Chapter: Modern Pharmacology with Clinical Applications: Antiepileptic Drugs
Antiepileptic Drugs
Antiepileptic Drugs
Epilepsy (or epilepsies,
since markedly different clinical entities exist) is a common neurological
abnor-mality affecting about 1% of the human population. Epilepsy is a chronic,
usually life-long disorder charac-terized by recurrent seizures or convulsions
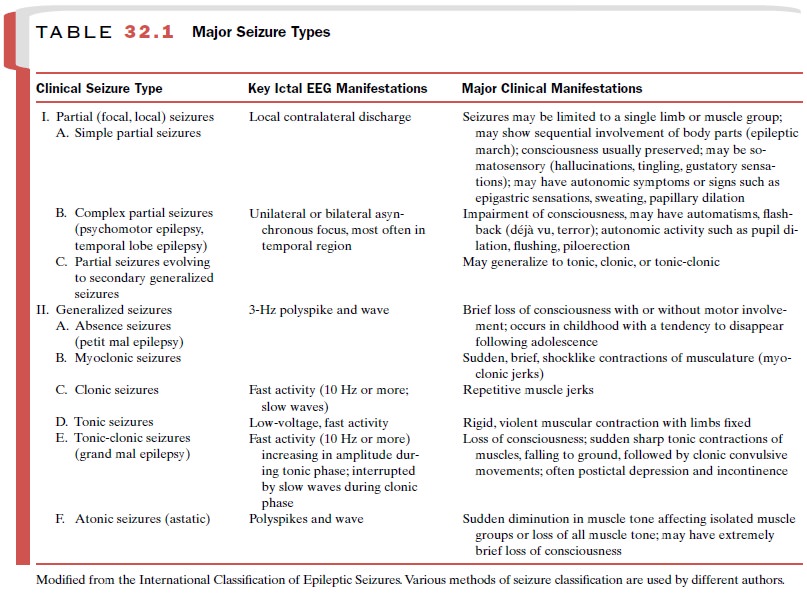
and usually, episodes of unconsciousness and/or amnesia. Table 32.1 illustrates
the major types of epileptic seizures. Patients often exhibit more than one
type. In most instances, the cause of the seizure disorder is not known
(idiopathic epilepsy), although trauma during birth is suspected of being one
cause.
Head trauma, meningitis, childhood fevers, brain tumors, and degenerative diseases of the cerebral circulation are conditions often associated with the appearance of recurrent seizures that may require treatment with anticonvulsant drugs. Seizures also may be a toxic manifestation of the action of central nervous system (CNS) stimulants and certain other drugs. Seizures often occur in hyperthermia (febrile seizures are very common in infants); sometimes in eclampsia, uremia, hypoglycemia, or pyridoxine defi-ciency; and frequently as a part of the abstinence syndrome of individuals physically dependent on CNS depressants.
The therapeutic goal in
epilepsy treatment is com-plete seizure control without excessive side effects.
The prognosis depends in part upon the type of seizure disor-der, but overall,
only about 40 to 60% of patients become totally seizure free with available
drugs. These agents are chemically and pharmacologically diverse, having in
common only their ability to inhibit seizure activity with-out impairing
consciousness. The choice of drug or drugs used depends on seizure
classification, since a particular drug may be more or less specific for a
particular type of seizure; patients having a mixture of seizure types pres-ent
particular therapeutic difficulties. It is not always clear when to treat with
one drug (monotherapy) or more than one drug (polytherapy) in a particular
patient. Approximately 25% of patients given a single anticon-vulsive agent do
not achieve successful seizure control because of an unacceptable level of side
effects. Therefore, two or more drugs may be combined in an at-tempt to provide
better seizure control.
Convulsive disorders often
begin in childhood, and drug therapy must be continued for decades; therefore, any
adverse reaction is especially significant. A knowl-edge of interactions
between anticonvulsants and other drugs is necessary, since the patient usually
must con-tinue anticonvulsant medication regardless of the need for other
drugs. Since it may be dangerous to withdraw anticonvulsant medication from a
pregnant woman with epilepsy, the teratogenic potential of anticonvulsant drugs
also is a consideration in the treatment of women of childbearing age.
The Development of Effective Drug Treatment for Convulsive Disorders
The first effective treatment
of seizure disorders was the serendipitous finding in 1857 that potassium
bromide could control seizures in some patients. Even though side effects were
troublesome, the bromides were widely used for many years. Phenobarbital was
intro-duced as a treatment for epilepsy in 1912 and was im-mediately shown to
be markedly superior to bromides. While other barbiturates were synthesized and
used, none were shown to be superior to phenobarbital, and the latter compound
is still used. A chemically related nonbarbiturate, phenytoin, was discovered
about 20 years later and also remains a valuable drug today. Approaches being
used for the identification of new an-ticonvulsant drugs include the search for
agents that block specific cationic channels in neuronal membranes, agents that
enhance the activity of the inhibitory neuro-transmitter γ-Aminobutyric acid
(GABA), and agents that are capable of inhibiting the activity of the
excita-tory neurotransmitters glutamic and aspartic acids.
Mechanism of Action
In epilepsy certain neurons
and/or groups of neurons become hyperexcitable and begin firing bursts of
action potentials that propagate in a synchronous manner to other brain
structures (and in the case of generalized seizures, to practically all areas
of the brain). These may be the result of abnormalities in neuronal membrane
stability or in the connections among neurons. It is known that the epileptic
bursts consist of sodium-dependent action potentials and a calcium-dependent
depolarizing potential.
Recent drug development
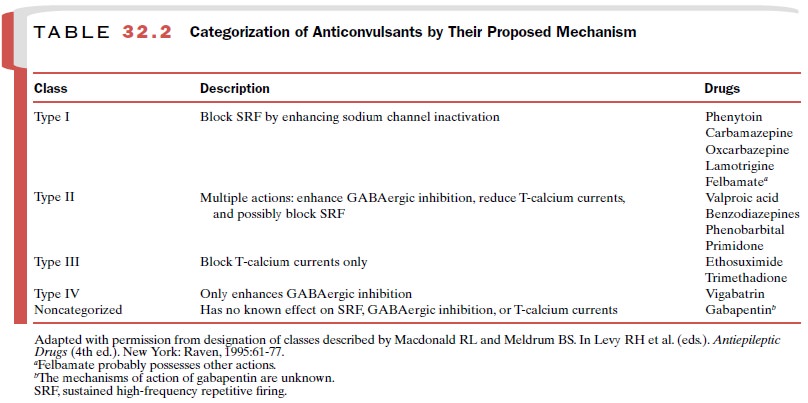
studies have centered on the capacity of known antiepileptic drugs (AEDs) to
in-teract with ion channels, and it is now established that several agents
appear to be exerting their effects prima-rily by inhibiting ion channels.
Modulation of neuronal sodium channels decreases cellular excitability and the
propagation of nerve impulses. Inhibition of sodium channels appears to be a
major component of the mechanism of action of several anticonvulsant drugs.
Much interest is also
centered on the role of calcium channels in neuronal activity, since the
depolarization associated with burst firing is mediated by the activation of
calcium channels. At therapeutically relevant con-centrations, the antiabsence
drug ethosuximide appears to exert its effect by inhibiting the T-type calcium
chan-nels. A portion of valproic acid’s activity may also be at-tributable to
this effect.
Disinhibition may play an
important role in the generation of epileptic seizures, since a reduction of
GABAergic inhibition is necessary to produce the synchronous burst discharges
in groups of cells. Com-pounds that antagonize the activity of GABA
(picro-toxinin, penicillin C, bicuculline) are CNS convulsants, while agents
that facilitate GABA’s inhibition have an-ticonvulsant activity. Several
anticonvulsant drugs act to facilitate the actions of GABA.
Excitatory neurotransmitters
also may be involved in the appearance of epilepsy, since the bursting activity
typically seen during epileptic discharges may be due in part to the action of
glutamate acting on N-methyl-D-aspartate (NMDA) receptor
channels to produce depo-larization. It is likely that a major part of the anticon-vulsant
activity of felbamate involves blockade of the NMDA receptor. Table 32.2
summarizes the most likely mechanism of action associated with available
anticon-vulsant drugs.
Related Topics