Chapter: Clinical Dermatology: Infestations
Scabies
Scabies
Cause
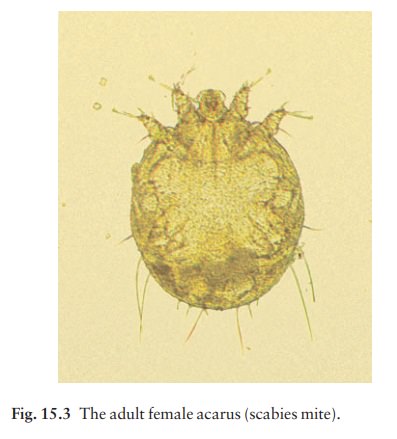
Scabies is caused by the mite Sarcoptes scabiei var. hominis (Fig. 15.3).
Adult mites are 0.3– 0.4 mm long and
therefore just visible, although hard to see except through a lens. It is now
well established that the mites are transferred from person to person by close
bodily contact and not via inanimate objects.
Once
on the skin, fertilized female mites burrow through the stratum corneum at the
rate of about 2 mm per day, and produce two or three oval eggs each day. These
turn into sexually mature mites in 2–3 weeks. The number of mites varies from
case to case, from less than 10 in a clean adult to many more in an unwashed
child. The generalized eruption of scabies, and its itchiness, are thought to
be caused by a sensit-ization to the mites or their products.
Epidemiology
The
prevalence of scabies in many populations rises and falls cyclically, peaking
every 15–20 years. The idea of ‘herd immunity’ has been put forward to explain
this, spread being most easy when a new generation of susceptible individuals
has arisen.
Presentation
For the first 4 – 6 weeks after infestation there may be no itching, but thereafter pruritus dominates the picture, often affecting several people and being par-ticularly severe at night.
The
most dramatic part of the eruptionaexcoriated, eczematized or urticarial
papulesais usually on the trunk, but these changes are non-specific and a
burrow has to be identified to confirm the diagnosis (Fig. 15.4).
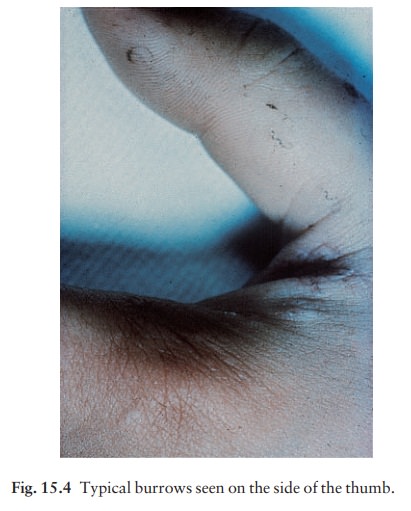
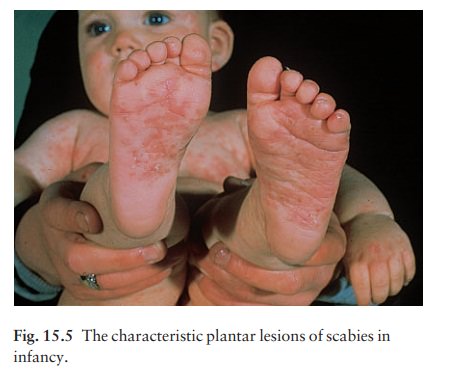
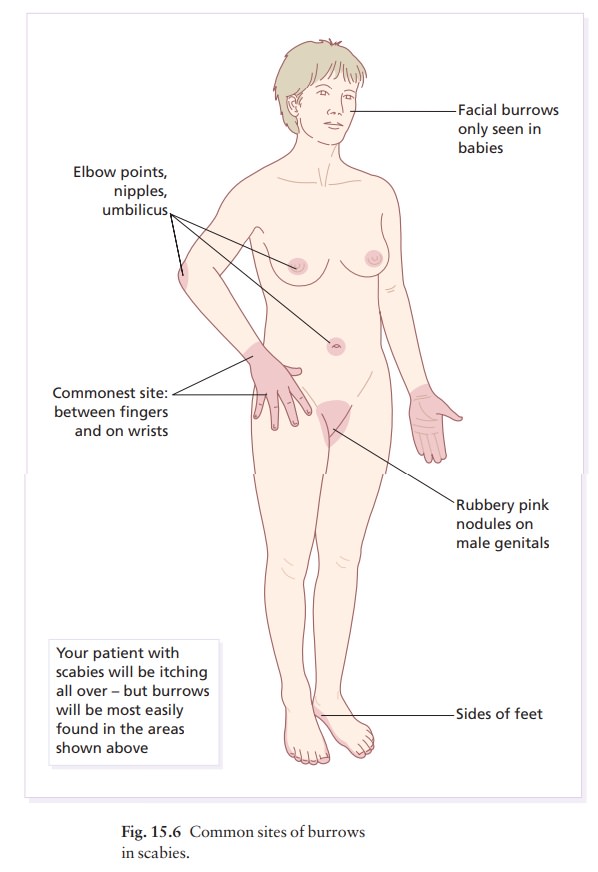
Most
burrows lie on the sides of the fingers, finger webs, sides of the hand and on
the flexural aspects of the wrists. Other favourite sites include the elbows,
ankles and feet (especially in infants; Fig. 15.5), nipples and genitals (Fig.
15.6). Only in infancy does scabies affect the face. Burrows are easily missed
grey-white
The acarus may be seen through a
lens as a small dark dot at the most recent least scaly end of the burrow. With
experience it can be removed for microsco-pic confirmation. On the genitals,
burrows are associated with erythematous rubbery nodules (Fig. 15.7).

Course
Scabies
persists indefinitely unless treated. In the chronic stage, the number of mites
may be small and diagnosis is correspondingly difficult. Relapses after
apparently adequate treatment are common and can be put down to reinfestation
from undetected and untreated contacts.
Complications
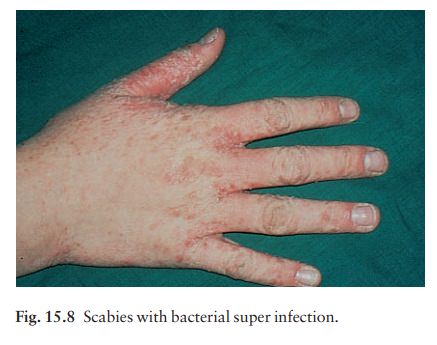
•
Secondary infection, with
pustulation, is common (Fig. 15.8). Rarely, glomerulonephritis follows this.
•
Repeated applications of scabicides
can cause skin irritation and eczema.
Persistent itchy red nodules may remain on the gen-itals or armpits of children for some months after ade-quate treatment.
•
Venereal disease may be acquired at
the same time as scabies.
•
Crusted (Norwegian) scabies, which
may not be itchy, is a widespread crusted eruption in which vast numbers of
mites are found. It affects people with learning difficulties or the
immunosuppressed, and can be the unsuspected source of epidemics of ordinary
scabies.
Differential diagnosis
Only
scabies shows characteristic burrows. Animal scabies from pets induces an itchy
rash in humans but this lacks burrows. The lesions of papular urticaria are excoriated papules, in groups, mainly on
the legs. Late-onset atopic eczema, cholinergic urticaria, lichen planus,
neurotic exco-riations and dermatitis
herpetiformis have their own distinctive features. Fibreglass can also cause
epidemics of itching.
Investigations
With
practice an acarus can be picked neatly with a needle from the end of its
burrow and identified microscopically; failing this, eggs and mites can be seen
microscopically in burrow scrapings mounted in potassium hydroxide or mineral oil. Some find dermatoscopy a
quick and reliable way to identify the mite.
Treatment
•
Use an effective scabicide; there
are many on the market now (Formulary 1). In the UK, the preferred treatment is
with malathion or permethrin; lindane is no longer available. Topical treatment
plus ivermectin (on a named patient basis in the UK), in a single dose of 200
µg/kg by mouth, is effective for Norwegian scabies and scabies that does not
respond to topical measures alone.
•
For babies over 2 months, toddlers
and young children we advise permethrin cream, 25% benzyl benzoate emulsion
diluted with three parts of water, or 6% precipitated sulphur in white soft
paraffin (petrolatum).
•
It is still not clear which
scabicides can be safely used to treat pregnant women or those who are
breast-feeding. Despite the absence of convincing evidence that unborn children
can be damaged by topical scabicides, we prefer to use the same measures that
we use to treat babies (above).
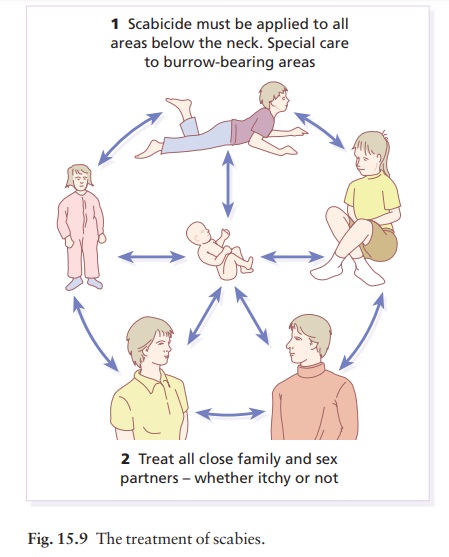
•
Do not just treat the patient: treat
all members of the family and sexual contacts, whether they are itching or not
(Fig. 15.9).
•
Have a printed sheet to give to the
patient and go through it with themascabies victims are notoriously confused.
•
One convenient way to apply
scabicides to the skin is with a 5 cm (2 inch) paintbrush. The number of
applications recommended varies from dermatologist to dermatologist. There is
no doubt that some pre-parations, such as malathion, disappear quickly from the
skin, leaving it vulnerable to any mites which hatch out from eggs that have
survived. A second application, a week after the first, is then essential. With
permethrin, this may be less important. The main reason for recommending a
second application is that it will cover areas left out during an inefficient
first application.
•
Make sure that patients grasp the
fact that scabic-ides have to be applied to all areas of skin below the jaw
line, including the genitals, soles of the feet, and skin under the free edge
of the nails. If the hands are washed, the scabicide should be reapplied. A hot
bath before treatment is no longer recommended.
•
Ordinary laundering deals
satisfactorily with cloth-ing and sheets. Mites die in clothing unworn for 1
week.
•
Residual itching may last for
several days, or even a few weeks, but this does not need further applications
of the scabicide. Rely instead on calamine lotion or crotamiton.
Related Topics