Chapter: Obstetrics and Gynecology: Infertility
Male Infertility
MALE INFERTILITY
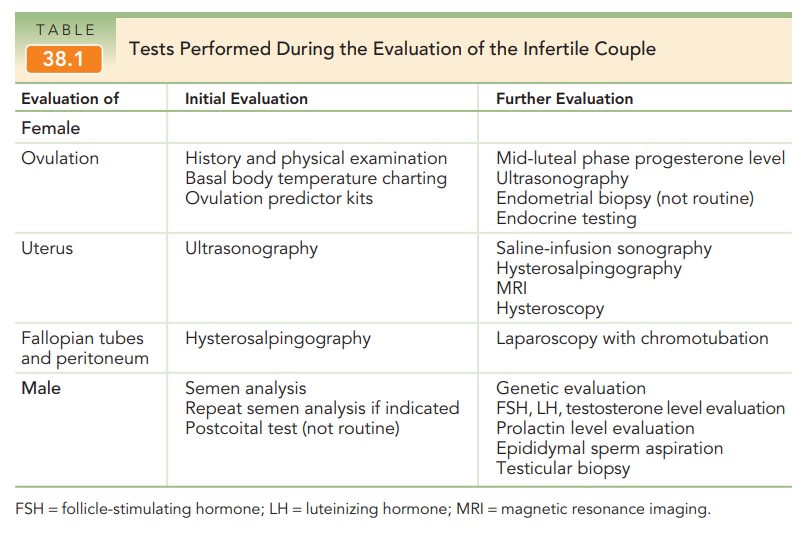
Because male infertility is
common, it is important to also perform a semen
analysis when initiating evaluation of the female partner. The semen
specimen is usually obtained by masturbation after 2 to 3 days of abstinence;
frequent ejac-ulation may lower the sperm concentration. It is important to
collect the entire ejaculate, because the first part contains the greatest
density of sperm. Analysis of the specimen should be performed within 1 hour of
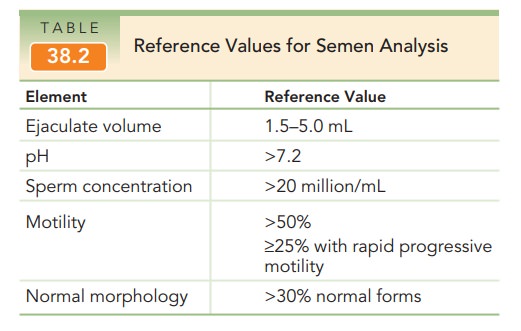
ejaculation (see Table 38.1). The standard semen analysis evaluates the
quantity and quality of seminal fluid, sperm concentra-tion, and sperm motility
and morphology. Normal semen measurements have been established by the World
Health Organization (Table 38.2). A normal semen analysis excludes a male cause
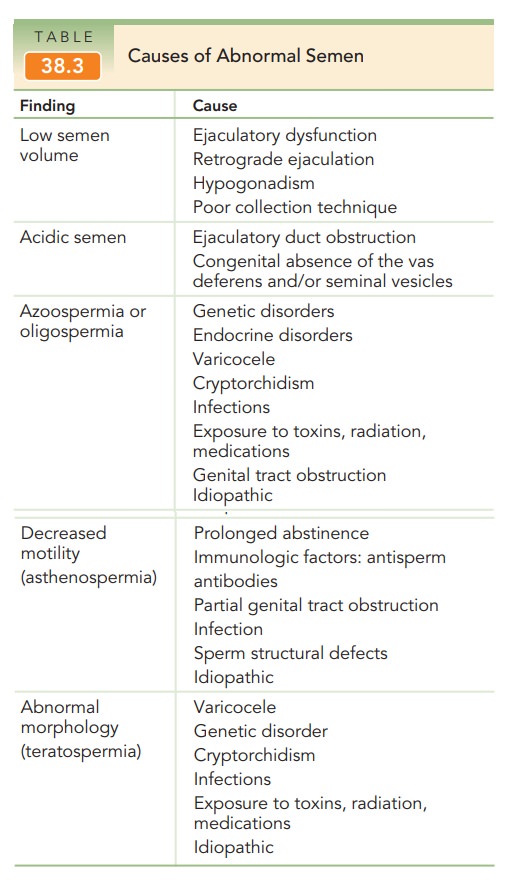
for infertility in more than 90% of heterosexual couples. Certain abnormalities
identified by the semen analysis are associated with specific etiologies of
male infertility (Table 38.3). Sperm function can be further evaluated with specialized
diagnostic tests, but these tests are not routinely used.
Besides the semen analysis, the postcoital test has historically been
used to evaluate sperm concentration and their interaction with the cervical
mucus. To perform this test, a sample of cervical mucus must be obtained 2 to
12 hours after intercourse that occurs 1 to 3 days prior to ovulation. The
sample is placed on a glass slide and exam-ined under a microscope. Standard
criteria include the presence of at least 5 motile sperm per high-powered
field. However, the diagnostic utility and validity of this test is limited;
thus, its routine use is not indicated. Furthermore, conventional fertility
treatments such as intrauterine insem-ination and in vitro fertilization (IVF)
bypass any abnormal-ities of the cervix or cervical mucus.
If the results of the semen analysis are abnormal, it should be repeated in 1 to 2 weeks. Persistent abnormali-ties in the semen necessitate further investigation. The male partner should be evaluated by a urologist or repro-ductive endocrinologist who specializes in male infertility. Occasionally, male infertility may be the presenting sign of a serious medical condition, such as testicular cancer or a pituitary tumor. Etiologies of male infertility include con-genital, acquired, or systemic disorders that can be grouped into the following categories: hypothalamic-pituitary disease that causes gonadal dysfunction (1% to 2%), testic-ular disease (30% to 40%), post-testicular defects that cause disorders of sperm transport or ejaculation (10% to 20%), and unexplained infertility (40% to 50%).
Abnormalities
in spermatogenesis are a major cause of male infertility. Unlike
oocytes, which undergo development ina cyclic fashion, sperm are being produced
constantly by the testes. As sperm develop within the germinal epithe-lium of
the testis, they are released into the epididymis where maturation occurs before
ejaculation.
Sperm
production and development takes approximately 70 days. Therefore, abnormal
results of the semen analysis reflect events that occurred more than 2 months
before the specimen collection.
Alternatively, a minimum of 70
days is required to observe changes in sperm production following initiation of
any therapy.
Further evaluation of the
infertile male includes endocrine and genetic testing. Endocrine evaluation is
appropriate for individuals with abnormal sperm concentra-tions or signs of
androgen deficiency. Serum testosterone, FSH, and LH levels will identify
primary hypogonadism (low testosterone, or elevated FSH and LH) or secondary
hypogonadism (low testosterone, FSH, and LH). A low LH level in the presence of
oligospermia (sperm concentration
less than 5 million/mL) and a normal testosterone level may indicate exogenous
steroid use. A serum prolactin level
should be assessed in men with low testosterone levels.
Genetic
abnormalities may affect sperm production or trans-port. Genetic testingis
indicated in men withazoospermia(no
sperm) and severe oligospermia. The most common abnormalities identified
include gene mutations in the cys-tic fibrosis transmembrane conductase
regulator (CFTR), somatic and sex chromosome abnormalities, and micro-deletions
of the Y chromosome. Men with mutations in one or both copies of the CFTR gene
often exhibit congenital bilateral absence of the vas deferens or other
obstructive defects, and many have no pulmonary symptoms. A karyo-type may
reveal abnormalities, such as Klinefelter syndrome (47 XXY) or chromosome
inversions and translocations. Special testing must be performed to search for
Y chromo-some microdeletions, because they are not detected by rou-tine
karyotype analysis; these microdeletions are associated with altered testicular
development and spermatogenesis. If a genetic condition is identified, genetic
counseling is strongly recommended.
Men with azoospermia can be
further evaluated by two diagnostic procedures. If an obstructive process is suspected
(obstructive azoospermia), then sperm should accumu-late just before the
obstruction. For example, men with congenital absence of the vas deferens or
those who underwent a vasectomy have a swollen epididymis where constant
production of sperm results in a small collection. Percutaneous epididymal sperm aspiration (PESA) or microsurgical epididymal sperm aspiration
(MESA) procedures can retrieve motile, healthy sperm. If no obstruc-tion is
present (nonobstructive azoospermia) and a testicu-lar abnormality is
suspected, a testicular biopsy may identify a few sperm present in the
seminiferous tubules. With either procedure, small numbers of sperm are
obtained compared to a normal ejaculated specimen. These retrieved sperm can be
used to try to achieve pregnancy; however, the female partner must undergo IVF,
and a single sperm is used to fertilize a singe oocyte (intracytoplasmic sperm
injection).
Related Topics