Chapter: Modern Medical Toxicology: Hydrocarbons and Pesticides: Hydrocarbon
Aliphatic Hydrocarbons
ALIPHATIC HYDROCARBONS
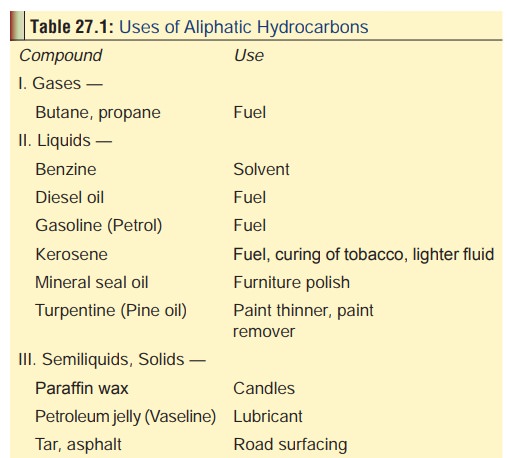
Uses
Listed
in Table 27.1.
Mode of Action
■■ Ingestion of
aliphatic hydocarbons with high molecular weight such as paraffin wax,
vaseline, grease, etc. is associated with little or no toxicity.
■■ Liquid hydrocarbons
are the most toxic, but symptoms gener-ally are the result of aspiration into
the airways rather than absorption from the GI tract.
■■ The aspiration
potential of a hydrocarbon depends on properties—viscocity, surface tension, and volatility.
Viscocity is the tendency of a
substance to resist flow (“the ability to resist stirring”) which is measured
in Saybolt Seconds Universal (SSU). The lower the viscocity (i.e. below 60
SSU), the higher the tendency for aspira-tion. Surface tension refers to the adherence of a liquid compound along
its surface (“the ability to creep”). It is the result of cohesive forces
generated by the attraction between molecules (van der Waals forces). The lower
the surface tension, the higher the tendency for aspira-tion. Volatility refers to the ability of a
liquid to become a gas. The higher the volatility, the higher the tendency for
aspiration.
■■ Aliphatic hydrocarbons possessing high
aspiration potentialinclude gasoline, kerosene, mineral seal oil, and
turpentine.
Clinical Features
RS: Respiratory distress from
aspiration usually begins within 30 minutes of exposure, and is manifested
mainly by gasping, coughing, and choking. There are 3 grades:
·
Mild : coughing, choking, tachypnoea,
drowsiness,rales, rhonchi.
·
Moderate : grunting, lethargy, flaccidity,
bronchospasm.
·
Severe : cyanosis, coma, seizures.
Moderate fever is often present but does not correlate with severity. Haemoptysis and pulmonary oedema may occur after significant aspiration or inhalation.
CNS:
Lethargy with depressed sensorium. Coma and convulsions are rare. Aniline,
heavy metals, camphor, pesti-cides and other additives or contaminants in
hydrocarbon preparations may produce additional CNS toxicity. For instance,
chronic cerebellar degeneration may be associated with lead additives of gasoline.
GIT:
Burning of mouth, sore throat, nausea, and vomiting. Haematemesis may occur.
Diarrhoea is rare.
CVS:
Arrhythmias are seen in solvent abuse, but are rare in ingestions.
Skin:
Acute exposure can cause dermatitis, and if this is prolonged it may result in
full thickness burns. Chronic exposure to kerosene can cause severe acne.
Contact with liquefied petroleum gases (e.g. propane, butane, propylene,
isobutane, butenes, n-butane), ethane, etc. can result in frostbite or effects
resembling frostbite.
Haematologic:
Disseminated intravascular coagulation, haemolytic anaemia and pancytopenia
have occasionally been reported following vapour inhalation, aspiration, or
ingestion of hydrocarbons.
Other
effects:
·
Elevated liver enzyme levels and hepatosplenomegaly can
occur with petroleum distillate ingestion.
·
Renal effects (acute renal tubular
necrosis, proteinuria, or haematuria) occur infrequently following acute
expo-sure to petroleum distillates and other unsubstituted hydrocarbons.
·
Straight chain hydrocarbons with few
carbon atoms (e.g. methane, ethane, propane gases) can cause asphyxiation if
exposure occurs in poorly ventilated spaces.
·
Injection of kerosene, naphtha, turpentine, gasoline, or
hydrocarbon insecticides has resulted in febrile reac-tions, local tissue
inflammation and systemic effects, including pulmonary oedema, pneumonia and
mild CNS depression. Injection of pressurised hydrocarbons has caused severe
tissue damage. Subcutaneous injec-tion of paint, lacquer or other material via
high pres-sure spray guns is a surgical emergency. High-pressure injection
injuries can result in necrosis and thrombosis with amputation required in 60
to 80% of cases.![]()
·
Exposure to hydrocarbons may result
in the loss of colour vision, with the risk of impaired colour vision
increasing with increasing exposure.
·
Poisoning due to inhalation of
butane and other similar gaseous hydrocarbons is dealt with under “Glue
sniffing”.
Diagnosis
·
X-Ray—Changes may be evident as early as 30 minutes after
exposure and peak at about 72 hours, after which there is gradual resolution.
Common radiologic findings include perihilar densities, bronchovascular
markings, bibasilar infiltrates, and pneumonic consolidation. Early upright
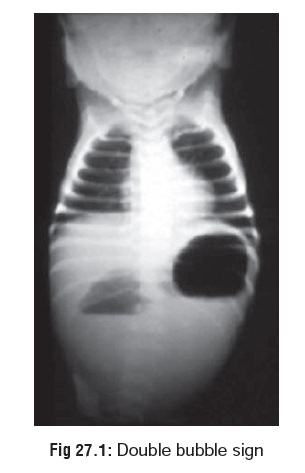
·
X-rays may reveal two liquid densities in the stomach (double bubble sign) (Fig 27.1), which represents two
interfaces: air-hydrocarbon, and hydrocarbon-fluid, since hydrocarbons are not
miscible with water and are usually lighter. Two important points are to be
noted in connection with radiographic changes in hydrocarbon ingestion—
o They correlate poorly with clinical
symptoms.
o They lag behind clinical
improvement.
·
Arterial blood gases—There is hypoxaemia.
· Blood—Leucocytosis is common during the first 48 hours.
Treatment
·
The following signs and symptoms present upon initial
examination of patients after hydrocarbon ingestion have 80% or better
predictive value for pneumonitis:
o Lethargy, rhonchi, rales,
retractions, cyanosis, and the development of leukocytosis and fever within 4
hours.
o The only parameter with an 80% or
greater predictive value for NO toxicity was the absence of tachypnoea.
o Early chest X-rays were not useful
in predicting pneu-monitis in symptomatic or asymptomatic patients.
·
The immediate concern is the threat of respiratory failure.
A chest X-ray should be taken after stabilisation to confirm or rule out
aspiration. The following measures are necessary if respiration is compromised:
o Endotracheal intubation.
o Oxygen.
o Continuous positive airway pressure
or positive end-expiratory pressure. A recent innovation is high frequency jet
ventilation (HFJV), utilising high respiratory rates (220 to 260) with small
tidal volumes. Extracorporeal membrane oxygenaion (ECMO) is an effective option
in severe pulmonary toxicity when all other meaures have failed.
o Bronchodilators—preferably inhaled
cardioselective drugs such as salbutamol.
·
Decontamination:
o If there is suspicion of dermal
exposure, all clothing should be removed and the skin washed with copious
amounts of soap and water, since significant toxicity can result from cutaneous
absorption.
o Induction of vomiting is not
recommended.
o Stomach wash may be done cautiously
after intuba-tion, especially in those cases where a large quantity of
hydrocarbon has been ingested. However, several investigators are against this
practice and assert that it only enhances the risk of pulmonary toxicity.
o Activated charcoal is generally
considered to be inef-fective in adsorbing petroleum distillates, though there
are experimental studies suggesting the opposite.
·
While prophylactic administration of corticosteroids was
advocated in the past, it is not advocated today, since studies have not
demonstrated any beneficial effects. On the other hand it can increase the chances
of bacterial superinfection.
·
Similarly, prophylactic administration of antibiotics which
was the norm in the past is also discouraged today, since it can alter the
bacterial flora and lead to subsequent infection by resistant gram-negative
bacteria. Pulmonary cultures should be done to decide on antibiotic
adminis-tration, though this may not be practicable in critically ill patients.
In such cases, prophylactic antibiotic therapy may be justified.
·
Crystalloid solutions must be administered judiciously.
Pulmonary artery monitoring may help. In general, the pulmonary artery wedge
pressure should be kept relatively low while still maintaining adequate cardiac
output, blood pressure and urine output.
Treatment of frostbite:
Rewarming—
–– Do not institute rewarming unless
complete rewarming can be assured; refreezing thawed tissue increases tissue
damage. Place affected area in a water bath with a temperature of 40 to 420
Celsius for 15 to 30 minutes until thawing is complete. The bath should be
large enough to permit complete immersion of the injured part, avoiding contact
with the sides of the bath. A whirlpool bath would be ideal. Some authors
suggest that an antibacterial (hexachlorophene or povidone-iodine) be added to
the bath water.
–– Correct systemic hypothermia.
––
Rewarming may be associated with increasing pain, requiring narcotic
analgesics.
Wound Care—
––
Digits should be separated by sterile absorbent cotton; no constrictive
dressings should be used. Protective dressings should be changed twice per day.
––
Perform daily hydrotherapy for 30 to 45 minutes in warm water 400
Celsius. This helps debride devital-ised tissue and maintain range of motion.
––
The injured extremities should be elevated and should not be allowed to bear
weight.
–– Clear blisters should be debrided
but haemorrhagic blisters left intact.
–– Further surgical debridement
should be delayed until mummification demarcation has occurred (60 to 90 days).
Spontaneous amputation may occur.
–– Analgesics may be required during
the rewarming phase; however, patients with severe pain should be evaluated for
vasospasm. Arteriography and nonin-vasive vascular techniques (e.g. Doppler
ultrasound, digital plethysmography, isotope scanning), have been useful in
evaluating the extent of vasospasm after thawing.
––
Tetanus prophylaxis as indicated.
–– Topical aloe vera may decrease
tissue destruction and should be applied every 6 hours.
–– Ibuprofen is a thromboxane
inhibitor and may help reduce tissue loss. Adult dose of 200–400 mg every 12 hours
is recommended.
The following treatment
measures/drugs are contraindicated in hydrocarbon poisoning:
·
Emetics
·
Activated charcoal
·
Olive oil/mineral oil
·
Cathartics
Catecholamines (dopamine, adrenaline, noradrenaline, isoproterenol, etc.).
Tar and asphalt can cause
distressing problems of a different sort. These hot hydrocarbon mixtures can
produce severe burns on dermal contact. The material hardens quickly and
becomes extremely difficult to remove. Thermal injury can be minimised by
immediate cooling with cold water. Removal of hardened tar can be attempted
after application of mineral oil, petroleum jelly, or antibac-terial ointment.
Recent reports suggest that surface-acting agents in combination with a
hydrocarbon ointment may be more effective.
Autopsy Features
·
Pulmonary oedema and varying degree
of lung pathology are prominent features.
·
There may also be evidence of
gastrointestinal congestion and (rarely) corrosion.
·
There is often characteristic odour
depending on the type of hydrocarbon ingested.
Forensic Issues
·
Most cases of poisoning result from
accidental exposure. In India, accidental kerosene poisoning is quite common in
the paediatric age group, since it is a popular household fuel and is often
negligently left around in the kitchen in bottles or cans.
·
uncommon because of easy
availability of many of these agents.
·
Experimental animal studies and some
studies on cancer incidence and mortality in human occupational groups suggest
that hydrocarbon exposure is associated with renal neoplasia.
Related Topics