Chapter: Medical Physiology: Circulatory Shock and Physiology of Its Treatment
Shock Caused by Hypovolemia-Hemorrhagic Shock
Shock Caused by Hypovolemia-Hemorrhagic Shock
Hypovolemia means diminished blood volume. Hem-orrhage is the most common cause of hypovolemic shock. Hemorrhage decreases the filling pressure of thecirculation and, as a consequence, decreases venousreturn. As a result, the cardiac output falls below normal, and shock may ensue.
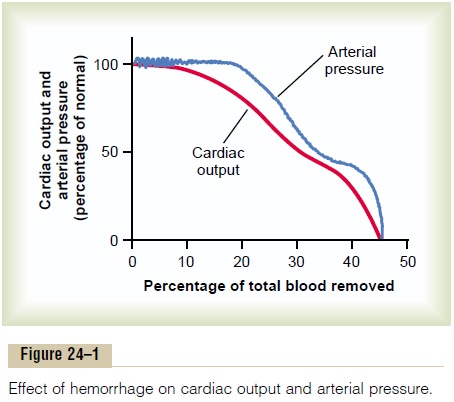
Relationship of Bleeding Volume to Cardiac Output and Arterial Pressure
Figure 24–1 shows the approximate effects on both cardiac output and arterial pressure of removing blood from the circulatory system over a period of about 30 minutes. About 10 per cent of the total blood volume can be removed with almost no effect on either arte-rial pressure or cardiac output, but greater blood loss usually diminishes the cardiac output first and later the arterial pressure, both of which fall to zero when about 35 to 45 per cent of the total blood volume has been removed.
Sympathetic Reflex Compensations in Shock—Their Special Value to Maintain Arterial Pressure. The decrease in arte-rial pressure after hemorrhage—as well as decreases in pressures in the pulmonary arteries and veins in the thorax—causes powerful sympathetic reflexes (initi-ated mainly by the arterial baroreceptors and other vascular stretch receptors).
These reflexes stimulate the sympathetic vasoconstric-tor system throughout the body, resulting in three important effects: (1) The arterioles constrict in most parts of the systemic circulation, thereby increasing the total peripheral resistance. (2) The veins and venous reservoirs constrict, thereby helping to main-tain adequate venous return despite diminished blood volume. (3) Heart activity increases markedly, some-times increasing the heart rate from the normal value of 72 beats/min to as high as 160 to 180 beats/min.
Value of the Sympathetic Nervous Reflexes. In theabsence of the sympathetic reflexes, only 15 to 20 per cent of the blood volume can be removed over a period of 30 minutes before a person dies; this is in contrast to a 30 to 40 per cent loss of blood volume that a person can sustain when the reflexes are intact. Therefore, the reflexes extend the amount of blood loss that can occur without causing death to about twice that which is possible in their absence.
Greater Effect of the Sympathetic Nervous Reflexes in Maintaining Arterial Pressure than in Maintaining Cardiac Output. Referring again to Figure 24–1, notethat the arterial pressure is maintained at or near normal levels in the hemorrhaging person longer than is the cardiac output. The reason for this is that the sympathetic reflexes are geared more for maintaining arterial pressure than for maintaining output. They increase the arterial pressure mainly by increasing the total peripheral resistance, which has no beneficial effect on cardiac output; however, the sympathetic con-striction of the veins is important to keep venous return and cardiac output from falling too much, in additionto their role in maintaining arterial pressure.
Especially interesting is the second plateau occur-ring at about 50 mm Hg in the arterial pressure curve of Figure 24–1. This results from activation of the central nervous system ischemic response, which causes extreme stimulation of the sympathetic nervous system when the brain begins to suffer from lack of oxygen or from excess buildup of carbon dioxide. This effect of the central nervous system ischemic response can be called the “last-ditch stand” of the sympathetic reflexes in their attempt to keep the arterial pressure from falling too low.
Protection of Coronary and Cerebral Blood Flow by the Reflexes. A special value of the maintenanceof normal arterial pressure even in the presence of decreasing cardiac output is protection of blood flow through the coronary and cerebral circulatory systems.
The sympathetic stimulation does not cause significant constriction of either the cerebral or the cardiac vessels. In addition, in both these vascular beds, local blood flow autoregulation is excellent, which prevents moderate decreases in arterial pressure from signifi-cantly decreasing their blood flows. Therefore, blood flow through the heart and brain is maintained essen-tially at normal levels as long as the arterial pressure does not fall below about 70 mm Hg, despite the fact that blood flow in some other areas of the body might be decreased to as little as one third to one quarter normal by this time because of vasoconstriction.
Progressive and Nonprogressive Hemorrhagic Shock
Figure 24–2 shows an experiment that we performed in dogs to demonstrate the effects of different degrees of sudden acute hemorrhage on the subsequent course of arterial pressure. The dogs were bled rapidly until their arterial pressures fell to different levels. Those dogs whose pressures fell immediately to no lower than 45 mm Hg (groups I, II, and III) all eventually recovered; the recovery occurred rapidly if the pres-sure fell only slightly (group I) but occurred slowly if it fell almost to the 45 mm Hg level (group III). When the arterial pressure fell below 45 mm Hg (groups IV, V, and VI), all the dogs died, although many of them hovered between life and death for hours before the circulatory system deteriorated to the stage of death.
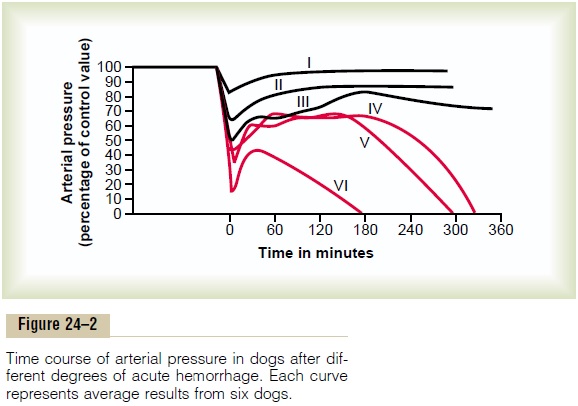
This experiment demonstrates that the circulatory system can recover as long as the degree of hemor-rhage is no greater than a certain critical amount. Crossing this critical threshold by even a few milliliters of blood loss makes the eventual difference between life and death. Thus, hemorrhage beyond a certain crit-ical level causes shock to become progressive. That is, the shock itself causes still more shock, and the condi-tion becomes a vicious circle that eventually leads to deterioration of the circulation and to death.
Nonprogressive Shock—Compensated Shock
If shock is not severe enough to cause its own pro-gression, the person eventually recovers. Therefore, shock of this lesser degree is called nonprogressive shock. It is also called compensated shock,meaningthat the sympathetic reflexes and other factors com-pensate enough to prevent further deterioration of the circulation.
The factors that cause a person to recover from moderate degrees of shock are all the negative feed-back control mechanisms of the circulation that attempt to return cardiac output and arterial pressure back to normal levels. They include the following:
1. Baroreceptor reflexes, which elicit powerfulsympathetic stimulation of the circulation.
2. Central nervous system ischemic response, which elicits even more powerful sympathetic stimulation throughout the body but is not activated significantly until the arterial pressure falls below 50 mm Hg.
3. Reverse stress-relaxation of the circulatory system, which causes the blood vessels to contract around the diminished blood volume, so that the blood volume that is available more adequately fills the circulation.
4. Formation of angiotensin by the kidneys, whichconstricts the peripheral arteries and also causes decreased output of water and salt by the kidneys, both of which help prevent progression of shock.
5. Formation of vasopressin (antidiuretic hormone) by the posterior pituitary gland, which constrictsthe peripheral arteries and veins and greatly increases water retention by the kidneys.
6. Compensatory mechanisms that return the blood volume back toward normal, including absorptionof large quantities of fluid from the intestinal tract, absorption of fluid into the blood capillaries from the interstitial spaces of the body, conservation of water and salt by the kidneys, and increased thirst and increased appetite for salt, which make the person drink water and eat salty foods if able.
The sympathetic reflexes provide immediate help toward bringing about recovery because they become maximally activated within 30 seconds to a minute after hemorrhage.
The angiotensin and vasopressin mechanisms, as well as the reverse stress-relaxation that causes contraction of the blood vessels and venous reservoirs, all require 10 minutes to 1 hour to respond completely, but they aid greatly in increasing the arterial pressure or increasing the circulatory filling pressure and thereby increasing the return of blood to the heart.
Finally, readjustment of blood volume by absorption of fluid from the interstitial spaces and intestinal tract, as well as oral ingestion and absorption of additional quantities of water and salt, may require from 1 to 48 hours, but recovery eventually takes place, provided the shock does not become severe enough to enter the progressive stage.
“Progressive Shock” Is Caused by a Vicious Circle of Cardiovascular Deterioration
Figure 24–3 shows some of the positive feedbacks that further depress cardiac output in shock, thus causing the shock to become progressive. Some of the more important feedbacks are the following.
Cardiac Depression. When the arterial pressure falls lowenough, coronary blood flow decreases below thatrequired for adequate nutrition of the myocardium.
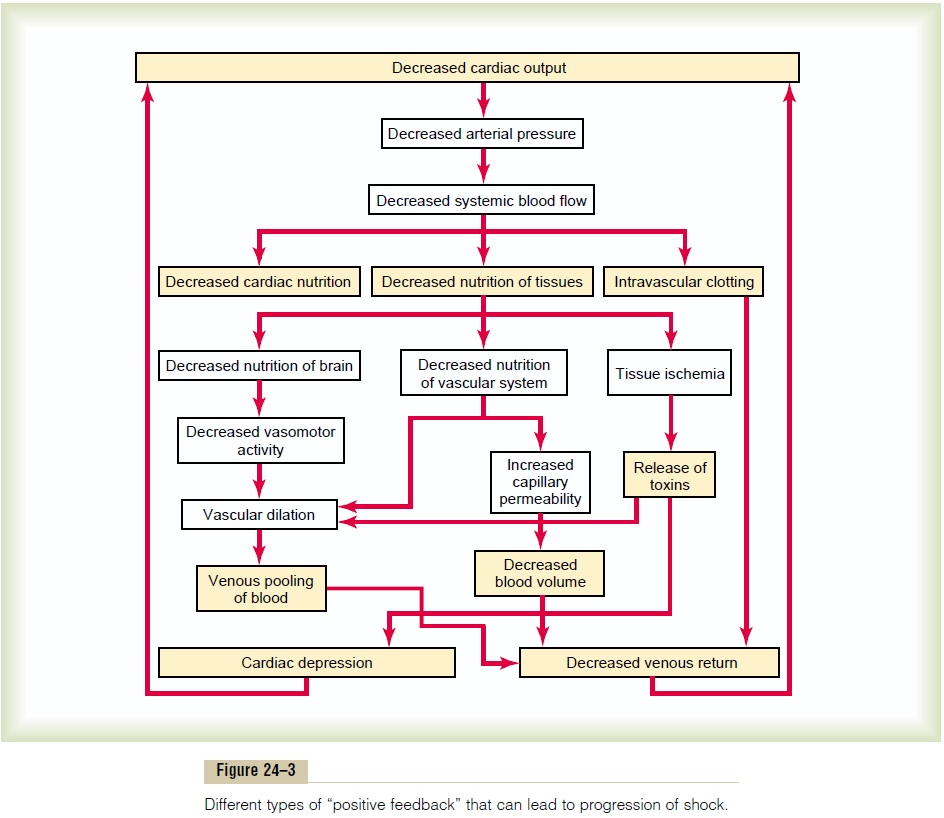
This weakens the heart muscle and thereby decreases the cardiac output more. Thus, a positive feedback cycle has developed, whereby the shock becomes more and more severe.
Figure 24–4 shows cardiac output curves extrapo-lated to the human heart from experiments in dogs, demonstrating progressive deterioration of the heart at different times after the onset of shock. A dog was bled until the arterial pressure fell to 30 mm Hg, and the pressure was held at this level by further bleeding or retransfusion of blood as required. Note from the second curve in the figure that there was little deteri-oration of the heart during the first 2 hours, but by 4 hours, the heart had deteriorated about 40 per cent; then, rapidly, during the last hour of the experiment (after 4 hours of low coronary blood pressure), the heart deteriorated completely.
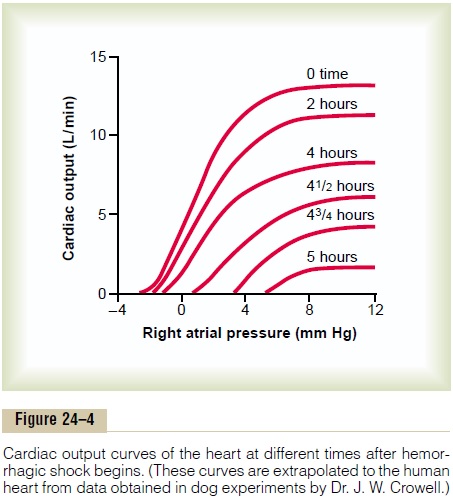
Thus, one of the important features of progressive shock, whether it is hemorrhagic in origin or caused in another way, is eventual progressive deterioration of the heart. In the early stages of shock, this plays very little role in the condition of the person, partly because deterioration of the heart is not severe during the first hour or so of shock, but mainly because the heart has tremendous reserve capability that normally allows it to pump 300 to 400 per cent more blood than is required by the body for adequate bodywide tissue nutrition. In the latest stages of shock, however, dete-rioration of the heart is probably the most important factor in the final lethal progression of the shock.
Vasomotor Failure. In the early stages of shock, variouscirculatory reflexes cause intense activity of the sympathetic nervous system. This, as discussed earlier, helps delay depression of the cardiac output and especially helps prevent decreased arterial pressure. However, there comes a point when diminished blood flow to the brain’s vasomotor center depresses the center so much that it, too, becomes progressively less active and finally totally inactive. For instance, com-plete circulatory arrest to the brain causes, during thefirst 4 to 8 minutes, the most intense of all sympathetic discharges, but by the end of 10 to 15 minutes, the vaso-motor center becomes so depressed that no further evidence of sympathetic discharge can be demon-strated. Fortunately, the vasomotor center usually does not fail in the early stages of shock if the arterial pressure remains above 30 mm Hg.
Blockage of Very Small Vessels—“Sludged Blood.” In time,blockage occurs in many of the very small blood vessels in the circulatory system, and this also causes the shock to progress. The initiating cause of this blockage is sluggish blood flow in the microvessels.
Because tissue metabolism continues despite the low flow, large amounts of acid, both carbonic acid and lactic acid, continue to empty into the local blood vessels and greatly increase the local acidity of the blood. This acid, plus other deterioration products from the ischemic tissues, causes local blood aggluti-nation, resulting in minute blood clots, leading to very small plugs in the small vessels. Even if the vessels do not become plugged, an increased tendency for the blood cells to stick to one another makes it more dif-ficult for blood to flow through the microvasculature, giving rise to the term sludged blood.
Increased Capillary Permeability. After many hours ofcapillary hypoxia and lack of other nutrients, the permeability of the capillaries gradually increases, and large quantities of fluid begin to transude into the tissues. This decreases the blood volume even more, with a resultant further decrease in cardiac output, making the shock still more severe. Capillary hypoxia does not cause increased capillary permeability until the late stages of prolonged shock.
Release of Toxins by Ischemic Tissue. Throughout thehistory of research in the field of shock, it has been suggested that shock causes tissues to release toxic substances, such as histamine, serotonin, and tissue enzymes, that cause further deterioration of the circu-latory system. Quantitative studies have proved the significance of at least one toxin, endotoxin, in some types of shock.
Cardiac Depression Caused by Endotoxin. Endotoxinis released from the bodies of dead gram-negative bacteria in the intestines. Diminished blood flow to the intestines often causes enhanced formation and absorption of this toxic substance. The circulating toxin then causes increased cellular metabolism despite inadequate nutrition of the cells; this has a spe-cific effect on the heart muscle, causing cardiac depres-sion. Endotoxin can play a major role in some typesof shock, especially “septic shock,”.
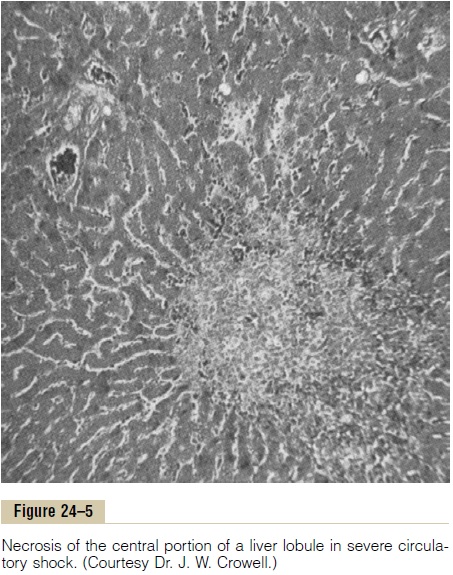
Generalized Cellular Deterioration. As shock becomessevere, many signs of generalized cellular deteriora-tion occur throughout the body. One organ especially affected is the liver, as illustrated in Figure 24–5. This occurs mainly because of lack of enough nutrients to support the normally high rate of metabolism in liver cells, but also partly because of the extreme exposure of the liver cells to any vascular toxin or other abnor-mal metabolic factor occurring in shock.
Among the damaging cellular effects that are known to occur in most body tissues are the following:
1. Active transport of sodium and potassium through the cell membrane is greatly diminished. As a result, sodium and chloride accumulate in the cells, and potassium is lost from the cells. In addition, the cells begin to swell.
2. Mitochondrial activity in the liver cells, as well as in many other tissues of the body, becomes severely depressed.
3. Lysosomes in the cells in widespread tissue areas begin to break open, with intracellular release of hydrolases that cause further intracellulardeterioration.
4. Cellular metabolism of nutrients, such as glucose, eventually becomes greatly depressed in the last stages of shock. The actions of some hormones are depressed as well, including almost 100 per
cent depression of the action of insulin.
All these effects contribute to further deterioration of many organs of the body, including especially (1) the liver, with depression of its many metabolic and detoxification functions; (2) the lungs, with eventual development of pulmonary edema and poor ability to oxygenate the blood; and (3) the heart, thereby further depressing its contractility.
Tissue Necrosis in Severe Shock—Patchy Areas of Necrosis Occur Because of Patchy Blood Flows in Different Organs. Not all cells of the body are equallydamaged by shock, because some tissues have better blood supplies than others. For instance, the cells adja-cent to the arterial ends of capillaries receive better nutrition than cells adjacent to the venous ends of the same capillaries. Therefore, one would expect more nutritive deficiency around the venous ends of capil-laries than elsewhere. This is precisely the effect that Crowell discovered in studying tissue areas in many parts of the body. For instance, Figure 24–5 shows necrosis in the center of a liver lobule, the portion of the lobule that is last to be exposed to the blood as it passes through the liver sinusoids.
Similar punctate lesions occur in heart muscle, although here a definite repetitive pattern, such as occurs in the liver, cannot be demonstrated. Never-theless, the cardiac lesions play an important role in leading to the final irreversible stage of shock. Deteri-orative lesions also occur in the kidneys, especially in the epithelium of the kidney tubules, leading to kidney failure and occasionally uremic death several days later. Deterioration of the lungs also often leads to res-piratory distress and death several days later—called the shock lung syndrome.
Acidosis in Shock. Most metabolic derangements thatoccur in shocked tissue can lead to blood acidosis all through the body. This results from poor delivery of oxygen to the tissues, which greatly diminishes oxida-tive metabolism of the foodstuffs. When this occurs, the cells obtain most of their energy by the anaerobic process of glycolysis, which leads to tremendous quan-tities of excess lactic acid in the blood. In addition, poor blood flow through tissues prevents normal removal of carbon dioxide. The carbon dioxide reacts locally in the cells with water to form high concentrations of intracellular carbonic acid; this, in turn, reacts with various tissue chemicals to form still other intracellu-lar acidic substances. Thus, another deteriorative effect of shock is both generalized and local tissue acidosis, leading to further progression of the shock itself.
Positive Feedback Deterioration of Tissues in Shock and the Vicious Circle of Progressive Shock
All the factors just discussed that can lead to further progression of shock are types of positive feedback. That is, each increase in the degree of shock causes a further increase in the shock.
However, positive feedback does not necessarily lead to a vicious circle. Whether a vicious circle devel-ops depends on the intensity of the positive feedback. In mild degrees of shock, the negative feedback mech-anisms of the circulation—sympathetic reflexes, reverse stress-relaxation mechanism of the blood reservoirs, absorption of fluid into the blood from the interstitial spaces, and others—can easily overcome the positive feedback influences and, therefore, cause recovery. But in severe degrees of shock, the deterio-rative feedback mechanisms become more and more powerful, leading to such rapid deterioration of the circulation that all the normal negative feedback systems of circulatory control acting together cannot return the cardiac output to normal.
Considering once again the principles of positive feedback and vicious circle, one can readily understand why there is a critical cardiac output level above which a person in shock recovers and below which a person enters a vicious circle of cir-culatory deterioration that proceeds until death.
Irreversible Shock
After shock has progressed to a certain stage, transfu-sion or any other type of therapy becomes incapable of saving the person’s life. The person is then said to be in the irreversible stage of shock. Ironically, even in this irreversible stage, therapy can, on rare occasions, return the arterial pressure and even the cardiac output to normal or near normal for short periods, but the circulatory system nevertheless continues to dete-riorate, and death ensues in another few minutes to few hours.
Figure 24–6 demonstrates this effect, showing that transfusion during the irreversible stage can some-times cause the cardiac output (as well as the arterial pressure) to return to normal. However, the cardiac output soon begins to fall again, and subsequent trans-fusions have less and less effect. By this time, multiple deteriorative changes have occurred in the muscle cells of the heart that may not necessarily affect
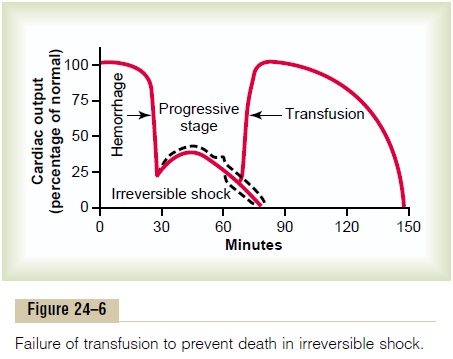
the heart’s immediate ability to pump blood but, over a long period, depress heart pumping enough to cause death. Beyond a certain point, so much tissue damage has occurred, so many destructive enzymes have been released into the body fluids, so much acidosis has developed, and so many other destructive factors are now in progress that even a normal cardiac output for a few minutes cannot reverse the continuing deterio-ration. Therefore, in severe shock, a stage is eventually reached at which the person will die even though vig-orous therapy might still return the cardiac output to normal for short periods.
Depletion of Cellular High-Energy Phosphate Reserves in Irreversible Shock. The high-energy phosphate reservesin the tissues of the body, especially in the liver and the heart, are greatly diminished in severe degrees of shock. Essentially all the creatine phosphate has been degraded, and almost all the adenosine triphosphate has downgraded to adenosine diphosphate, adenosinemonophosphate, and, eventually, adenosine.Thenmuch of this adenosine diffuses out of the cells into the circulating blood and is converted into uric acid, a substance that cannot re-enter the cells to reconstitute the adenosine phosphate system. New adenosine can be synthesized at a rate of only about 2 per cent of the normal cellular amount an hour, meaning that once the high-energy phosphate stores of the cells are depleted, they are difficult to replenish.
Thus, one of the most devastating end results of deterioration in shock, and the one that is perhaps most significant for development of the final state of irreversibility, is this cellular depletion of these high-energy compounds.
Hypovolemic Shock Caused by Plasma Loss
Loss of plasma from the circulatory system, even without loss of red blood cells, can sometimes be severe enough to reduce the total blood volume markedly, causing typical hypovolemic shock similar in almost all details to that caused by hemorrhage. Severe plasma loss occurs in the following conditions:
1. Intestinal obstruction is often a cause of severelyreduced plasma volume. Distention of the intestine in intestinal obstruction partly blocks venous blood flow in the intestinal walls, which increases intestinal capillary pressure. This in turn causes fluid to leak from the capillaries into the intestinal walls and also into the intestinal lumen. Because the lost fluid has a high protein content, the result is reduced total blood plasma protein as well as reduced plasma volume.
2. In almost all patients who have severe burns or other denuding conditions of the skin, so much plasma is lost through the denuded skin areas that the plasma volume becomes markedly reduced.
The hypovolemic shock that results from plasma loss has almost the same characteristics as the shock caused by hemorrhage, except for one additional com-plicating factor: the blood viscosity increases greatly as a result of increased red blood cell concentration in the remaining blood, and this exacerbates the slug-gishness of blood flow.
Loss of fluid from all fluid compartments of the body is called dehydration; this, too, can reduce the blood volume and cause hypovolemic shock similar to that resulting from hemorrhage. Some of the causes of this type of shock are (1) excessive sweating, (2) fluid loss in severe diarrhea or vomiting, (3) excess loss of fluid by nephrotic kidneys, (4) inadequate intake of fluid and electrolytes, or (5) destruction of the adrenal cortices, with loss of aldosterone secretion and conse-quent failure of the kidneys to reabsorb sodium, chloride, and water, which occurs in the absence of the adrenocortical hormone aldosterone.
Hypovolemic Shock Caused by Trauma
One of the most common causes of circulatory shock is trauma to the body. Often the shock results simply from hemorrhage caused by the trauma, but it can also occur even without hemorrhage, because extensive contusion of the body can damage the capillaries sufficiently to allow excessive loss of plasma into the tissues. This results in greatly reduced plasma volume, with resultant hypovolemic shock.
Various attempts have been made to implicate toxic factors released by the traumatized tissues as one of the causes of shock after trauma. However, cross-transfusion experiments into normal animals have failed to show significant toxic elements.
In summary, traumatic shock seems to result mainly from hypovolemia, although there might also be a moderate degree of concomitant neurogenic shock caused by loss of vasomotor tone, as discussed next.
Related Topics