Chapter: Clinical Dermatology: Physical forms of treatment
Phototherapy - Physical forms of treatment
Phototherapy
Ultraviolet
radiation (UVR) helps some conditions (e.g. psoriasis, atopic dermatitis,
nummular eczema, parapsoriasis, pityriasis lichenoides, pityriasis rosea, acne
and cutaneous T-cell lymphoma; Table 16.4). For psoriasis, UVB may be given up to three times weekly, for
3–8 weeks, on its own or com
After tests to establish a starting dose, irradiance is increased by small
increments, aiming to produce minimal ery-thema only after 24 h. Ultraviolet A
is combined with psoralens in PUVA treatment. Close supervi-sion is needed
because extreme phototoxicity from an overdose, from sunlight or concomitant
use of tanning booths, has produced severe burns and even death. A careful
record should also be kept of the cumulative UVR dose as the risk of developing
skin cancers, including malignant melanoma, is increased when a patient has
received a large cumulative dose.
Photodynamic therapy
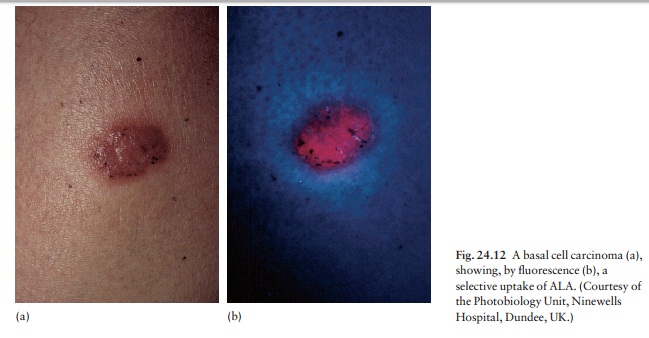
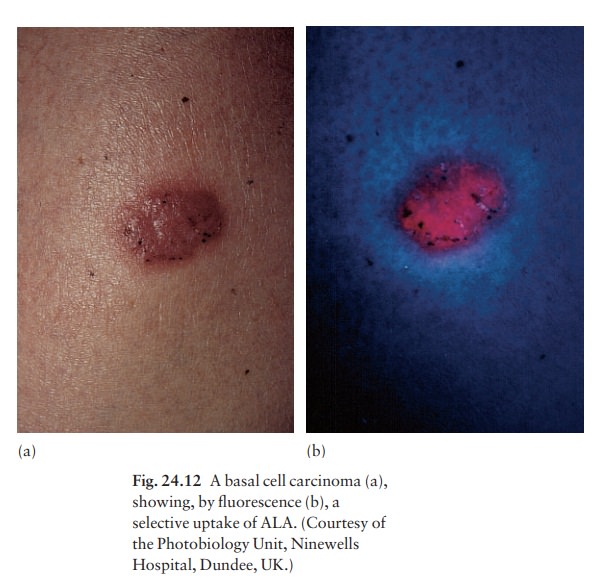
Photodynamic therapy (PDT) is a new form of photo-therapy used for skin cancers and precancers such as superficial basal cell carcinoma less than 2 mm thick), intraepidermal carcinoma, erythro-plasia of Queyrat and actinic keratoses. Selective tumour destruction is achieved by incorporating the photosensitizer in the target (malig-nant) tissue and then activating it with either a laser or non-laser light source. A promising combination is the naturally occurring porphyrin precursor, amino-laevulinic acid (ALA) and irradiation with a red light. The water-soluble ALA (20% in Unguentum M) is applied topically, under occlusion, to the tumour. After 4 h or so, when the ALA has been selectively absorbed by the tumour (Fig. 24.12), the area is exposed to the light for 15–60 min. The activated ALA converts molecular oxygen to cytotoxic sing-let oxygen and free radicals, which in turn cause ischaemic necrosis of the tumour by damaging cell membranes, especially those in the walls of blood ves-sels.
PDT is carried out in an outpatient setting and its potential advantages over standard treatments include:
•
non-invasiveness;
•
ability to treat many lesions at
once;
•
rarely causes ulceration and leads
to a good cos-metic result;
•
good patient acceptability; and
useful
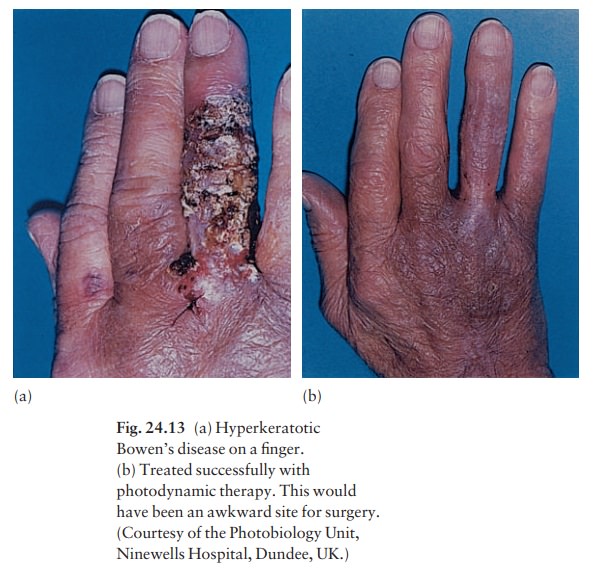
for treating tumours on sites that present sur-gical difficulty, e.g. the taut
skin of the finger (Fig. 24.13)
Related Topics