Chapter: Essentials of Psychiatry: Adjustment Disorders
Adjustment Disorders
Adjustment Disorders
Definition
The Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition, Text Revision (DSM-IV-TR) states that the
essential fea-ture of adjustment disorder (AD) is the development of clinically
significant emotional or behavioral symptoms in response to an identifiable
psychosocial stressor (American Psychiatric Associa-tion, 2000). The symptoms
must develop within 3 months after the onset of the stressor (criterion A). The
clinical significance of the reaction is indicated either by marked distress
that is in excess of what would be expected given the nature of the stressor or
by signif-icant impairment in social or occupational (academic) functioning
(criterion B). This disorder should not be used if the emotional and cognitive
disturbances meet the criteria for another specific Axis I disorder (e.g., a
specific anxiety or mood disorder) or are merely an exacerbation of a
preexisting Axis I or Axis II disorder (criterion C). AD may be diagnosed if
other Axis I or II disorders are present, but do not account for the pattern of
symptoms that have occurred in response to the stressor. The diagnosis of AD
does not apply when the symptoms represent bereavement (criterion D). By
defi-nition, AD must resolve within 6 months of the termination of the stressor
or its consequences (criterion E). However, the symptoms may persist for a
prolonged period (i.e., longer than 6 months) if they occur in response to a
chronic stressor (e.g., a chronic, dis-abling general medical condition) or to
a stressor that has enduring consequences (e.g., the financial and emotional
difficulties result-ing from a divorce) (American Psychiatric Association,
2000).
Although
the above definition provides a certain structure for identifying and
describing AD, there is still uncertainty as to when the impairment in
functioning or the severity of the psychi-atric symptoms that develop in
response to a stressor are suffi-cient to warrant a diagnosis of AD. The
DSM-IV-TR describes the boundary issues between conditions that may be a focus
of clini-cal attention (V codes), subthreshold
disorders (NOS disorders) and the specific mental disorders (American
Psychiatric Associa-tion, 2000). A compelling literature documents that there
is much “physical” in mental disorders and much “mental” in physical
dis-orders. No definition adequately specifies precise boundaries for the
concept of a “mental disorder”. “The concept … lacks a con-sistent operational
definition that covers all situations. Whatever its original cause, it must
currently be considered a manifestation of a behavioral, psychological, or biological
dysfunction in the in-dividual”. The issue of defining boundaries is especially
problem-atic in the subthreshold
diagnoses, for example, the AD, in which there are no symptom checklists,
algorithms, or guidelines for the “quantification of attributes”.
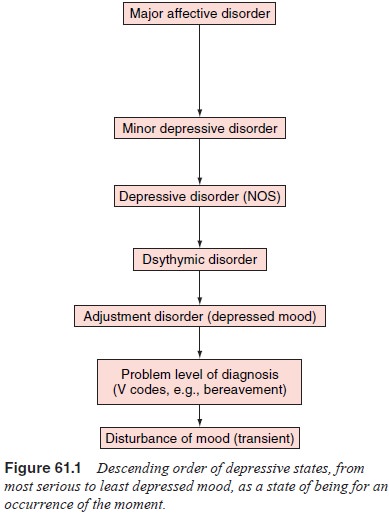
The symptoms of AD are defined in terms of their being a maladaptive response to a psychosocial stressor. There are, in fact, no specific symptoms of AD; any combination of behavioral or emotional symptoms that occur in association with a stressor may qualify. The lack of specific symptoms or quantifiablecriteria of the AD permits the labeling of early or temporary men-tal states when the clinical picture does not meet full evidence for a more specific mental disorder, but the morbid state is more than expected in a normal reaction and treatment or intervention may be indicated. AD are an essential “linchpin” in the psychi-atric–taxonomic spectrum-hierarchy: 1) disorders with specific diagnostic criteria; 2) disorders not otherwise specified (NOS); 3) adjustment disorders; 4) other conditions that may be a focus of clinical attention (V codes) (American Psychiatric Association, 2000); and 5) normal fluctuations of mental states.
Disorders
that do not fulfill the criteria for a specific mental disorder may be accorded
a lesser interest by mental health care workers, research institutes and
third-party payers, even though they present with serious (or incipient)
symptoms that require intervention or treatment. Given this concept, the AD are
formu-lated as a means of classifying psychiatric morbidity that is clini-cally
significant; when the symptom profile is as yet insufficient to meet the more
specifically operationalized criteria for another mental disorder; when the
symptoms, disturbance of mood, and vocational or interpersonal dysfunction are
in excess of a nor-mal reaction to the stressors in question; and for which
treatment is indicated. For example, a diagnosis of AD is not given when the
clinical picture is a psychosocial problem (V code) requiring clinical
attention, such as noncompliance, phase of life problem, bereavement, or
occupational (academic) problem. Their etio-logical and dynamic attributes make
the AD a fascinating group of disorders that serve as a fulcrum between normality
and more specific mental disorders (Figure 61.1).
Attention
to less severe mental symptoms (and psychiatric morbidity) may forestall the
evolution to more serious disorders and allow remediation before relationships,
work and functioning are so impaired that they are disrupted or permanently
sundered
Yet, in
the gray area in which early diagnosis may have enormous value with modest
therapeutic investment, guidelines are the most tenuous. It is the
professionals at the “front door” – primary care physicians, triage personnel,
emergency department staff, walk-in clinic staff – who need assistance in
making this difficult call: Is there sufficient psychiatric morbidity to
warrant mental health intervention?
Because
AD is a nonpejorative psychiatric condition it may have been overdiagnosed in
youths to protect them from feared adversities of major psychiatric
nomenclature. An early study ob-served that 25% of a sample of adolescents with
AD had attempted suicide and that 17% probably “would have met DSM-III criteria
for major depressive disorder” because they had the required symp-toms.
Nevertheless, in psychological autopsy studies of adolescent suicide
completers, approximately 20% do not meet the criteria for any single
psychiatric diagnosis, although they present with significant functional
impairment and life-threatening behavior.
How to
diagnose individuals with suicidal behavior who do not meet criteria for a
specific mental is a challenge. Runeson and colleagues (1996) observed from psychological
autopsy methods that there was a very short median interval between first
suicidal communication and suicide in AD (less than 1 month) compared with
major depressive disorder (3 months), borderline personality disorder (30
months), or schizophrenia (47 months).
Recent
life events, which would constitute an acute stress, were commonly found to
correlate with suicidal behavior in a group that included those with AD
(Isometsa et al., 1996). The
as-sessment of suicidal behavior is an important tool in differentiating major
depressive disorder, dysthymic disorder and AD. Further-more, AD patients
appear to be among the most common recipients of a deliberate self-harm (DSH)
diagnosis, with the majority in-volving self-poisoning. Thus, DSH with all its
variants, e.g., reck-less driving, is more common in AD patients, whereas the
percent-age of completed suicidal behavior per
se was found to be higher in depressed patients (Spalletta et al., 1996). Of note, biological
find-ings in suicidal patients with AD suggest characteristic patterns of
monoamine oxidase (MAO) and noradrenaline turnover. Clearly, what is regarded,
as a subthreshold diagnosis – AD – does not nec-essarily imply the presence of
subthreshold symptomatology.
Related Topics