Chapter: Modern Pharmacology with Clinical Applications: Antianginal Drugs
β-Adrenoceptor Blocking Agents
β-Adrenoceptor Blocking Agents
β-adrenoceptor blockade is a rational approach
to the treatment of angina pectoris, since an increase in sym-pathetic nervous
system activity is a common feature in acute anginal attacks. Based on their
ability to reduce oxygen demand, all β-blockers tested so far have also been
shown to be effective in the treatment of second- ary angina. Administration of
these compounds results in a decrease in frequency of anginal attacks, a
reduc-tion in nitroglycerin consumption, an increased exercise tolerance on the
treadmill, and a decreased magnitude of ST segment depression on the
electrocardiogram during exercise. Propranolol is the prototype of this class
of compounds
β-Blockers approved for
clinical use in secondary angina in the United States include propranolol and
nadolol (Corgard), compounds that
block both β1- and β2-adrenoceptors equally, while atenolol (Tenormin) and metoprolol (Lopressor)
are cardioselective β1β-receptor antagonists.
Mechanism of Action
The myocardial response to
exercise includes an in-crease in heart rate and myocardial contractility.
These effects are mediated in part by the sympathetic nervous system.
Propranolol and other β-adrenoceptor
blockers antagonize the actions of catecholamines on the heart and thereby
attenuate the myocardial response to stress or exercise (Fig. 17.3). The
resting heart rate is reduced by propranolol, but not to the same extent as is
the de-crease in exercise-induced tachycardia. Overall, propra-nolol reduces
myocardial oxygen consumption for a given degree of physical activity.
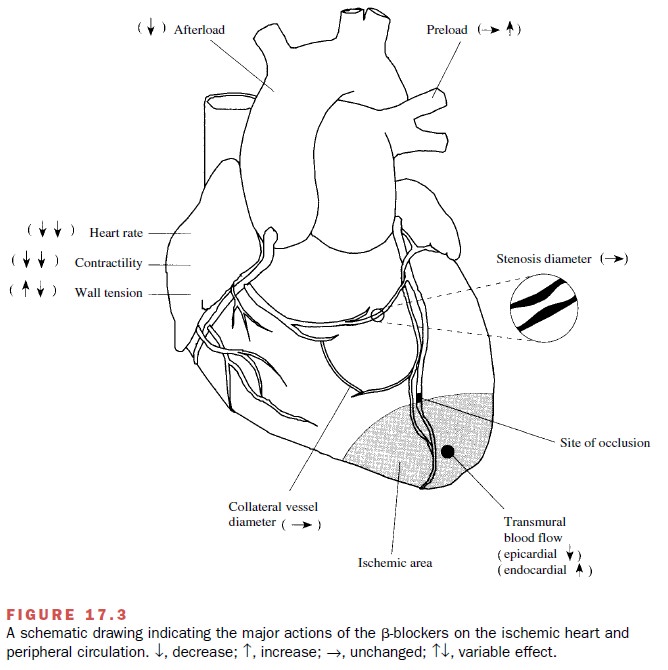
Arterial blood pressure
(afterload) is also reduced by propranolol. Although the mechanisms responsible
for this antihypertensive effect are not completely un-derstood, they are
thought to involve (1) a reduction in cardiac output, (2) a decrease in plasma
renin activity, an action in the central nervous system, and (4) a re-setting
of the baroreceptors . Thus, propranolol may ex-ert a part of its beneficial
effects in secondary angina by decreasing three of the major determinants of
myo-cardial oxygen demand, that is, heart rate, contractility, and systolic
wall tension.
Propranolol and other β-blockers also have been shown to produce an increase in oxygen supply to the subendocardium of ischemic areas. The mechanism re-sponsible for this effect is most likely related to the ability of β-blockers to reduce resting heart rate and in-crease diastolic perfusion time.
Because
subendocardial blood flow and flow distal to severe coronary artery stenosis
occur primarily during diastole, this increase in diastolic perfusion time, due
to the bradycardiac effect of propranolol and other β-blockers, would be
expected to increase subendocardial blood flow to ischemic re-gions. β-blockers
have no significant effect on coronary collateral blood flow. Finally, there is
evidence that - blockers can inhibit platelet aggregation.
Absorption, Metabolism, and Excretion
Propranolol is well absorbed
from the gastrointestinal tract, but it is avidly extracted by the liver as the
drug passes to the systemic circulation (first-pass effect). This effect
explains the large variation in plasma levels of propranolol seen after oral
drug administration.
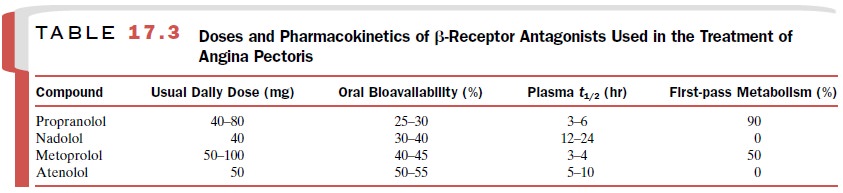
Because of these
interindividual variations in the ki-netics of propranolol, the therapeutic dose
of this drug is best determined by titration. End points of titration include
relief of anginal symptoms, increases in exercise tolerance, and plasma
concentration of propranolol be-tween 15 and 100 ng/mL. For additional details
on the pharmacokinetics of propranolol and other β-receptor antagonists
approved for clinical use in the treatment of angina pectoris, see Table 17.3.
Clinical Uses
By attenuating the cardiac
response to exercise, propra-nolol and other β-blockers increase the amount of
ex-ercise that can be performed before angina develops. Although propranolol
does not change the point of im-balance between oxygen supply and demand at
which angina occurs, it does slow the rate at which the imbal-ance point is reached.
Propranolol is particularly
indicated in the manage-ment of patients whose angina attacks are frequent and
unpredictable despite the use of organic nitrates. Propranolol may be combined
with the use of nitro-glycerin, the latter drug being used to control acute
at-tacks of angina. The combined use of propranolol and organic nitrates
theoretically should enhance the thera-peutic effects of each and minimize
their adverse effects (Table 17.4).
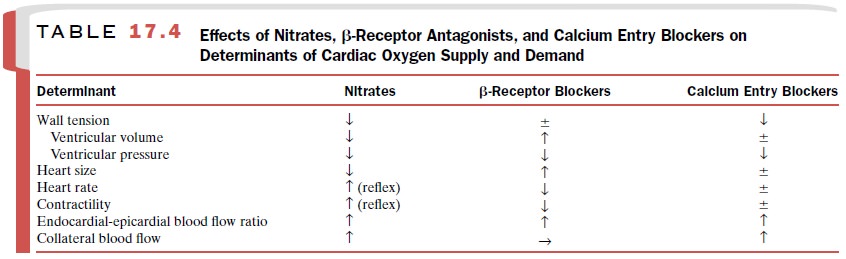
Propranolol and nadolol also have been used suc-cessfully in combination with certain calcium entry blockers, particularly nifedipine, for the treatment of secondary angina. Caution should be used, however, when combining a β-blocker and a calcium channel blocker, such as verapamil or diltiazem, since the nega-tive inotropic and chronotropic effects of this combina-tion may lead to severe bradycardia, arteriovenous nodal block, or decompensated congestive heart failure.
Table 17.3 provide additional
details concerning the most commonly used β-blockers (i.e., propranolol,
nadolol, atenolol, and metoprolol) in the treatment of angina pectoris.
Adverse Effects
Abrupt interruption of
propranolol therapy in individu-als with angina pectoris has been associated
with reap-pearance of angina, acute myocardial infarction, or death due to a
sudden increase in sympathetic nervous system tone to the heart. The mechanisms
underlying these re-actions are unknown, but they may be the result of an
in-crease in the number of β-receptors that occur following chronic β-adrenoceptor blockade (up-regulation of
re-ceptors). When it is advisable to discontinue propranolol administration,
such as before coronary bypass surgery, the dosage should be tapered over 2 to
3 days.
Related Topics