are often frankly pleasurable at the moment of action even if the per-son
is extremely remorseful afterward
A third hallmark of impulsive behaviors is that
patients are often relatively impervious to the consequences of their ac-tions
at the time and tend to underestimate their chances of being caught
Patients with impulsive patterns of behavior also
tend to underestimate the chances of being caught by a spouse or friend. In
addition, the impulsive nature of the action itself may increase the odds of
apprehension and punishment
Another feature common to impulsive behaviors is
that they often involve a binge, an episode of engaging in a behavior that
seems out of control and cannot be terminated by the patient. Often, the binge
ends only when an external constraint forces the patient to abandon the action.
An eating binge and the relapse of an alcoholic person are often similarly
described: “Once I started eating (drinking) I couldn’t stop. I just kept on
stuffing myself (ordering drinks) until I was too exhausted and sick (drunk and
broke) to continue”.
It is noteworthy that impulsively binging on a
substance such as alcohol sets the stage for further impulsive behaviors secondary
to intoxication.
Compulsive Behaviors
In its muted form, compulsivity can be seen as
careful-ness or attention to detail. It is easy to see how such attention to
detail is helpful in a variety of settings in daily life. Many jobs depend on
thoroughness and a willingness to keep working until the books are balanced to
the last penny. However, compul-sive behaviors become a problem when they begin
to consume much more time than necessary and when they are a response to
nonsensical thoughts (obsessions).
At first glance, compulsive patterns seem to be the oppo-site of impulsive patterns of behavior. In compulsive behaviors, a person repetitively behaves in a stereotyped way. Yet repeated impulsive behaviors can become difficult to distinguish from com-pulsive ones. Is a young female patient who repeatedly gives in to the urge to pull her hair out impulsive or compulsive or both?
In fact, there is evidence that impulsive and
compulsive behaviors tend to cooccur in the same individual. In one study,
impulsive aggression was found to be common in patients with
obsessive–compulsive disorder (Stein and Hollander, 1993). The authors
theorized that obsessive–compulsive disorder and impulsivity may both arise
from a similar problem in the self-regulation of behavior due to a
neuroanatomical lesion in the serotoninergic system. They found that treating
the obses-sive–compulsive disorder with serotonin reuptake inhibitors also
decreased these patients’ impulsive aggression.
The compulsions of obsessive–compulsive disorder, food-restricting behaviors such as those found in anorexia nervosa, and compulsive sexual behavior are common types of compul-sivity (see Table 20.6). Like impulsive behaviors, compulsions share common features and are experienced in similar ways by patients. However, the driving force behind compulsive behav-iors is not the gratification of impulses, but rather the prevention or reduction of anxiety and distress.
The concept that compulsive behavior is an attempt to reduce anxiety is easy to understand when the behavior is a re-sponse to an obsessive thought. However, even when the com-pulsive behavior is sexual in nature, it is driven by the need for anxiety reduction rather than by sexual desire (Coleman, 1992).
Avoidant Behaviors
As with impulsivity and compulsivity, avoidance in
its modulated form can be positive; learning from past negative ex-periences
and avoiding prior mistakes are important capacities.
Avoidant behaviors usually arise from a patient’s history of being fearful or concerned that he or she will become fearful in a given situation. Because of the past history or the perceived threat, the anxiety-provoking situation is avoided. Avoiding the situation means avoiding the fear and anxiety the situation threatens to produce
One study showed that fear and avoidance ratings
were highly correlated both at baseline level and after behavior therapy for
agoraphobia (Cox et al., 1993). In another
study, panic disorder patients with agoraphobia were differentiated from panic
disorder patients without agoraphobia by increased rates of anxiety-relevant
cognitions in the agoraphobic group (Ganellen et al., 1986).
Another feature common to avoidant behaviors is
that they become self-reinforcing and tend to worsen in severity over time if
left untreated.
A further common feature of avoidant behaviors is
their tendency to heighten anticipatory anxiety and precipitate the very
reactions that a person fears.
Related Topics