Chapter: Pathology: Cardiac Pathology
Ischemic Heart Disease
ISCHEMIC HEART DISEASE
Cardiac
ischemia is usually secondary to coronary artery disease (CAD); it is
themost common cause of death in the United States. It is most often seen in
middle-age men and postmenopausal women.
Angina
pectoris is due to transient cardiac ischemia without cell death
resulting insubsternal chest pain.
·
Stable
angina (most common type) is caused by coronary artery
atheroscle-rosis with luminal narrowing >75%. Chest pain is brought on by
increased cardiac demand (exertional or emotional), and is relieved by rest or
nitroglyc-erin (vasodilation). Electrocardiogram shows ST segment depression
(suben-docardial ischemia).
·
Prinzmetal
variant angina
is caused by coronary artery vasospasm and produces episodic
chest pain often at rest; it is relieved by nitroglycerin (vasodilatation).
Electrocardiogram shows transient ST segment elevation (transmural ischemia).
·
Unstable
or crescendo angina is caused by formation of a
nonocclusive throm-bus in an area of coronary atherosclerosis, and is
characterized by increasing frequency, intensity, and duration of episodes;
episodes typically occur at rest. This form of angina has a high risk for
myocardial infarction.
Myocardial
infarction (MI) occurs when a localized area of cardiac muscle
undergoescoagulative necrosis due to ischemia. It is the most common cause of
death in the United States. The mechanism leading to infarction is coronary
artery atheroscle-rosis (90% of cases). Other causes include decreased
circulatory volume, decreased oxygenation, decreased oxygen-carrying capacity,
or increased cardiac workload, due to systemic hypertension, for instance.
·
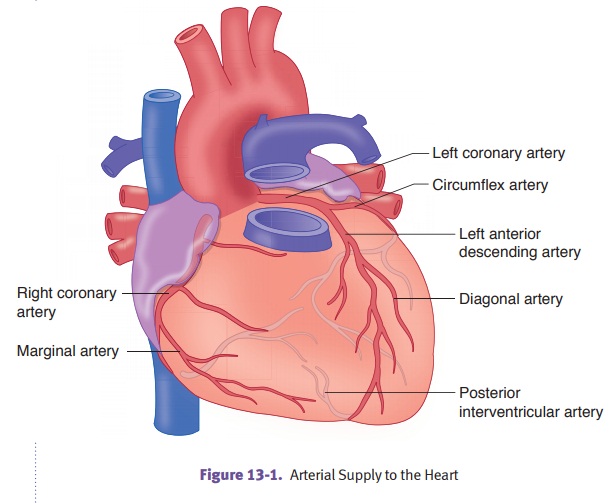
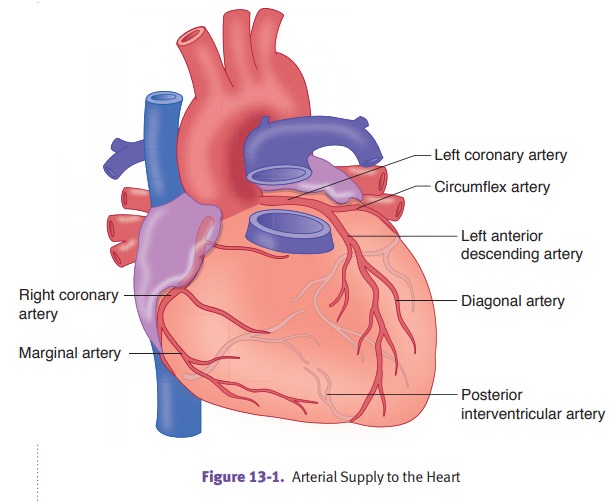
Distribution
of coronary artery thrombosis.The left anterior descendingartery
(LAD) is involved in 45% of cases; the right coronary artery (RCA) is involved
in 35% of cases; and the left circumflex coronary artery (LCA) is involved in
15% of cases.
Infarctions
are classified as transmural, subendocardial, or microscopic.
·
Transmural
infarction (most common type) is considered to have
occurredwhen ischemic necrosis involves >50% of myocardial wall. It is
associated with regional vascular occlusion by thrombus. It causes ST elevated
MIs (STEMIs) due to atherosclerosis and acute thromobosis.
·
Subendocardial
infarction is considered to have occurred when
ischemicnecrosis involves <50% of myocardial wall. It is associated with
hypoperfu-sion due to shock. ECG changes are not noted. This type of infarction
occurs in a setting of coronary artery disease with a decrease in oxygen
delivery or an increase in demand.
·
Microscopic
infarction is caused by small vessel occlusion due to
vasculitis,emboli, or spasm. ECG changes are not noted.
The
clinical presentation of MI is classically a sudden onset of severe “crushing”
substernal chest pain that radiates to the left arm, jaw, and neck. The pain
may be accompanied by chest heaviness, tightness, and shortness of breath;
diaphoresis, nausea, and vomiting; jugular venous distension (JVD); anxiety and
often “feeling of impending doom.” Electrocardiogram initially shows ST segment
elevation. Q waves representing myocardial coagulative necrosis develop in
24–48 hours.
·
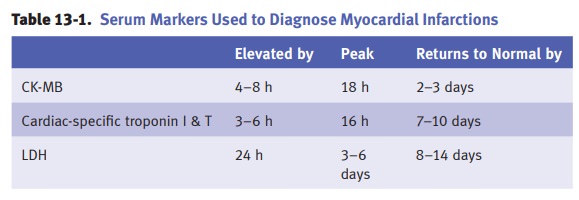
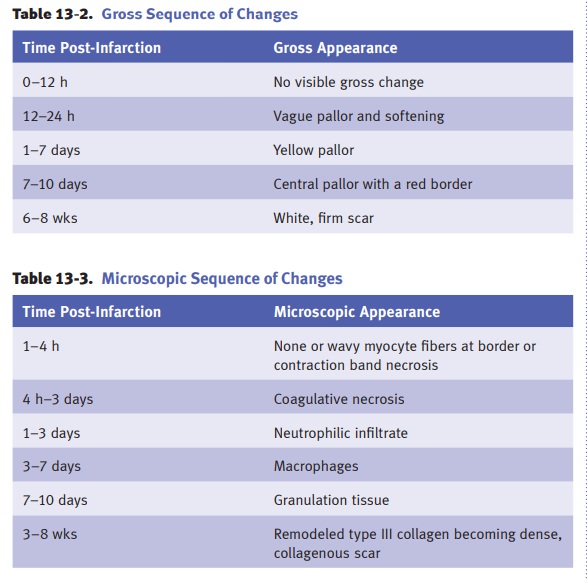
Gross
and microscopic sequence of changes.The
microscopic and grosschanges represent a spectrum that is preceded by
biochemical changes going from aerobic metabolism to anaerobic metabolism
within minutes. The time intervals are variable and depend on the size of the
infarct, as well as other factors.
Complications
of MI include cardiac arrhythmias that may lead to sudden car-diac death;
congestive heart failure; cardiogenic shock (>40–50% myocardium is
necrotic); mural thrombus and thromboembolism; fibrinous pericarditis;
ventricu-lar aneurysm; and cardiac rupture. Cardiac rupture most commonly
occurs 3–7 days after MI, and has effects that vary with the site of rupture:
ventricular free wall rupture causes cardiac tamponade; interventricular septum
rupture causes left to right shunt; and papillary muscle rupture causes mitral
insufficiency.
Sudden cardiac death is
defined to be death within 1 hour of the onset of symp-toms. The mechanism is
typically a fatal cardiac arrhythmia (usually ventricular fibrillation).
Coronary
artery disease is the most common underlying cause (80%); other causes include
hypertrophic cardiomyopathy, mitral valve prolapse, aortic valve stenosis,
congenital heart abnormalities, and myocarditis.
Chronic
ischemic heart disease is the insidious onset of
progressive congestive heartfailure. It is characterized by left ventricular
dilation due to accumulated ischemic myocardial damage (replacement fibrosis)
and functional loss of hypertrophied non-infarcted cardiac myocytes.
Related Topics